Introduction
It has been over 30 years since Erl Pettman introduced the ‘Quadrant Approach’ for assessment and treatment of musculoskeletal disorders (Pettman 1981, 1984). This approach considered how non-optimal movement patterns, or biomechanics, of the thorax contributed to a wide variety of pain states and altered function of the neck, jaw, low back, shoulder girdle, upper and lower extremities. Pettman’s Quadrant Approach inspired the clinical enquiry that continues today of the role of the thorax in multiple conditions. Many Canadian physiotherapists have contributed to the clinical knowledge and expertise I will highlight in this article including Carol Kennedy, Janet Lowcock, Erl Pettman, Cliff Fowler, John Oldham, Laurie McLaughlin, Linda-Joy Lee and Diane Lee. Today, we understand that the thorax is part of many integrated systems including the musculoskeletal, respiratory, cardiac, digestive and urogynecological.
Integrated Systems
Understanding the relationships between, and within, integrated systems and the consequences of impaired function of one on another is complex. Many health practitioners specialize in varying aspects of thorax disorders including physiotherapists, orthopaedic manual therapists, pelvic floor therapists, massage therapists, respiratory therapists and respirologists, cardiac physiotherapists, cardiologists, and exercise physiologists and treatment is often based on the practitioner’s training and experience. The thorax is not only an integrated system within itself (i.e. comprised of many differentiated yet linked parts (Siegel 2010)) but is also integrated as part of the whole body/person. Therefore, understanding what comprises optimal function and how to assess and manage the thorax is fundamental to all forms of treatment for multiple conditions.
Research
Surprisingly, there is limited research on both the biomechanics of the thorax and its contribution to multiple pain states and conditions. This is perhaps due to the perception that it is a very stable structure or to the belief that thoracic pain and impairment are not as prevalent as neck, shoulder or low back pain. Furthermore, the rib cage and the 13 joints per typical thoracic ring (Lee 1994) pose significant methodological challenges for investigating segmental (inter and intra-ring) biomechanics. Many of the ex vivo studies investigating mobility and/or stability of a thoracic ring use cadaveric specimens without an intact rib cage, and while this is occasionally seen in clinical practice (rib removal), it is not the most common clinical presentation. Consequently, these studies are limited for application to clinical practice.
The Biomechanical Model
In 1993 a clinical model of in vivo biomechanics of the thorax was proposed (Lee 1993). This biomechanical model was derived from clinical observations with consideration of the available evidence. In 2014, I was invited to prepare an update article on the biomechanics of the thorax for the Journal of Manual and Manipulative Therapy (Lee 2015) and for this I conducted a literature search of all published studies from 1993 to 2014 to see if any research evidence could clarify, validate or negate the model proposed in 1993. To date, there are no studies that have been able to investigate in vivo segmental, inter-ring (between two adjacent thoracic rings) biomechanics. Sizer et al (2007) noted that “In vivo studies are clinically applicable but lead to challenges in controlling extraneous variables that include motor and postural control, as well as tissue adaptation anatomical and circadian variability; applied preload forces the degree of thoracic kyphosis and scoliosis; and technical difficulty in measuring spinal coupling.” However, this is clinical reality and practitioners are expected to interpret movement behavior with these variables in situ. They conclude with “The lack of a common coupling pattern may merit individual clinical assessment for each patient examined”.
- How should clinicians interpret the movement findings of the thorax noted on assessment?
- What are the normal, or optimal, biomechanics for the thorax?
- What is abnormal?
To date, the highest ranked level of evidence (a systematic review (Sizer et al 2007)) does not provide clinicians with a biomechanical model against which to compare the patient’s movement results. So, while it is acknowledged that the thorax plays a key role in optimal function of the trunk (including the head and neck), upper and lower extremities, respiration, digestion, and continence we still rely on clinical models of proposed alignment (posture), biomechanics and control for assessment and management of the thorax in multiple pain states and conditions.
I’ve been asked to include in this article a summary of what a thorough assessment of the thorax should include and how clinicians can determine if the thorax is contributing to the individual patient’s presenting complaint/condition.
Is the thorax contributing to your patient’s presentation?
Assessment of the thorax follows the same fundamental principles for assessment of any other region of the body. The essential examination includes both subjective and objective components and then clinical reasoning of the examination findings to formulate an individualized treatment plan.
Hearing the story and how it is told – the subjective examination
Assessment begins not only by learning the details of the patient’s story (onset of symptoms, timeline of events, aggravating and relieving activities, presence of any macro or microtrauma, medical considerations etc.) but actually hearing how the story is told. This helps to identify any emotional (fears, anger, anxiety) barriers that may need to be addressed. Asking the patient what they believe to be the problem provides information on their cognitive beliefs (memories of past experiences of self or others, consideration of what other health practitioners have told them) that can potentially provide barriers to recovery. The meaningful complaint (the symptom that the patient is going to use to determine ‘Am I better?’) is derived from hearing their story, as is the meaningful task. Meaningful tasks are those that aggravate the meaningful complaint, or tasks that the patient would like to be able to do better (e.g. sit without pain, run, elevate their arm, turn their head, not leak when they cough etc.). So, now you know what is bothering them and what they are unable to do. How does this direct what to assess? Specifically, how does this information help to guide the examination to determine if the thorax requires treatment?
What tests to include in the assessment – objective examination
The specific tests that comprise the individual objective examination are directed by key findings from the story, or the subjective examination. Neurological tests for conduction/reflexes and neural/dural mobility are done IF the story suggests there has been possible compromise or irritation of the structures inside the spinal canal.
Subsequently, screening tasks are chosen based on how they specifically relate to the patient’s meaningful task(s) and goals.
For example:
If the meaningful task is to be able to sit and work on the computer without pelvic girdle pain (PGP), then the following screening tasks would be pertinent to include in the objective examination:
- Sitting posture in a similar chair that brings on the PGP and the squat task to evaluate how they got into the chair.
- Seated bilateral arm elevation just to the level that they need to manipulate the keys on the keyboard (simulating computer work).
If the meaningful task is to be able to put a box on a high shelf without impingement pain in the right glenohumeral joint, then the following screening tasks would be more relevant to assess:
- Standing unilateral full arm elevation (initially right arm (if right hand dominant) followed by left arm reaching up and across the chest to the bottom of a box).
- Head and neck extension (to look up to the shelf) in isolation then followed by head and neck extension combined with arm elevation.
If the meaningful task is to be able to run without urinary leakage, none of the previous screening tests would be appropriate. Relevant screening tasks for the thorax for running would include:
- Standing step forward – initiated by the left and right lower extremities.
- Standing thoracic rotation without and then with arm elevation to 30 degrees (simulating the arm and thorax action required for optimal running biomechanics).
- Thoracic rotation in step forward lunge position.
For each of these screening tasks, the starting position of the individual thoracic rings (posture and alignment) is determined to facilitate valid interpretation of the task findings. Subsequently, the task is performed and the behavior (alignment, biomechanics and control) of each thoracic ring is assessed (manual palpation and visual observation).
To interpret the findings, one needs to have an understanding of what is required of that specific thoracic ring for that task. Should it move, and how should it move (active mobility testing for that task) or should it not move (motion control testing)? If it does not move when it should or if it moves when it should not then this thoracic ring is behaving in a non-optimal manner for the task being assessed and further tests are required to determine if the non-optimal thoracic ring alignment, biomechanics and/or control are relevant to the clinical picture.
The entire thorax can be screened quite quickly during this initial scan to determine which segmental thoracic ring(s) require further testing.
Is the non-optimal behavior of a thoracic ring clinically relevant?
Subsequent tests for the thoracic ring(s) that demonstrate non-optimal alignment, biomechanics and/or control for the screening task include:
- Passive mobility testing of the integrated thoracic ring
- Can the starting position of the thoracic ring be manually corrected (Lee 2003)? If so, this rules out an articular system impairment such as fibrosis or fixation.
- Does the manual correction of the thoracic ring alignment, combined with facilitation of the requisite biomechanics and control (active assisted range of motion) for the task being assessed improve the
- performance of the task (measured by an increase in range of motion, strength and other functional considerations) and/or the
- patient’s experience of the task (reduction in symptoms, ease of performance, sense of ‘wow- what did you do!’)?
- Once the specific thoracic ring(s) is found which when corrected result in the best improvement in both performance and experience of the screening task, assessment of the four systems (articular, neural, myofascial and possibly visceral) that can potentially create non-optimal alignment, biomechanics and/or control of the specific thoracic ring(s) is done. Which system is assessed depends on the specific ‘vector’ felt on both correction and release of the thoracic ring. Space constraints prevents a complete description of all four systems in this article but to clarify the fundamentals of this part of the assessment let’s consider the difference in the behavior of a thoracic ring that is impacted by a stiff joint (articular system impairment) versus a joint that is compressed by over-activation of specific fascicles of the long muscles of the trunk (neural system impairment).
- Articular system impairments (i.e. fibrosis, joint fixation) do not permit the thoracic ring to be manually corrected and no improvement in the screening task results until mobility of the impaired joint(s) of the thoracic ring is restored. When an attempt is made to manually correct this thoracic ring marked resistance is felt; the ‘beginning and end feel’ of motion is very hard. Specific passive arthrokinematic joint mobility tests for the relevant zygapophyseal and costotransverse joints are required to determine the underlying impairment(s). These findings then direct treatment. When there is a history of trauma to the thorax specific intra and inter-ring stability tests should be performed to rule in/out a loss of passive system integrity or form closure.
- Neural system impairments (over or under-activation of any muscle that attaches to the thoracic ring) are by far the most common finding and result from re-distribution of muscle activity and changes in motor output as a consequence of pain secondary to macro or microtrauma (Hodges & Smeets 2015). In this instance, the thoracic ring can be manually corrected and this correction often results in a huge improvement in both the performance of the screening and meaningful task as well as the patient’s experience while performing the task (Figure 1).
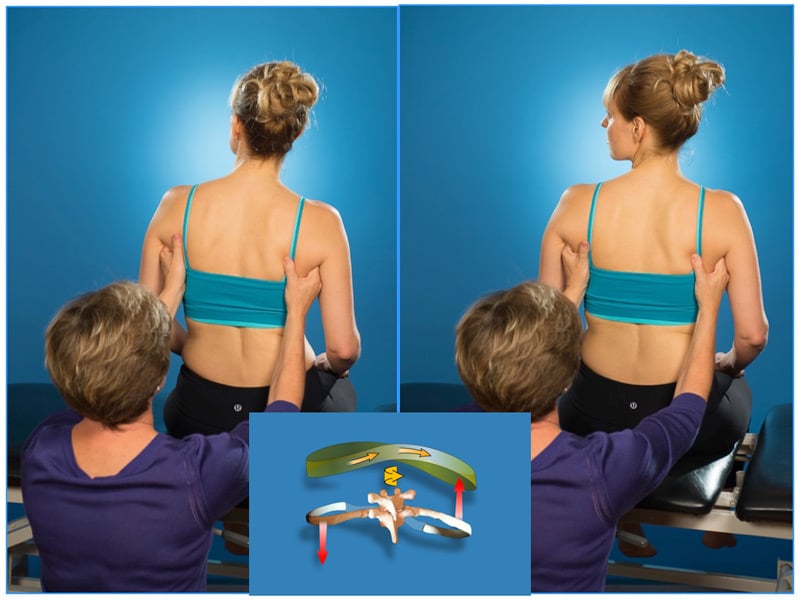
Figure 1 Left
The therapist is monitoring the biomechanics of the mid-thoracic rings (3-6) in the mid-axillary line as the patient rotates her head and neck to the left. Optimally, the mid-thoracic rings should rotate to the left. See the inset picture for the required osteokinematics and arthrokinematics of the mid-thoracic rings during this task. Note the available range of left head and neck rotation. The 4th thoracic ring starts right rotated/left translated and fails to left rotate/right translate during this task. In this region of the thorax, right rotation couples with right sideflexion (Lee 2015) thus the noted depression of the right scapula.
Figure 1 Right
The starting position of the 4th thoracic ring can be corrected (thus ruling out an articular restriction) and when the active range of motion for left rotation of the 4th thoracic ring is facilitated during left rotation of the head and neck the range of motion for this task is dramatically increased and the patient’s experience is positive. Additionally, note the change in posture of both the mid-thorax and right scapula. While not perfect, it is much better and suggests that further assessment to determine what is causing the non-optimal alignment and biomechanics of the 4th thoracic ring is relevant for improving the ability of this patient to turn their head to the left.
When manually correcting the relevant thoracic ring (or combination of rings), resistance is felt both on initiating the correction (beginning feel) and on its release. The location, direction and length of the force vector felt during both correction and release suggest the muscles to be assessed for over-activation. When the neural system (altered motor control) is determined to be the underlying system impairment of the specific thoracic ring(s) further tests to analyze the recruitment strategies of the segmental and multisegmental muscles pertaining to that specific ring during the specific screening task are indicated in order to plan treatment.
Specific passive arthrokinematic joint mobility tests often reveal asymmetric mobility findings and can be misinterpreted unless they are performed with the thoracic ring corrected to a neutral starting position.
Summary
In summary, to determine if non-optimal alignment, biomechanics and/or control of the thorax is contributing to the patient’s pain state and/or condition, an understanding of how the thorax should perform during tasks related to the patient’s story is required. Then, tests for active mobility, passive mobility and control (stability) can be applied to the specific thoracic ring(s) found to be behaving in a non-optimal manner during a specific screening task based on the meaningful task that is related to the patient’s goals. If the thorax is relevant to the clinical picture, correcting its alignment, biomechanics and control will make an immediate difference in function, performance and the patient’s experience.
The thorax is now recognized to be a contributor in multiple pain states and conditions and once the skills are acquired to determine individual thoracic ring alignment, biomechanics and control, assessment of the thorax is easily incorporated into a thorough whole body/person evaluation in a timely manner. Poor thoracic function is found in most musculoskeletal conditions but it is not always necessary to treat it. When it is relevant to the clinical picture the fundamental orthopaedic assessment tests for posture, movement and control will reveal the underlying system impairment, which then directs treatment. For further information on online and live classes on the thorax and its contribution to a multitude of patient conditions see www.learnwithdianelee.com.
Diane Lee
Diane Lee and Associates, Surrey, B.C. Canada
References
Hodges P W, Smeets R J 2015 Interaction between pain, movement and physical activity. Short-term benefits, long-term consequences and targets for treatment. Clin J Pain 31:97-107
Lee D 1994 Manual therapy for the thorax – A biomechanical approach. Diane G. Lee Physiotherapist Corporation
Lee D G 1993 Biomechanics of the thorax: a clinical model of in vivo function. Journal of Manual and Manipulative Therapy 1:13
Lee D G 2015 Biomechanics of the thorax – research evidence and clinical expertise. The Journal of Manual & Manipulative Therapy, 23(3):128–138
Lee L-J 2003 Thoracic stabilization & the functional upper limb: restoring stability with mobility, Course Notes. Vancouver, BC
Pettman E 1981 The Quadrant Courses. Orthopaedic Division of CPA.
Pettman E 1984 The Functional Shoulder Girdle. IFOMT, Vancouver
Siegel D 2010 Mindsight. New York. Bantam books. P 64
Sizer P S, Brismée J M, Cook C 2007 Coupling behavior of the thoracic spine: a systematic review of the literature. Journal of Manipulative and Physiological Therapeutics. 30(5):390–399



