Story
In September 2022, Mrs B presented to the clinic for an initial assessment and treatment. She chose to come to the clinic as she was an avid CrossFitter who was a former high level CrossFit master’s athlete. At the time of the assessment, Mrs B was a 53-year-old woman with two children. She was aware of my own background in the sport and knew I would not dismiss her based on how she chose to exercise. She mentioned it being difficult to find therapists over the years as they would often lecture her about the level and intensity of training she did at her age. I was recommended by several people from the gym she attended due to my approach to assessing dysfunction.
- Diane’s comment:
Wow, this is really, really sad, glad she found you.
She came to the clinic two weeks after injuring her lower back during a Crossfit session. She had been participating in a Crossfit workout for approximately fifty minutes, when the injury occurred. She described feeling ok prior to and during the workout, she added that she was tired from work that day. She said this feeling would normally pass once a workout started. However, in this case, it did not. During the last repetition of a deadlift movement in the workout she felt her lower back go into a spasm, and she felt as though her left side from the pelvis up to her mid back locked up. She tried to stretch it out after the workout; however, this provided limited relief and did not ease the spasm. She felt no numbness or tingling. The pain was localised to her lower back and up into the left side of the thorax.
- Diane’s questions:
The International Association for the Study of Pain has recently updated its classification to three phenotypes for pain: nociceptive, neuropathic, nociplastic. How would you classify Mrs B’s immediate pain and what findings from the story so far justify this classification?
- Stuart’s response:
Mrs B experienced nociceptive pain. The IASP definition of nociceptive pain is “pain that arises from actual or threatened damage to non-neural tissue and is due to the activation of nociceptors”. Mrs B experienced an acute event where she had a sudden onset of pain that lasted for a short period of time during a specific movement. In the story she did not mention any symptoms associated with neuropathic pain, such a dysaesthesia, paresthesia, or radicular like symptoms such as shooting pain down her leg. The pain was also an acute onset, with a definable event. Nociplastic pain is defined as pain that arises from altered nociception despite no clear evidence of actual or threatened tissue damage.
Mrs B went home, rested, and put some heat on her back. The next day, she felt better; however, her lower back felt tender and between her shoulder blades felt extremely tight. She no longer felt as though they were connected i.e., the mid thorax and lower back felt separate. The pain eased in the lower back over the coming days. She described her whole spine generally feeling tight, from her head to her pelvis. She decided to wait until she saw me before she trained again as she was rattled by the injury to her lower back.
- Diane’s questions:
What is known from the evidence on the response of the back extensor muscles that could help Mrs B understand, and be ‘less rattled’ as to where this tightness was coming from and why?
- Stuart’s response:
Onset of or persistent lower back pain often leads to increased activity of the superficial erector spinae muscles such as iliocostalis lumborum or longissimus thoracis, (Hodges and Chloewicki, 2013). There is also a variable response from the internal oblique, external obliques and rectus abdominis, (Lee, 2011). One reason for this is the delayed or impaired function in TrA and dMF, (Hodges and Chloewicki, 2013).
In practice I find there is usually a particular fascicle of longissimus or iliocostalis lumborum that extends from a lumbar spine region (such as L4/5 or L5/S1 in the case of back pain) where the patient has lost control. You can also trace the fascicle up to an associated thoracic ring. In the sessions, I usually show a quick visual demonstration of where these muscles attach onto the thorax. This helps patients like Mrs B understand how muscles from the lumbar spine can create a sensation of tightness that extended up into her mid thorax; or why I’m assessing thoracic rings. I will also palpate the particular fascicle up to the thoracic ring to give the patient some kinaesthetic feedback as well.
Mrs B said she always strived to move well and worked hard to ensure she only did things her body was capable of. She did not believe in “muscling through” workouts. Having experienced ridicule from peers for doing CrossFit, she took pride in the fact she remained relatively injury free.
Prior to the flare up, Mrs B had not suffered from any lower back injuries during Crossfit. Mrs B had previously experienced an ever-present tightness in her right shoulder that got worse the more she trained. She had seen other therapists and practitioners; however, they were unable to address the issue. She would receive routine treatment via soft tissue work to manage the tightness and pain that built up over a period of training. Although it became painful, she said it never felt like an “injury”. During her CrossFit Games preparation, she received treatment weekly to ensure she was not distracted by it. She was given multiple different reasons as to why it was a problem, but no one had ever been able to relieve it completely. Since ceasing high level competitive CrossFit a few years prior, she found she could manage it with stretching and mobilising in order to train, though it never went away. Additionally, she would get a “tune up” now and then if it got out of her control.
- Diane’s question:
When something ‘doesn’t go away’ we usually feel (in the ISM model at least) that the symptomatic body region is a victim of an impairment elsewhere. How does this shoulder report in her story modify your ‘low back pain’ assessment from an ISM perspective?
- Stuart’s response:
The shoulder aspect of the story indicates there is a long term, underlying issue that hasn’t been resolved. As you said, the shoulder sounds as though it has been a victim of impaired biomechanics in another region other than the shoulder. Given Mrs B’s diligence with training, and regular treatment of the shoulder, one would assume if it was a “shoulder driven shoulder” it would have cleared up and gone away. This information gives further recourse to assess Mrs B thoroughly as it is likely the seemingly random onset of back pain is in fact another symptom of an underlying issue. When assessing Mrs B I would view the lower back assessment as a only a segment of the whole assessment of Mrs B.
One thing I like I about the ISM assessment is that it is objective from the start. We can pick a task that is meaningful to the patient, so they feel as though they are being heard in terms of what is wrong, but their body leads us to the major site or sites of impairment. Once you start assessing, all the preconceived notions disappear as everybody is so different.
- Diane’s comment:
So true Stuart, and what I love is that there is minimal judgement in this approach, yet many who are not trained it in feel there is, thus the need for appropriate language when reporting an ISM case. We can have an initial impression, or judgement if you like, but further testing either validates or negates that impression and we always try to triangulate our findings and clinically reason all results to arrive at the best evidence and clinically informed decision for planning treatment.
Mrs B said that in the lead up to this workout, she had been very stressed at work. This was an unusual amount of stress for her. She also admitted her training had decreased due to the stress over the last couple of months. The stress had also affected her sleep and she was aware that she had been clenching her teeth a lot. She knew this as she could feel her jaw was tight upon waking and would need a few repetitions of opening before the tightness would subside. She mentioned this was a habit she had developed in her twenties. However, until the work stress had started a few months ago, she had managed to break that habit. Or at least she wasn’t aware of any tightness in jaw upon waking until recently.
- Diane’s question:
Is this information of any relevance to how you will plan treatment?
- Stuart’s response:
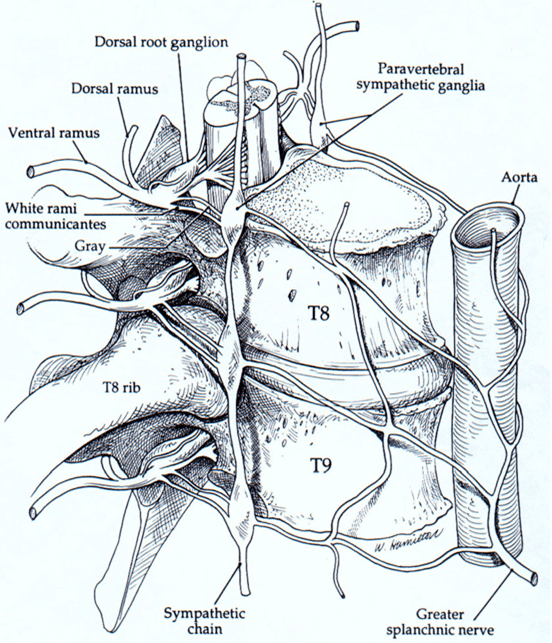
This information is very important for a number of reasons. The first reason is Mrs B’s acceptance as stress being a part of her story. This alerts me to the fact that her sympathetic nervous is, or has been, upregulated. This has ramifications for assessment and treatment, as her limbic system is likely to be on high threat alert. When the body is in a cyclical state of stress, it makes the body more prone to new stressors, (Marlien, 2021). Sustained stress creates an environment where the parasympathetic system is depressed by the competing sympathetic system, (Porges, 2011). This has ramifications for pain tolerance, healing, and the body’s perception of stress, (Marlien, 2021; Porges, 2011). Therefore, the best approach for Mrs B might be a “less is more” type approach. Overloading her with too much testing and heavy treatment may make her feel worse. The treatment may also require techniques to downregulate the nervous system before you can begin to treat the movement impairments. Such techniques involve downregulating the sympathetic nervous system and promoting the dorsal vagal system to increase parasympathetic activity, (Marlien, 2021). Such techniques may involve inhibition of the stellate ganglion at the cervical plexus, or the celiac ganglion, or superior mesenteric ganglion, or inferior mesenteric ganglion or the adrenal glands (Marlien, 2021; Stylian, 2022).
Understanding the role of the autonomic system in Mrs B story will also help shape the language used when describing what the findings are. You need to create a highly supportive, compassionate, and calm environment for the patient, (Lee 2011; Hengeveld and Banks, 2014). Highly medicalised language would not be appropriate, nor would it be wise to make threatening statements without evidence such as “it could be your disc that’s causing the pain”. Being aware of the patient’s emotional state and background leading up to them seeing helps you to come in at a level that is appropriate to the patient. This helps build trust and shows you care about their wellbeing.
Knowing the autonomic nervous system is part of the story is also useful for planning home exercise programs. Part of the homework may involve down regulating the sympathetic nervous system before Mrs B begins any corrective exercises. This would help to reduce the nervous system’s perception of threat, and increase its resilience to stress (Marlien, 2021; Porges, 2011). The choice of exercise is also important. Like treatment, it may be better to do less in the beginning until the patient can regulate their autonomic nervous system better.
This part of the story also alerts me to the fact that there may be other systems involved with Mrs B’s presentation such as the dural system, that may need treatment. Although you don’t want to have bias going into an assessment it, like the shoulder part of the story, alerts you to the fact that there may be more going on with this patient than meets the eye. Through experience, I have found this is often the case. It might not show up in the first treatment, but it will sometimes come up later. Thankfully ISM always takes you where you need to go!
Lastly, the information is relevant to the overall treatment in terms of understanding who the patient is in front of you. A patient’s cognitive and emotional dimensions may play a role in why the injury occurred, or how they respond to it, and how much pain they feel, (Hengeveld and Banks, 2014). Emotional states can also express themselves in physical postures that correlate with altered motor control, (Lee, 2011). Negative emotional states have been correlated to decreased flexibility of muscles when tested in isolation (Kurz, 2016).
In Mrs B’s case, stress would have played a role in her injury. Mrs B also noted that her habit of jaw clenching is directly related to stress and was a habit for her in the past. Her prior history has become a part of her current situation. Therefore, part of Mrs B’s treatment may require her to address the stressful aspects of her life. The awareness of outside factors playing into injury can be a powerful tool for recovery, (Marlien, 2021). Mrs B may need to be referred for counselling as her mental health could be a barrier to recovery.
- Diane’s comment:
Great answer and well-integrated!
Mrs B’s medical history included a c-section 17 years ago and she also had a laparoscopic surgery for a left ovarian cyst removal 2 years prior. Her only other complaints were the previously mentioned right shoulder issue that would often lead to golfer’s elbow in her right elbow if she engaged in a higher volume of training.
Meaningful Complaint
At the initial assessment, Mrs B’s primary complaint was lower back weakness when bending or hinging forward and feeling stiff in her mid-thorax. She did not feel comfortable with the idea of loading her lower back into flexion or squatting.
Cognitive and Emotional Beliefs
Mrs B wasn’t sure why she had hurt her back, which reduced her confidence. She believed she was likely to do it again and was fearful of going back to training or loading her back. She had the cognitive belief that her body was no longer capable of training hard. Therefore, she was worried her body wasn’t capable of Crossfit anymore and felt quite deflated as a result. The injury has taken away the self-assurance that she was capable, and she had lost belief in her body’s ability to perform. She said she suddenly felt old.
- Diane’s comment & question:
This is a huge statement Stuart and one I can resonate with! Aside from telling her this isn’t true, what is a better way of busting this cognitive belief and how did you frame that initially to Mrs B?
- Stuart’s response:
My first comment to people when they say they are getting old is to say “age is not a diagnosis”. For Mrs B, education around the factors that led to the injury would be the best way to break this cognitive belief. For Mrs B there was a defined set of events that led to this happening:
- Increased stress
- Decreased sleep
- Decreased training frequency
- Decreased energy and focus
Those factors will play a role in motor control under fatigue during sporting activities and make it more likely that someone will injure themselves (Kurz, 2016).
Linking up the aspects of her story with the findings from her screening task will also help connect the dots as to why her back became sore at the end of the workout. As mentioned previously, there are parts of her story that point to an underlying issue that may have needed the above factors to present itself. She has also not complained of back in the past, therefore this is essentially her first back injury in many years of competing in the sport of CrossFit.
So, with this all-in mind, during the session I showed her there was a combination of factors that led her injury. I said that her body was giving warning signs a long time ago; however, as conditions were manageable, her body could handle it. The increase in negative factors was what led to the system failing. It could no longer cope and decided to tell her it had had enough. However, I told her this was a blessing in disguise as it gives us a chance to resolve the underlying issues, so she is even better than she was before. This helped overcome her cognitive belief that it was her age that was the problem and that her body wasn’t capable anymore.
- Diane’s comment:
I like this approach; it is biopsychosocial right from the start.
Meaningful Tasks
Mrs B’s goal was to ease back into training without fear of injuring herself again. As the injury occurred during a Deadlift movement, I decided this movement would be the screening movement for the session.
Considering her recent flare up of symptoms, and her cognitive beliefs, I conducted the screening task unweighted. Mrs B essentially mimicked holding onto the bar, her body was in the same position she would be when she carries out this movement in the gym. She felt safe enough during this movement to be able to be assessed.
Screening Tasks
Functional Unit #1
Standing Start Screen
Mrs B had no symptoms in the standing start screen position. The standing start screen helps to establish the baseline position of the body before the screening task related to the meaningful task is assessed. This makes it easier to establish which findings are relevant and which are not. Hence, finding the findings. As every patient is an individual, we must treat them as such. Having a baseline assessment helps to establish objective findings in that patient at that time. This helps to prevent therapist driven bias’s coming into the assessment that might cloud the assessment process.
- Diane’s comment:
Excellent to note. We all have biases and the more we can negate those the more valid our findings will be.
We cannot assume, as therapists, that all findings are relevant. No one body will stand in perfect alignment, and our job is not to create this. Our job also isn’t to simply pick out faults in the patient. To quote A.T. Still, “Anyone can find disease, to find health should be the object of the practitioner”, (Lewis, 2016). Any findings we do find must then be assessed in a way that is relevant to the patient. Therefore, we are looking for any non-optimal biomechanics for the patient relevant to their meaningful task.
- Diane’s comment:
ISM is often criticized for making judgements that are not based in evidence pertaining to posture and alignment. Stuart makes an excellent point here as to how an ISM approach minimizes this judgement bias.
Findings
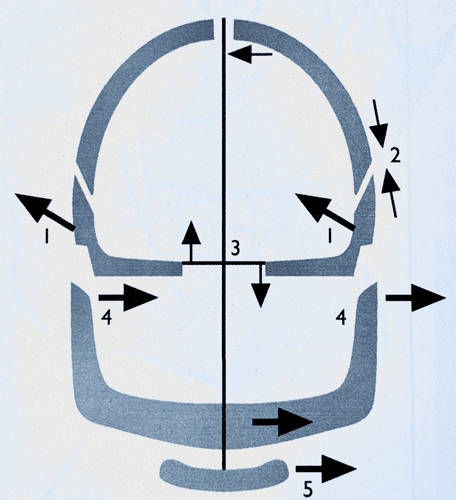
Pelvis: The pelvis was in a left transverse plane rotation (TPR) with a congruent left intrapelvic torsion (IPT)
Hips: The left head of femur (HOF) was anterior to the left acetabulum. This is an incongruent finding relative to the left transverse plane rotation of the pelvis.
- Diane’s question:
If the left femoral head was anterior to the right femoral head and not anteriorly translated to its acetabulum, would this have been a congruent or incongruent finding with the LIPT? If the pelvis was neutral and left femoral head was anterior to the acetabulum, is this incongruent? Essentially, there are two incongruencies in your findings, what are they?
- Stuart's response:
For a LIPT, If the left femoral was anterior to the right femoral head, this would still be an incongruent finding in a LIPT.
If the pelvis was neutral, and the left femoral head was anterior, this would be an incongruent finding. In neutral the femoral heads should be centred in the acetabulum and in line with the pelvis in the frontal plane.
For the pelvis in this case, the two incongruent findings were:
- The left femoral head relative to the transverse plane rotation of the pelvis
- The left femoral head relative to the left acetabulum
Lower Thorax: The lower thorax was generally right rotated in the transverse plane.
The 10th thoracic ring (TR10) was translated left and rotated right, which is an incongruent finding relative to the pelvis. The 8th thoracic ring (TR8) was translated right and rotated left. This was an incongruent finding relative to TR10. The 7th thoracic ring (TR7) was translated left and rotated right. This was an incongruent finding relative to TR8 and the pelvis. The 5th thoracic ring (TR5) was translated left and rotated right, incongruent to TR8 and the pelvis.
Lumbar Spine: The 5th lumbar vertebrae (L5) was rotated to the right relative to the pelvis. This was an incongruent finding relative to the pelvis.
- Diane’s question:
Think for a moment about the position of the sacrum and innominates in a left intra-pelvic torsion. What, in particular, is L5 rotated incongruent to? Then think about the anatomy of the iliolumbar ligaments on the left and right side of L5-S1 and tell me which bands on which side would be under greatest strain with this incongruence? How would you develop a pain provocation test to validate/negate a hypothesis of a particular band possibly producing nociception? To answer this, you have to review the biomechanics of coupled motion of L5-S1, review the anatomy of the 5 bands of the iliolumbar ligament and then develop some very specific tests for each! Not sure how it would guide treatment, but it is an exercise in applied anatomy and biomechanics and provides a higher level of understanding for Mrs B. I think she would like this a lot!
- Stuart's response:
L5 is incongruent to the sacrum due to its articulation with the sacrum via L5/S1. The sacrum is rotated to the left, while L5 is rotated to the right. L5 is also flexed, and side bent to the right, (Lee, 2011). This is incongruent biomechanics between L5 and the sacrum.
The 5 bands of the iliolumbar ligament include (Lee, 2011; Bogduk 2012):
- Anterior or ventral band: Attaches to the anteroinferior aspect of the entire length of the transverse process of L5. It blends with the superior band anterior to quadratus lumborum (QL) and attaches to the anterior margin of the iliac crest
- Superior band: Attaches at the tip of the transverse process of L5. The band divides laterally to envelop QL and inserts onto the iliac crest
- Posterior band: Arises from the tip of the transverse process of L5, attaches laterally to the iliac tuberosity posteriorly and inferiorly to the superior band. It also attaches to the thoracolumbar fascia.
- Inferior band: attaches onto the body and inferior border to the transverse process of L5. Inferiorly the band inserts onto the iliac fossa, while crossing the ventral sacroiliac ligament
- Vertical band: The vertical band attaches onto the anteroinferior border of the transverse process of L5 and then descends vertically to insert onto the posterior aspect of the arcuate line
The bands with the greater tension in a LTPR/LIPT of the pelvis with L5 rotated and side bent right would be:
a) The left posterior, superior and anterior parts of the ligament
b) The right inferior and vertical part of the ligamentFigure 2: Schematic of ligament tension during rotation, flexion, and extension (Viehofer et al. 2015) I found there is surprisingly little agreement on what the different parts of the ligament restrain. Sims and Moorman (1996), agree on the following with regards to stabilising L5 when the bands were divided bilaterally:
a) The posterior bands account for 61.2% of stability in flexion
b) The anterior bands account for 20.41% of stability in extension
c) The anterior bands account for 141.7% of stability in side bending
d) Both bands account for 5.3% of rotational stabilityFrom an observation of the anatomical location of the ligament and with the information from a study done by Viehofer et al. (2015) seen in Figure 2, I would say each part does the following:
Anterior band: restrains extension and side flexion
Posterior band: restrains flexion and rotation
Superior band: restrains side flexion
Vertical band: sacroiliac joint sagittal plane motion (nutation/counternutation)
Inferior band: Extension and rotationTherefore, to test each part of the ligament you would need to stabilise the sacrum and innominate and then do the following tests in standing:
- Anterior band – extension and side flexion away from the left side
- Posterior band – flexion and rotation away from the left side
- Superior band – side flexion away from the left side
- Inferior band – extension and rotation away from the left side
- Vertical band – extension
Pain provocation in a particular direction might indicate a particular band of ligament is the source of the nociception. This would only be accurate if you were certain there was no other structures involved in the pain provocation testing.
- Diane’s comment:
I wonder if all this testing has been done looking at a neutral sacrum and then moving L5, in other words, modelling the pelvis as a cylinder? If the intra-pelvic torsion and its impact on ligament tension in this complex isn’t considered, then it can likely be hypothesized the way you have done this. One example, in a LTPR/LIPT the sacrum is rotated left and nutated relative to the left innominate and the left innominate is posteriorly rotated relative to the left side of the sacrum. Normally, L5 follows the posterior rotation of the left innominate and rotates/side flexes to the left. Let’s consider just the left vertical band in this scenario. Posterior rotation of the left innominate would slacken the left vertical band as would left side flexion of L5. The conjunct left rotation of L5 relative to the sacrum; however, increases tension in this band thus maintaining the tension. If the L5 was rotated to the right and side flexed right, the right rotation would slacken the tension and the side flexion would tense the vertical band. So, for me it isn’t likely that this band is a source of nociception.
Consider now the left superior or posterior band that attach from the transverse process of L5 to the iliac crest. Posterior rotation of the left innominate coupled with RIGHT rotation/RIGHT side flexion of L5 would really tense these bands. Neither the movement of the sacrum, innominate, nor L5, offloads/balances this increased tension. This is what I often see clinically when a patient presents with L5 rotated incongruent to the sacrum particularly when the SIJ doesn’t unlock (innominate doesn’t anteriorly rotate which would balance tension). A specific pain provocation test would be to further right rotate L5 and posteriorly rotate the left innominate, although I’m not sure we can say for sure that it is only these bands (posterior and superior) that are nociceptive if pain is produced, as you mention above. This pattern is often associated with inhibited deep segmental multifidus to the left of L5 with, or without, atrophy.
- Stuart's response:
That is extremely interesting and explains something I notice when treating some patients who have the lumbar spine as a secondary driver that can’t be corrected. I find needling the iliolumbar ligament (in particular the superior or posterior band) restores segmental multifidus control where there is no atrophy of multifidus. On testing it appears as though there is a lack of coordination between transverse abdominis and the deep multifidus at that level, however, there doesn’t appear to be any wastage of multifidus. Then after treatment I’ve testing again and found the coordination is restored.
- Diane’s comment:
Interesting! Have you read this paper? Indahl, A., Kaigle, A., Reikerås, O. & Holm, S. Electromyographic response of the porcine multifidus musculature after nerve stimulation. Spine 20, 2652–2658 (1995).
They found this in pigs:
Stimulation of the disc anulus fibrosus induced reactions in the multifidus on multiple levels and on the contralateral side, whereas stimulation of the facet joint capsule induced reactions predominantly on the same side and segmental level as the stimulation.
There’s the evidence for your technique!
- Stuart's response:
Yes! I remember you showing me this study in Part 1. That’s what spurred me on to try that.
- Diane’s comment:
Now that’s translating evidence into clinical practice!
The 4th lumbar vertebrae (L4) was rotated left.
- Diane’s question:
L4 was rotated left relative to the coronal body plane or relative to L5? Why is this clarification essential?
- Stuart's response:
The biomechanics of lumbar vertebrae rotation involve all three planes of motion. When L5 rotates to the right it does the following, (Lee, 2011, Bogduk 2012):
- Rotates to the right in the transverse plane (axial rotation)
- Rotates to the right in the frontal/coronal plane (side flexion)
- Rotates forward in the sagittal plane (translation)
In this rotated and side flexed position L5 has created a new axis of rotation that is no longer in any pure body plane. Therefore, L4 needs to be assessed relative to L5. Without this information the position of L4 could be assessed incorrectly leading to confusing or inaccurate findings.
- Diane’s further question:
So tell me, where was L4 relative to L5 regardless of the coronal plane of the body?
- Stuart's response:
L4 was rotated left relative to L5 as L4 is rotated and side bent to try and compensate for the right rotation of L5. Due to the ligamentous attachments and orientation of the zygapophyseal joints, L4 should rotate in both the coronal and transverse planes (sideflex & axially rotate) relative to L5. This is because the axis of rotation is through the vertebral body. According to Bogduk (2012), the L5/S1 joint coupled movements are more consistent than the coupled movements of L4/5. Therefore, lateral flexion of the vertebrae will be coupled with ipsilateral axial rotation at L5/S1, (Bogduk, 2012). However, L4/5 has a variable response with either ipsilateral or contralateral coupling, (Bogbuk, 2012). This might explain in clinic why L5 and L4 don’t always exhibit the same pattern.
- Diane’s comment:
nice finding! I didn’t know this – this is like the AA joint in the neck!
- Stuart’s continued response:
In this case however, L5 was rotated to the right, and L4 was rotated to the left. The rotation of L4 was about the axis of the vertebral body of L5 in the transverse plane of L5 not the transverse plane of the patient’s body itself. So, if the pelvis is in a left transverse plane rotation, L5 is rotated to the right, and L4 rotates to the left around L5’s orientation; does that mean L4 is still rotated to the right relative to the position of the pelvis? My answer would be yes.
Also, to your point above, when they studied the mechanics of the lumbar spine were the sacrum and innominates relative to the lumbar spine when they assessed it? I feel like there needs to be more study in relation to that.
I like the quote you put into The Pelvic Girdle from Stokes’ book that clinical observation of a patient’s spinal motion is the most direct way to assess it, despite its lack of objectivity. It highlights that you really need to see what’s in front of you rather than assuming you know what’s going on.
- Diane’s comment:
OK, my brain is hurting now with all this relative biomechanics and it is so true!
Unweighted Deadlift
The task I chose to assess any change in findings from the standing start screen was an unweighted deadlift or hinge motion. This was the movement Mrs B was doing when she injured herself and was therefore the most meaningful to her and relevant to her cognitive beliefs.
An optimal hinge strategy for the deadlift involves both innominates remaining posteriorly rotated relative to the sacrum. The pelvis should remain neutral in the transverse plane. The femoral heads should remain centred throughout the task. The hindfoot, should start in neutral alignment if moving from standing into the hinge. They will pronate and supinate as the knees flex and extend in and out of the movement. The lumbar spine, thorax, cervical spine, and cranium should also remain neutral through the movement. The shoulder girdles should remain neutral, and the humerus will flex and extend as the bar moves around the body.
In this task, I felt it was best to assess the patient from standing and then hinging into the movement. Normally the deadlift starts by picking the bar up from the floor. Mrs B said that she felt pain when she was lowering the bar, not lifting it. Therefore, it was in the eccentric phase of the deadlift, which starts from a standing position into a semi squat.
- Diane’s comment:
Excellent deconstruction of the part of the task that has the most meaning!
Given Mrs B could stabilise in standing, I needed to assess at what point in the task her body could not maintain optimal alignment and biomechanics. This occurred very early in the task, assessing from the bottom position of the movement would provide false negatives or at least unclear findings.
Findings
Pelvis: During the task the pelvis remained in a left TPR and the left SIJ unlocked (lost control). This happened at a point 20% into the task.
Hips: The left HOF moved further anterior relative to the left acetabulum. This continued to be an incongruent finding relative to the left TPR of the pelvis. The increase in femoral head translation occurred just before the unlocking of the left SIJ.
Lumbar: L5 increased its rotation to the right when the left SIJ unlocked. L4 also increased its rotation to the left as L5 rotated to the right.
- Diane’s question:
Let’s carry on the iliolumbar conversation here. L5 is rotated incongruent to the direction of rotation of the sacrum in a LTPR. Is it congruent or incongruent to the innominate motion when the left SIJ now unlocks? If it isn’t following the sacrum what could it be following?
- Stuart’s response:
L5 is following the innominates. The left innominate rotates anteriorly as the sacrum counter nutates. The posterior and superior bands of the right iliolumbar ligament take L5 to the right.
- Diane’s response:
Exactly and I suspect this puts a lot of ‘stress’ on the facet joints at L5-S1.
Thorax: The lower thorax remained right rotated in the transverse plane. TR10 increased its translation to left and rotation right relative to the pelvis.
At this point I had three incongruent findings to work with (the left hip, the pelvis ( TPR & left SIJ unlock) and the lower thorax (TR10). I first corrected the left hip as it gave way before the left SIJ unlocked. Correcting the left hip restored control and alignment of the pelvis and alignment of TR10. Correcting the left hip did not correct the lumbar segments (L5 & L4) fully, L5 and L4 still rotated incongruent to each other but later in the task now. The task experience felt better to Mrs B, but her body position did not look good, she rotated more to the right in her upper thorax and cranium.
Correcting the left hip did not correct TR8. TR8 remained translated right and rotated left during the task. It did not change position when tested in the movement. I noted that correcting the left hip however improved TR7 and fully corrected TR5 in the upper thorax.
The left hip, so far, was the best overall correction of the corrections for the thorax in FU1. However, correcting the left hip did not make a change to TR8. When I partially corrected TR8 it corrected TR7, but this correction did not change the left hip in the task. TR8 was the best choice of thorax corrections but was a secondary driver.
The correction at TR8 was only a partial manual correction and it felt like there was an intra-thoracic ring articular restriction. I would need to mobilise any articular restrictions within TR8 to assess if it really was a secondary driver in the thorax and to assess if changing the osteokinematics of TR8 could potentially change the neural drive to the lumbar spine or left hip. Currently, the manual partial correction of TR8 was not changing the left hip. Also, when correcting TR8, Mrs B did not look or feel good. So rather than stop there I chose to continue with the assessment as I felt it was unlikely TR8 was the primary driver. Had Mrs B looked and felt good with the TR8 correction I would have stopped there and treated any articular restrictions within TR8 that needed to be treated. Then I would have gotten Mrs B up again and re-assessed.
- Diane’s comment:
Normally, I have tons of questions, but you are reasoning this flow in an excellent manner Stuart!
Driver for Functional Unit #1
In relation to the findings at the lumbar spine, correcting the left hip improved the lumbar spine but did not give a full correction. Therefore, the left hip had the best overall correction for everything in FU1 except for TR8. A partial correction of TR8 and the left hip did not give a better correction than the left hip alone to the task or to the lumbar spine. In ISM, there are no manual corrections for the lumbar spine. The lumbar spine was also a secondary driver as there was no full correction of the alignment and biomechanics of the lumbar spine by correcting the primary left hip driver or secondary thorax driver. Therefore, the lumbar spine was also a secondary driver.
At this point I had a primary left hip driver, with a secondary thorax and lumbar driver.
Mrs B’s lumbar spine was still giving way under load, although later in the task. With the left hip corrected it felt better to Mrs B, but the body positioning didn’t look right in the task. When I corrected the left hip, it made the upper thorax worse and increased the TPR of the shoulder girdles. This also increased the right rotation of the cranium. A left hip and thorax correction with TR8 also made the upper thorax, shoulder girdles and cranium look worse. Mrs B could also feel this as she went into the movement, hence why I chose to leave TR8 alone for the time being.
Therefore, I felt it was relevant to continue into FU2 to see if there was a better correction from another site of impairment in FU2 that made Mrs B look and feel better than what I had found in FU1. The change to body regions in FU2 with a change to the findings in FU1 would indicate there was a relationship between these regions that needed further investigation.
- Diane’s comment:
Indeed, it would.
A quick screen for cervical rotation showed it was restricted to the left.
- Diane’s question:
Was this quick screen task done in standing or the deadlift position? It should be done in the screening task position.
- Stuart’s response:
I had not thought of doing it in the task, though now you have asked the question it seems glaringly obvious that you should. That would make more sense as you want to assess how the various body regions are responding to the loading of the task.
- Diane’s response:
Some of our best learning occurs with the simplest of questions, right?
- Stuart’s response:
The more I practice, the more I realize it’s the finer details that make the most difference. The more you know and understand anatomy and biomechanics (how you teach it anyway) the less you have to do when treating patients. Plus, you get better results!
I used this as a quick screen to objectively assess the impact of correcting the FU1 drivers on FU2. If there had been a complete correction of cervical rotation, it could be hypothesised that the FU1 driver is also the best overall correction for FU2. Then I would move to FU3. Although based on what I saw from the FU1 corrections, this seemed unlikely. When I corrected the left hip in standing, not the deadlift position, it worsened the cervical rotation to the left. This confirmed my choice to continue into FU2 as there seemed to be a relationship between the functional units. The correction of the left hip had a negative impact on the alignment and biomechanics of the body regions in FU2, meaning the left hip was not the primary driver for the overall task. It was the primary driver for FU1.
Functional Unit #2
Standing Start Screen
Findings
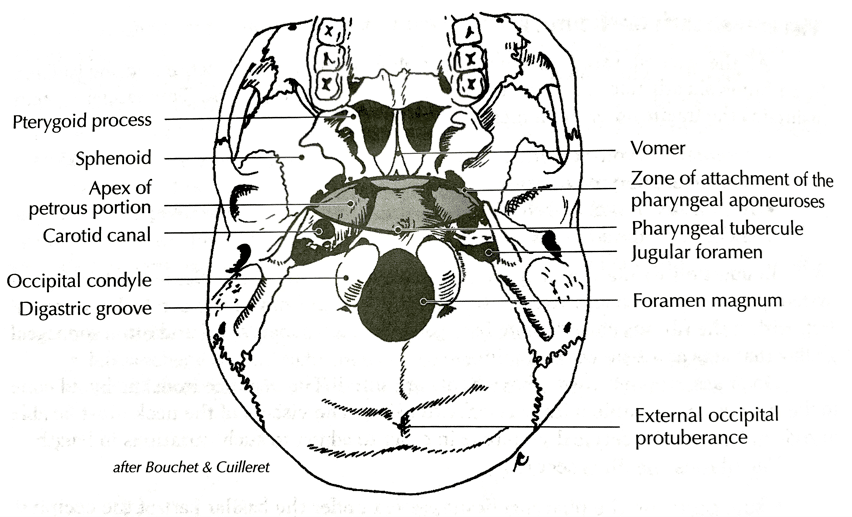
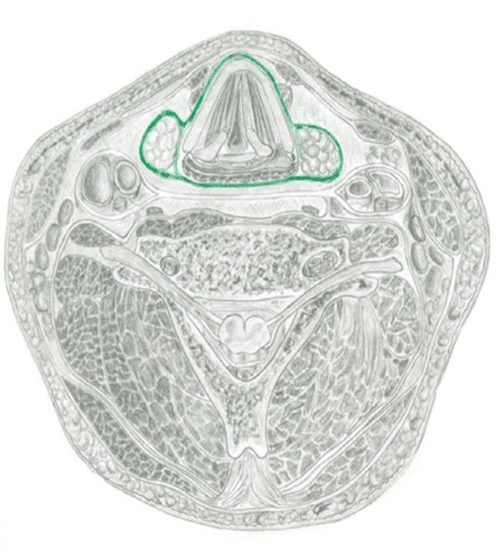
Cranial region: The cranium: Right intracranial torsion (ICT) with an incongruent left rotated sphenoid. The sphenoid position was assessed from the front of the cranium by palpating the greater wing of the sphenoid on the left and right side and visually assessing the position of the left and right orbits relative to the rotation of the cranium. The first cervical vertebrae (C1) was left rotated. This is also incongruent to the ICT. The 2nd cervical vertebrae (C2) was right rotated/left translated.
- Diane’s question:
Given these start screen findings of the bones of the cranial region, tell me the start position now of the OA and AA joints. The pattern should then make sense.
- Stuart’s response:
OA Joint – The convex surfaces of the occiput glide posterior in flexion and anterior in extension. Normal coupling of the OA joints is contralateral. The occiput itself is rotated and side bent to the right (osteokinematically in space), The atlas is left rotated with right side flexion relative to the occiput to counter the position of the occiput:
- Right occipital condyle glides posteriorly – the atlas glides anteriorly on that side (arthrokinematically)
- Left occipital condyle glides anteriorly – the atlas glides posteriorly on that side (arthrokinematically)
- The occiput is then in right rotation but left side flexion relative to the atlas.
AA Joint – The axis (C2) is rotated to the right and translated to the left and side flexed to the right; there is ipsilateral coupling in the cervical spine from C2 down (C2-3). The atlas is left rotated, and side flexed to the right:
- The left C1 facet glides posteriorly as the left C2 facet glides anteriorly – AA extension on that side
- The right C1 facet glides anteriorly as the right C2 facet glides posteriorly – AA flexion on that side
The position of these joints is an attempt to neutralise the tension on the alar ligaments.
Cervical Spine: The 7th Cervical vertebrae (C7) was translated right and left rotated. This is incongruent to the ICT and C2.
Upper Thorax: The 2nd Thoracic Ring (TR2) was translated left and rotated right. The 1st thoracic ring (TR1) was left rotated. This was an incongruent finding relative to TR2.
Shoulder Girdles: There was a left intra-shoulder girdle torsion (ISGT). The head of humerus (HOH) were congruent on either side. This is an incongruent finding relative to TR2.
Summary of congruencies:
ICT, C2 and TR2 are right rotated.
Sphenoid, C1 and C7, TR1 and SGs are left rotated.
Unweighted Deadlift
Findings
During the task, the right ICT of the cranium increased, and the sphenoid remained incongruent in left rotation. TR2 increased its right rotation as did C2. The shoulder girdles remained the same in a LTPR while TR1 rotated to the left. I used these findings to determine where the driver was in FU2. I noted that the cranium and upper thorax were rotating to the right during the task. Given TR2 was rotated to the right and the next incongruent finding relative to the pelvis I corrected it first.
- Diane’s comment:
When working in functional units, we don’t compare everything to the pelvis – we look for incongruencies with the unit itself. So, my choice of correction order following this functional unit principle would have been to note the relationship first between TR2 and C7, then C7 and C2 – I would have prioritized these and then looked at the priority segment in relationship to the ICT. When the sphenoid rotation is incongruent to the ICT, this is like the hip being incongruent to the pelvis, you know you will have at least two intra-regional vectors/drivers within this unit. So, let’s see what Stuart found.
- Stuart’s response:
That makes more sense to me. I find as I am working my way up, I get a sense of what my hands should be on. The findings that play a role in the person’s presentation seem to make sense when you touch them. Though that isn’t “clinical reasoning” I have learned trust that sense since I started ISM as so much of what we do is about feel and listening to the body. However, maybe there is an unconscious clinical reasoning going on in the background that has pieced together the knowledge and experience you have gained over time.
I found that when I corrected TR2 it did not correct TR1, the cervical spine or cranium or the task. The TR2 correction did, however, correct the shoulder girdles.
As the cranium rotated to the right along with C2, I tried C2 as the next correction. This made no changes below and left the cranium in a RICT and made no change to the task. When I corrected the Cranium itself (co-correction of the sphenoid and ICT), it gave a full correction of the cervical spine and TR1 and the shoulder girdles. The cranial correction however, only partially corrected TR2.
Driver for Functional Unit #2
The cranial region was the primary driver for FU2 with a secondary thorax driver at TR2.
- Diane’s comment:
and there you have it – two drivers within the unit. There is no wrong or right way to order your corrections. Over time you will begin to recognize certain patterns.
- Diane’s question:
There are a lot of options for corrections with this many incongruent findings in both the start screen and the task. What made you decide to start with TR2? Do you have a clinical reasoning process for where to start with this many incongruencies or did you just start at the bottom and work your way up? Can you think of a better way?
- Stuart’s response:
I decided to go for the biggest incongruent findings relative to the pelvis (i.e. things that were rotated to the right). I did this as I noted that the overall direction of FU2 in the task was an increase in right rotation. TR2 was the first finding that was rotated to the right. C2 was next. Given that the cranium increased its right rotation with the left hip correction, and I had noted that there was a restriction in cervical rotation to the left, I should have started with the cranium first. Mrs B’s story also indicated that there may have been a cranial component to her story. So logically the findings in FU2 largely indicate compensations from a RICT.
Drivers for FU1 and FU2
FU1 PD Left Hip, SD Thorax (TR8?), and Lumbar spine
FU2 PD Cranial, SD Thorax (TR2)
Priority between Unit Drivers
I found the cranial correction partially corrected the left hip (the anterior translation occurred later in task). The lumbar spine still gave way with the cranial correction but closer to the end of range and TR8 remained the same. The correction of the left hip did not correct the cranium; it made it worse. The left hip correction alone also worsened TR2 and the cranium.
The TR2 correction alone did not change the left hip or lumbar spine or TR8, therefore it was a secondary driver in the overall task as well as FU2. When I corrected the left hip with a cranial correction and TR2 correction it gave the best correction to the task so far. This correction also gave the best correction to the lumbar spine at this point as well, it was the latest in the task that it had given way. However, as the lumbar spine still did not fully correct it was still a secondary driver in FU1.
The left hip, cranial and TR2 correction did not change TR8. it also remained as a secondary driver in FU1.
For the patient, both the look and feel during the meaningful task were the best with the left hip, cranium and TR2 corrected. Therefore, they were the best overall corrections for FU1 and FU2 so far.
Summary of unit drivers
Primary driver for the task: FU1 Left Hip and FU2 Cranial Region
SD for task: FU1 Thorax (TR8), Lumbar spine and FU2 Thorax (TR2)
At this point I had to ascertain whether these were also the best corrections for FU3 as I had noted the left foot had pronated in the task. The left elbow was also more flexed during that task.
Before assessing this I did a quick test with my corrected findings so far. With the co-correction of the Cranium/thorax and hip I noted that these corrections corrected the left foot and the left elbow in the task. Although the task was unweighted, the testing position mimicked the position of the wrist and while holding onto the bar. The task may have been different with a weighted bar in the Mrs B’s hands for the both the elbow and the foot. However, I had a good correction of the task, the left elbow, and the left foot with the co-correction of the left hip, thorax (TR2), and cranium. I was happy to move on in this session.
Further Analysis of Drivers
The Cranial Region: Cranium
Further assessment of the cranium was done using an active and passive mobility test. As the movements of the cranium are involuntary or passive, it is not necessary to test the active control and passive control of the cranium.
Active Mobility Test
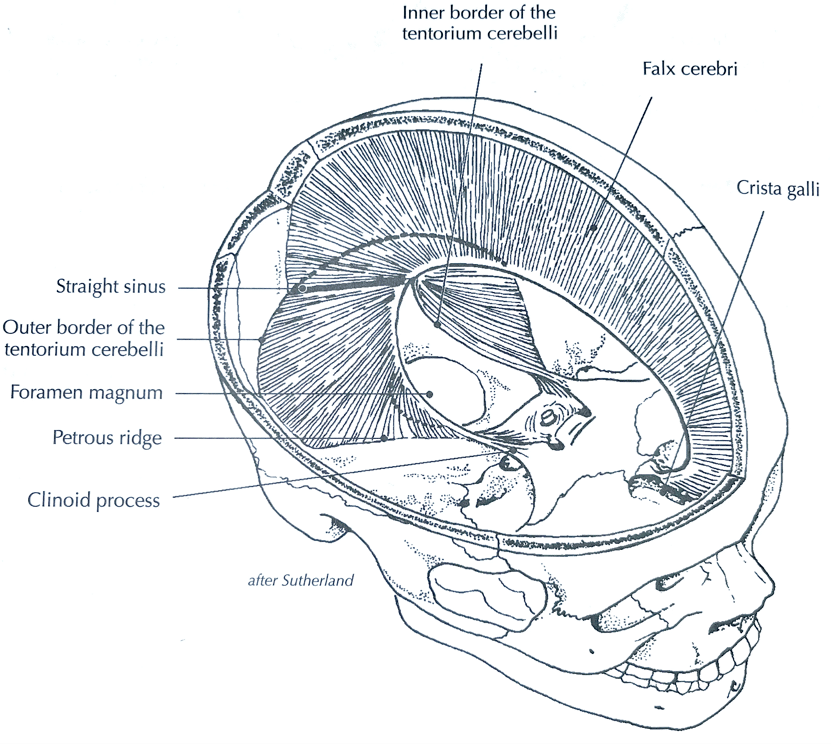
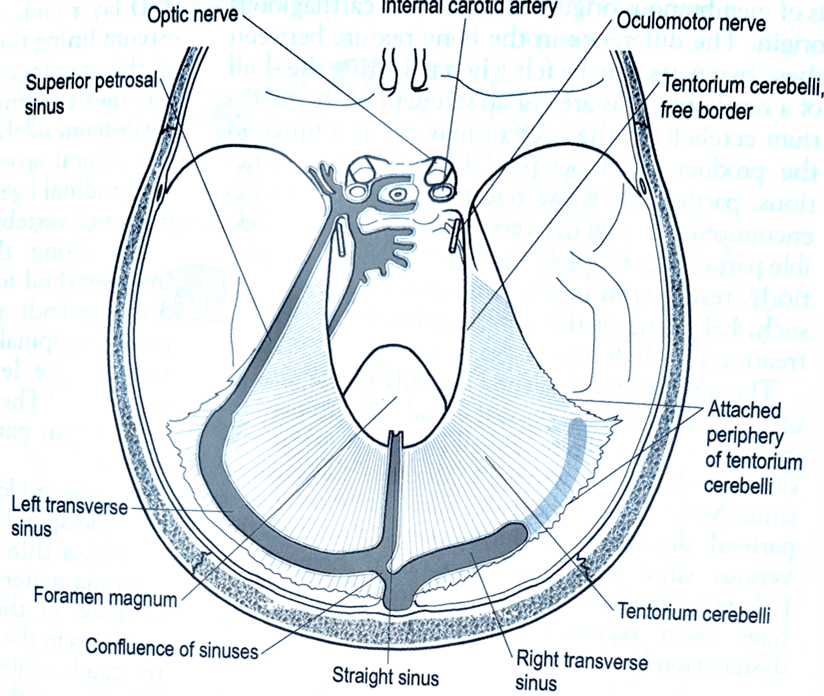
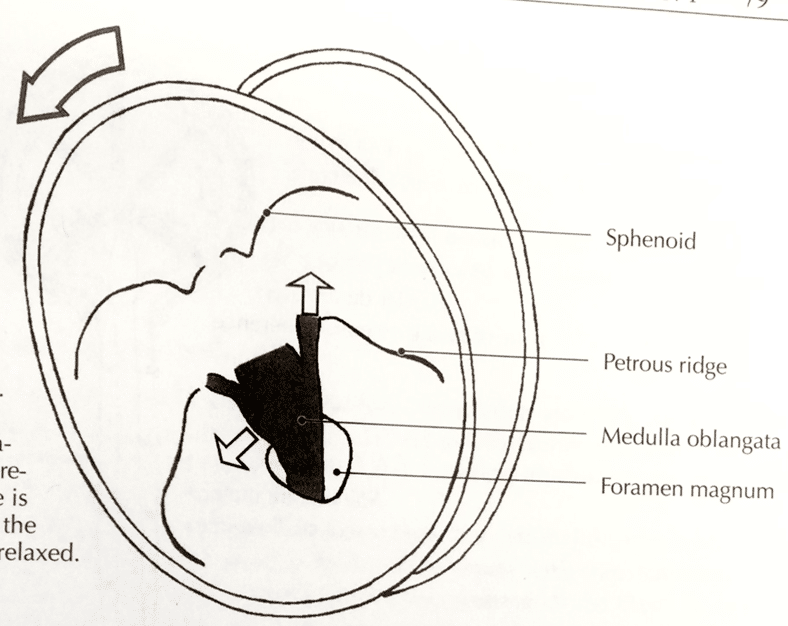
From the work of W.G. Sutherland, it has been theorised that the bones of cranium move in the living organism, (Barral and Crobier, 1999; Liem, 2004; Surgueef, 2007; Sutherland, 1990; Stylian, 2022; Upledger and Credevoogd, 1983). This movement is palpated as a rhythmic cyclic phenomenon called the primary respiratory mechanism, (Barral and Crobier, 1999: Liem 2004; Surgueef 2007: Sutherland, 1990; Stylian, 2022). It is divided into two phases: inspiration and expiration. During inspiration, the midline unpaired structures of the skull and move in the direction of the foetal curve as the nervous system coils; this is named cranial flexion, (Surgueef 2007: Stylian, 2022). The paired structures, for example the temporal bones, move in external rotation, (Surgueef 2007: Stylian, 2022). During expiration the midline structures move in the direction of craniosacral extension, while the paired structures move in internal rotation as the nervous system uncoils, (Surgueef 2007: Stylian, 2022).
The movements of these bones can also be felt and seen during movement, (Lee, 2018). As such it is necessary to assess how and when the cranial bones move during the meaningful task, if it is a driver. This is achieved by assessing the anterior and posterior rotation of the temporal bones and the position of the sphenoid during the task. For the purposes of keeping consistent language within ISM, the terms for motions of the cranial bones have been replaced so that they are like the pelvis. Therefore, the cranial motions are as follows:
Temporal bone
a) Anterior rotation (ISM) = external rotation (Osteopathy)
b) Posterior rotation (ISM) = internal rotation (Osteopathy)
Sphenoid bone
a) Nutation = flexion or inspiration of the skull
b) Counternutation = extension or expiration of the skull
- Diane’s comment:
Thanks for explaining and integrating all this Stuart, wonderful to have in a case report. Now then, I’d like to clarify the integration a bit particularly for the midline bones. In Sutherland’s osteopathic terminology, the flexion phase (inspiration or coiling) has the sphenoid and occiput moving in opposite directions around a coronal axis through each bone, not the sphenobasilar symphysis, yet the motion of each bone is called flexion. This confused me for ages! Consider sagittal plane motion of the spine, forward movement around a coronal axis is typically called flexion and backward motion extension. In the sacrum forward motion is called nutation and backward motion counternutation. So you will find in ISM writings, I have called the forward movement of the sphenoid in the flexion phase, nutation, and the backward movement of the occiput in the flexion phase, counternutation to keep the terms of the midline bones in the pelvis the same as the cranium. The innominates anteriorly and posteriorly rotate as do the temporal, parietal and frontal bones since they are all lateral bones. The metopic suture of the frontal bone responds like a ‘crease’ in cardboard for this motion to occur after the suture appears to have closed.
- Stuart’s response:
This is where my hat really goes off to you Diane. Of all the reading I have done on the cranium, no one has coupled the cranium with movements elsewhere in the body like you have. The fact that I can clinically assess the position of the cranium against the position of the cranio-vertebral joints and assess that in relation to the other body units is amazing. Also, keeping the language consistent has also made it far less intimidating to assess. Furthermore, the fact that you can assess findings in the cranium and have them completely change by changing a caudal driver is also amazing. The ISM assessment process really stops you from looking at everything with a bias from a skill you might have learned recently.
For example, I have seen patients who have been having repetitive treatments done to keep their symptoms at bay (e.g., visceral, or cranial work). Yet when assessing them I have found a driver that was neither cranial nor was the primary vector visceral. For example, I had a patient with a foot driver and articular thorax driver from an old traumatic ankle injury. This was driving their cranial/visceral findings. Once those were treated, their visceral and cranial findings were able to be resolved. They had visceral and cranial findings (liver irritation from a TR7 articular restriction, and a subsequent ventral Vagus nerve irritation that was causing a cranial torsion). So, the previous therapist was not wrong in what they were treating; the patient did have those findings. However, they were a symptom of another issue that had worsened over time.
- Diane’s response:
So much clarity comes when we are able to blend models. We all see the same patients and when we are allowed to dive deep into other profession’s approaches, the clarity only improves, and this can’t help but improve our patient outcomes.
Mrs B’s cranium began in a right ICT with an incongruently left rotated sphenoid. The left temporal bone was anteriorly rotated relative to the right which was posteriorly rotated. During the deadlift task the right temporal bone moved further into posterior rotation and left temporal bone into further anterior rotation. The sphenoid remained rotated left relative to the temporal bones.
An active mobility test of the cranium involves rotating the cranium left and right to end range head and neck rotation to assess the motion of the temporal bones in the transverse plane. At the end range of head and neck rotation there should be rotation of the temporal bones relative to the direction of rotation.
- Diane’s question:
When the head and neck rotate to the left, what is the ‘rotation of the temporal bones relative to the direction of rotation?’
- Stuart’s response:
Left rotation: Left temporal bone rotates posteriorly, right temporal bone rotated anteriorly.
In Mrs B’s case there was no posterior rotation of the left temporal bone when she turned her head to the left. Similarly, there was limited anterior rotation of the right temporal bone when turning left. This coincides with the restriction of left head and neck rotation noted in the screen for head and neck rotation during the quick screening task.
Passive Mobility Test
The passive mobility test is used to assess the ability to de-rotate the temporal bones and sphenoid and bring the cranium into a neutral position. It is also used as a passive listening test to assess what vectors of pull are acting on the cranium. This helps to determine whether the vectors acting on the cranium are intracranial or extracranial. This test involves distracting the temporal bones laterally and then bringing each temporal bone into a neutral position relative to the ICT. As the sphenoid is incongruently rotated to the ICT, it is also necessary to bring the sphenoid into a neutral position relative to the temporal bones. Then a release and listen is performed to ascertain which bones moves first and where it gets pulled to.
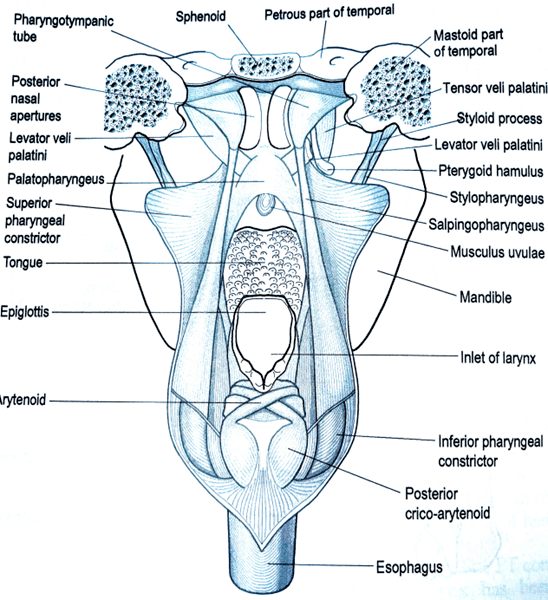
Figure 3a – Superior attachment of the pharyngobasilar fascia (Barral and Crobier, 1999)The third finger of the left hand was used to direct the sphenoid out of left rotation by distracting the left greater wing of the sphenoid from the left sphenosquamous suture.
Then, the left temporal bone was distracted and rotated posteriorly, while the right temporal bone was distracted and rotated anteriorly.
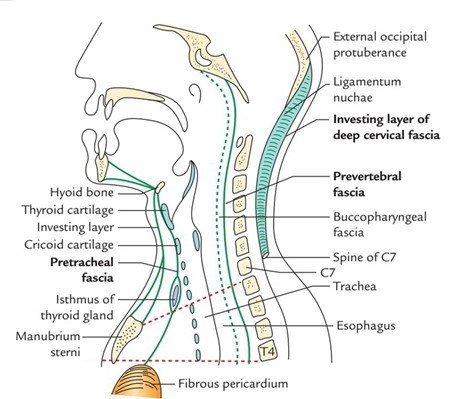
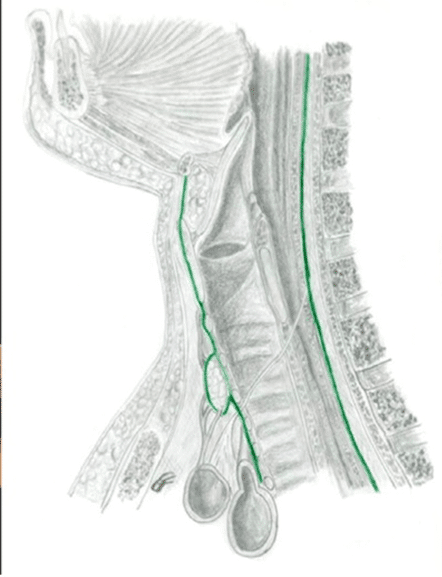
Upon release of this correction, the first bone to move, and thus the strongest vector, was on the left side of the sphenoid. The sphenoid was drawn back towards the left temporal bone into left rotation and nutation from an inferior vector coming from a caudal pull from pharyngobasilar fascia and even more caudally via the buccopharyngeal fascia towards TR2. This confirmed my thinking there was a connection between the cranium and TR2 that was deep to the muscular vectors that would normally affect TR2. The attachment and anatomy of this can be seen in figures 3a,b and figure 4a,b,c,d.
- Diane’s question:
What do you hypothesize the vector to be when the passive listening draws the sphenoid into left rotation (intracranially) but not inferiorly?
- Stuart's response:
Stuart’s response: The structure that could pull the sphenoid into left rotation is the anterior attachment of the cerebelli tentorium where it attaches to the posterior clinoid process. This can be seen in the figures 5, 6 and 7 below.
Figure 5 – The reciprocal tension membranes (Barral and Crobier, 1999
Figure 6 – Attachment of the Tentorium Cerebelli (Sergueef, 2007)
Figure 7 – Tension on the cerebelli tentorium with left rotation (Barral and Crobier, 1999). During a twisting or rotation dysfunction of the dural membranes the tentorium cerebelli will move caudad on the side where the occipital bone is lowered and cephalad to the opposite side (Liem 2004). The tentorium will also move towards the side of convexity, which is the side of dysfunction, (Liem, 2004). However, I think the above statements assume there is not an incongruency between the temporal bones and sphenoid. Also, with a right intracranial torsion the posterior portion of the cerebelli tentorium is stretched, (Barral and Crobier, 1999).
The second vector felt was the left temporal bone getting pulled into anterior rotation by the left temporomandibular joint.
- Diane’s question:
How does a joint create a vector? Are you meaning tight ligaments and capsule of the left TMJ where pulling the temporal bone into anterior rotation relative to the mandible? I’m not sure I’ve ever felt this one!
- Stuart's response:
Yes, that is correct. The articular capsule attaches from the condyle of the mandible to the temporal bone (Liem, 2004). The capsule is also continuous with the lateral pterygoid muscle, masseter and temporals muscles, (Liem, 2004). This would cause a laterotrusion of the mandible from repetitive contraction of the lateral pterygoid (superior part), posterior part of the temporalis and deep portion of the master, (Liem, 2004).
Figure 8 – Articular Capsule (Liem, 2004) A restriction of the condyle in a lateral position does the following to the cranium (Liem, 2004):
- Asymmetric motion of the temporal bones
- Compression of the parietotemporal suture
- Torsion of the tentorium cerebelli
- Lateral displacement of the hyoid bone
This can be seen in Figure 9.
Figure 9 – The effects of a lateral restriction on the cranium (mandible rotated to the left in the transverse plane) (Liem, 2004)
There was also a vector felt acting on the right temporal bone as it moved into posterior rotation that was intracranial. I hypothesised this to be the right cerebellar tentorial membrane.
That concluded the assessment of the cranium as there were no further tests for the cranium.
These findings suggest the following structures would require release in the following order:
- Buccophragyngeal/Phrayngobasilar fascia vector
- Anterior Left cerebellar tentorial membrane at the posterior clinoid process
- Articular capsule of the left TMJ
- Right cerebellar tentorial membrane at the right transverse sinus
Further Assessment of the Left Hip
Further assessment of the left hip included active mobility, passive mobility, active control, and passive control tests.
Active Control
As was noted in the screen task the left hip translated anterior relative to the left acetabulum and lost centre in the first 20% of the movement.
Active Mobility
The left and right hips were palpated as the patient was taken through flexion, extension, adduction, and abduction in the position of loss of control noted in the task in standing. It could be felt that the hip did not want to extend or adduct very easily in this position. This is similar to the finding in the screening task confirming there are vectors acting on the hip as the hip loses control.
Passive Mobility
This was conducted in supine. The femoral head was palpated as the left hip was taken into flexion. This is similar to the screening task. In this assessment the femoral head translated anteriorly in the first 20 degrees of movement. This coincides with the loss of control during the task.
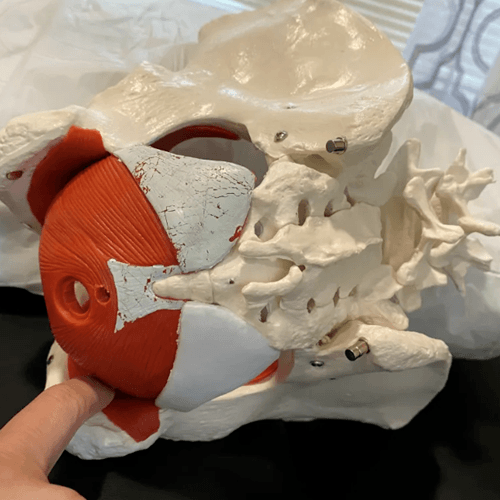
Once it was established where in the range of motion the femoral head lost centre, a passive listening test was performed to assess what vectors were acting on the left femoral head. After stabilising the left side of the pelvis, the left femoral head was manually translated laterally and then posteriorly, to centre the head of femur, and then this position was released to determine the location, length and strength of the relevant vectors. From this it was established there was a vector coming from inside the pelvis, in the pelvic bowl, that directed up towards the left ovary where a surgical scar was located. There was also a secondary rotational vector coming from obturator internus.
As the hip vector drew my attention to the abdominal pelvis I also used a Barral local listening test at the deduced point of termination of the vector. I found there to be a scar tissue restriction at an incision point from the abdominal surgery Mrs B mentioned in her story. The vector extended towards the sigmoid colon, and the sigmoid colon extends down toward the acetabulum, (Barral, 2005). The left ovary sits deep to the sigmoid colon, (Barral, 2005). This local listening test helped me to establish the connection between the hip and abdomen.
- Diane’s comment:
Such a lovely integration of models, yet again!
Passive Control
This was not conducted as there was nothing in the history indicating this test was necessary.
- Diane’s comment:
I would disagree with this statement Stuart. Whenever anterior translation of a femoral head relative to the acetabulum is noted, I think a passive control test for the anterior labrum and capsule is warranted.
- Stuart's response:
Again, now you have mentioned that it seems glaringly obvious that I should have done that.
The patient never complained of hip pain at any point in her history. I think that is why I thought it was not necessary to test. But when you consider the biomechanics of the joint position, I can see what you mean.
These findings suggest the following structures would require release in the following order:
- Intrapelvic vector coming from surgical incision site
- Obturator internus vector
Further Assessment of Secondary Drivers - The Thorax: TR8
Further assessment of TR8 was conducted as I suspected there were articular restrictions within this thoracic ring. This was deduced during the meaningful task assessment and in standing before assessing the left hip and cranium. As this was not a primary driver, I needed to screen this quickly and treat the relevant articular restrictions in the thoracic ring. Then I could assess its relationship in relation to the task and the drivers I had found so far.
I chose to do this after I had assessed the other functional units as a partial correction of TR8 was not indicating it was a primary driver.
Active Mobility
The osteokinematics of TR8 were noted during the meaningful task. The 8th thoracic ring was held in right translation and left rotation. It did not change during the task. No other active mobility test was performed as the thorax remains neutral during the meaningful task. Had Mrs B had issues with running for example, I would use rotation as part of the active mobility test for the thorax.
Passive Mobility
The screening test ascertained that TR8 felt very stiff when trying to correct it. This suggested there was an articular system impairment as opposed to a visceral system or neural system impairment.
- Diane’s question:
Passive listening both during the attempted correction and on release of the correction would also provide a finding that would suggest an impaired articular system vs visceral or neural. What would the listening be like to further validate going into the articular system tests for TR8?
- Stuart's response:
An articular vector also has a very short and definitive stop upon release of the correction. This indicates the vector is very close to the joints of the thoracic ring. A neural system impairment would have longer smoother directional vector of pull depending on the structures acting on the thoracic ring. A visceral system impairment would have an intrathoracic vector of pull that would direct itself towards the midline of the body and then superiorly or inferiorly depending on the structure. For example, the liver has a very long and heavy pull into the thorax usually from the right side of the thorax. The stomach has a waftier type of pull from the left side of the thorax. When there is a long vector involving multiple structures, you can feel the pull snake its way through the patient and terminate somewhere that makes your brain go “huh? Ok”. Then you get out some anatomy pictures and try to reason what you feel with some relevant anatomy.
The articular system was assessed using the following tests:
a) Inhalation/exhalation while palpating the costotransverse (CT) joints at TR8. In the vertebrochondral region this is used to assess the anterior, lateral, and inferior (ALIF) glide of the CT joints in inhalation. Then the posterior medial and superior (PMS) glide of the CT joints in exhalation.
- Diane’s question:
Since TR8 was held in left rotation/right translation IF there were NO restrictions of the CT joints, the starting position of these joints would be asymmetric and could possibly yield a false positive. Is the right 8th rib more posteromedial superior or anteroinferiorlateral in this starting position? Is the left 8th rib more posteromedial superior or anteroinferiorlateral in this starting position?
- Stuart's response:
As the ring is rotated to the left and translated to the right the following should happen if there are no articular restrictions acting on the CT joints:
The right rib: The articular surfaces of the rib would glide into more posteromedial superior glide
The left rib: The articular surfaces of the rib would glide into more anterolateral inferior glide
- Diane’s response:
We need this information to interpret the arthrokinematic findings. For example, if when passive mobility testing the CT joint arthrokinematic glide on the right you found the PMS glide to be more limited than the ALI, you would have to question if this joint was the relevant articular restriction for the ring because its starting position is more towards PMS and it should be more limited if this is a positional finding and not an articular restriction.
b) Flexion and extension of the thorax while palpating the 4 associated transverse processes of the zygapophyseal joints at thoracic ring 8.
- Diane’s question:
Since TR8 was held in left rotation/right translation IF there were NO restrictions of the Z joints the starting position of these joints would be asymmetric and could possibly yield a false positive. Is the right Z joint more flexed (superiorly glided) or extended (inferiorly glided) in this starting position? Is the left Z joint flexed (superiorly glided) or extended (inferiorly glided) in this starting position?
- Stuart's response:
As the vertebral body is rotated to the left and translated to the right the following should happen:
The right z-joint should be more superiorly glided (flexed)
The left should be more inferiorly glided (extended)
The testing yielded a restricted right costotransverse joint in ALI glide. The right T7-8 Z-joint was restricted in extension, meaning there was a restriction in inferior glide of the 7th vertebrae on the 8th on that side. The left T7-8 Z-joint was restricted into flexion, meaning there was a restriction in superior glide of the 7th vertebrae on the 8th on that side.
- Diane’s comment:
Therefore, within this thoracic ring, there are 3 joint restrictions to address since the limitation of motion is consistent with an articular restriction and not a positional finding.
Active Control
During the meaningful task assessment, a partial manual correction of TR8 corrected TR7; however, it did not change at all during the task.
- Diane’s question:
Not sure you can test this when there are articular restrictions. Active control testing is done when there are no longer any vectors restriction mobility and a given load cannot be controlled.
- Stuart's response:
Yes that is correct. What I wrote would be related to active mobility. I have actually seen this in a few patients. After releasing the articular system and muscular vectors acting on a ring they are unable to maintain optimal biomechanics of the ring when the ring was placed under load.
- Diane’s comment:
Yes but these vectors have not been released yet in this patient. Therefore, at this point in the assessment I don’t think an Active Control test was required.
Passive Control
This was not tested as nothing in the history suggested this was necessary.
Treatment
Releasing Beliefs and Gaining Understanding
Since Mrs B had come in with back pain that had been created by a back exercise, it was necessary to educate her as to why treatment of her cranium would be necessary to help her low back pain. For her, the cranial correction was the most confusing part of the assessment. Although she could feel her cranium was part of the meaningful task assessment, she still didn’t understand the why. Mrs B had noted stress as being a significant factor in the lead up to the injury, so she was open to the fact that it was somehow related. She had already heard of the methods of ISM assessment from other peers at the gym, so was intrigued, and not at all surprised, by the seemingly “outside the box” approach.
To help connect the dots, Mrs B was educated around the effects of the muscles of jaw acting on the cranium and the dural system both within and outside the skull, as well as the effects of the sympathetic nervous system on the dural system. I also showed her how muscles attached from the pelvis and lumbar spine and inserted onto the thorax. This helped piece together why we might have needed several corrections in the body to get a good correction for the task. I have found using visual aids quite useful in at least getting patient’s onboard with the idea of interregional connections.
At that point Mrs B was ready for treatment. Addressing the cognitive beliefs through education and explanation helped to put her at ease.
- Diane’s comment:
This is too important of a point to not pause and reflect on what Stuart has done here. Bialosky et al wrote an excellent paper in 2010 on patient’s expectations and the importance of this expectation on outcomes. Unless the patient understand the how and why different impairments are related, they may just think ‘you are nuts’ and not come back, especially if you haven’t been able to completely change their experience of the task when there are multiple drivers, as there are in this case. Gaining trust, and building relationship is critical at this stage. Sometimes, we can’t always know how things are connected/related and that’s OK as long as we can show them via visuals, anatomy or experiences that they are.
Bialosky, J. E., Bishop, M. D. & Cleland, J. A. Individual expectation: an overlooked, but pertinent, factor in the treatment of individuals experiencing musculoskeletal pain. Physical therapy 90, 1345–1355 (2010).
Release
Thorax – TR8: Articular System
The articular restrictions at TR8 were treated first.
- Diane’s question:
OK, I need you to justify why you chose to treat a secondary driver first. The principles of ISM suggest that primary drivers are treated before secondary ones. However, I can think of a reason why you might have decided to start with this secondary driver and I’m curious what your reasoning was.
- Stuart's response:
I wanted to know if releasing the 8th thoracic ring would change the control of the lumbar spine. Due to the rotation and translation of the 8th thoracic ring you could hypothesise the articular restriction was created by overactivity of either the left longissimus or iliocostalis or both. Therefore, releasing the 8th thoracic ring may change the nervous system’s response to loading. The release could improve the motor control of the intrinsic system overall. This might negate the lumbar spine as a secondary driver.
As TR7 and TR8 were translated in opposition to each other, the release of the 8th thoracic ring may have also changed the behaviour of the dural system and autonomic system. As the sympathetic chain sits right in front of the vertebral body, a constant twist at this level could be quite stressful for the autonomic system, see figure 10, (Barral and Crobier 1999). The rotation at TR7/8 could also create tension on the dura, which upon release may improve the inferior vector felt on the cranium. As the stomach and liver can act on these rings, the release of the ring may also yield changes in tension placed on the ventral vagus nerve, the phrenic nerve and dorsal vagus nerve, see figure 11 (Barral 2020; Barral and Crobier 2013; Barral and Crobier 1999; Marlien 2021). The mid back stiffness was a part of Mrs B’s story, so releasing an articular restriction there would yield at least some relief and encourage Mrs B that I knew what I was doing. This would help build trust.
Figure 10 – The sympathetic chain at TR8 and TR9 (Barral and Crobier 1999)
Figure 11 – The autonomic nervous system in the abdomen (Shuenke et al. 2010) - Diane’s comment:
Yes, it really is to determine what impact a complete correction of TR8 would have on the others. Great reasoning here.
The 3 joint restrictions in TR8 were released using a vector-specific grade 4 sustained glide into their relative barriers of restriction e.g., restricted ALIF glide right CT joint, superior glide left Z-joint, and inferior glide right Z-joint. Essentially finding the “string in the spring” for each joint, until the articular barriers were released, (Lee, 2018). As mentioned in the assessment, there was a question mark over this thoracic ring’s impact on correcting the other drivers. After release, a quick screen was used to establish what had changed. It was noted there was now a dominant neuromuscular vector acting on TR8 that behaved in a similar pattern to the first screen. It allowed a full correction of TR7, but still did not change the hip and cranium as the best overall corrections. The left hip, TR2, and cranial correction also gave a correction of TR8. After this release; however, Mrs B noted she no longer felt tight in her mid-thorax, which was part of her story and meaningful complaints.
Due to an intuition from the story and assessment that there was a connection between the left hip and cranium via the deep fascial system, it seemed appropriate to treat the restriction in the left hip first.
- Diane’s comment:
I’m not sure it matters which PD you treat first as long as you treat both in the session.
Left Hip – Neural system
With the patient in crook lying the vector from the abdominal pelvic scar was released first by following the direction of resistance of the fascial barriers around the scar and into the pelvis. This was followed by a release of the sigmoid colon using the left leg as a long lever. While holding the visceral vector in the sigmoid colon the left femur was taken into extension until the barrier between them let go. As mentioned before, the left ovary sits behind the sigmoid colon, so this release made sense as being a barrier to hip mobility, (Barral 2007b). Vectors coming from the sigmoid colon can also have an impact on the biomechanics of L4/5 and L5/S1, which could explain the odd findings with the lumbar spine during initial assessment, (Barral, 2005; Barral, 2007b; Barral and Crobier, 2012).
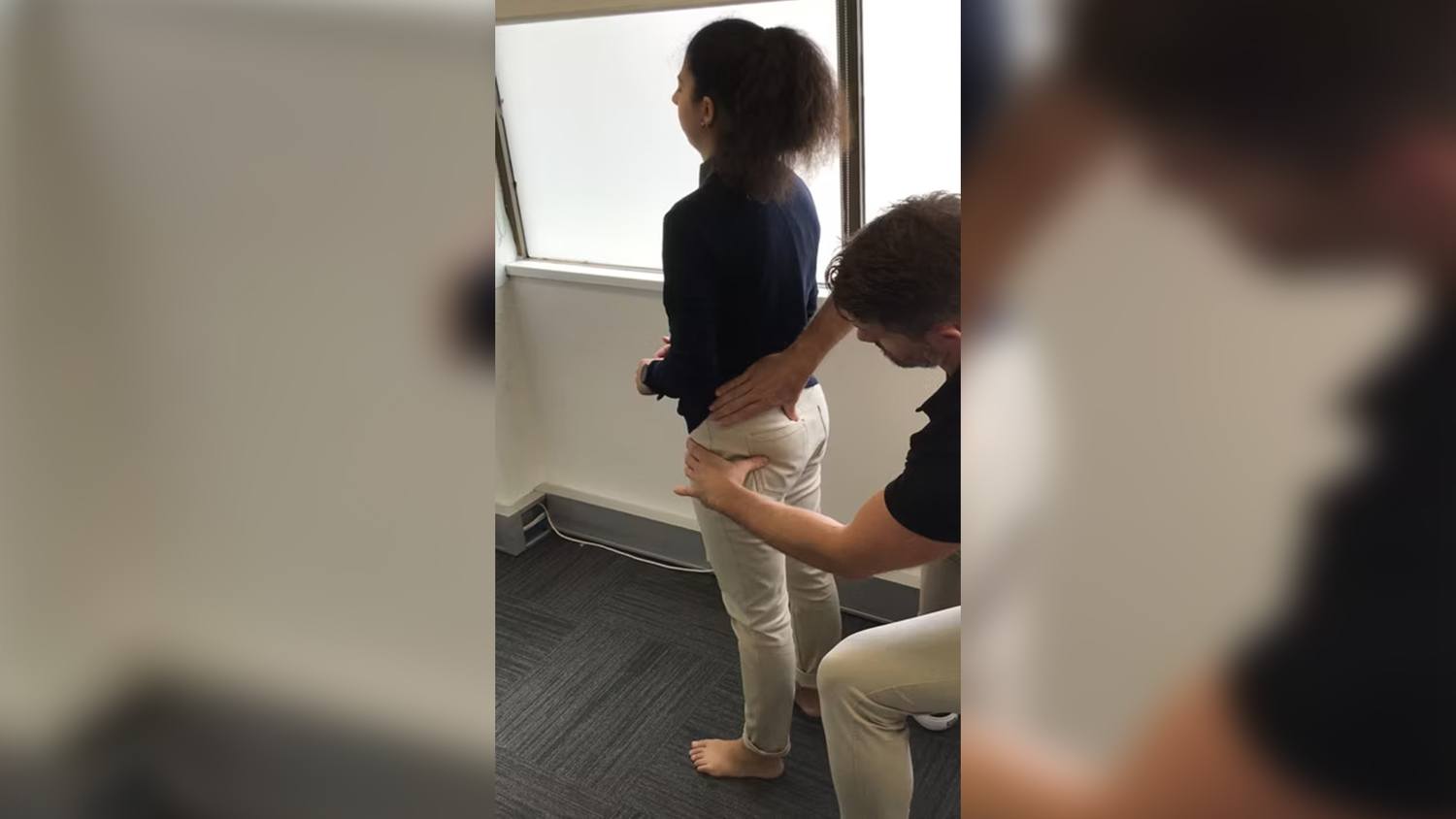
The obturator internus vector was released in side-lying using an external trigger point release on the body of obturator internus where it sits over the obturator membrane.
- Diane’s question:
Are you palpating this medial to the ischial tuberosity or through the obturator externus and membrane? I don’t think you can get through iliococcygeus to reach the obturator internus medial to the ischial tuberosity?
- Stuart's response:
I did it like this, see figure 12. I treat it though the transverse perineal muscle and then direct pressure in around the back of the ischium until I can palpate some of obturator internus. It’s probably not quite as effective as an internal release. A bit like obturator externus release through the pectineus; it’s hopefully enough to get the nervous system to let it go. I always re-assess to see if I get enough of a change of tone to have an impact on the task. If it keeps coming back as a dominant vector, I will refer them out to Amy Greenlees, who is an ISM women’s health therapist in Sydney, as they fall into a category I can’t fix. Though I have found the way George taught us to release it in crook lying with breathing a lot more effective. Increasing the pressure on the tissue as they patient breaths in allows you to sink into obturator internus a lot better. I have been able to successfully release some very stiff SIJ’s with this technique. Though part of the release I’m sure is also through release of iliococcygeus.
Figure 12 – Side lying palpation of obturator internus - Diane’s comment:
Yes, this is the same technique we did in Part 2 on our pelvic floor day. You are way posterior to the Superficial Transverse Perineal muscle and over the inferior part of OI inferior to the obturator membrane.
Cranial Region: Cranium – Myofascial system
With the left hip vector released, a quick reassessment of the cranium with a passive correction/release and listen indicated the vector now had less caudal pull on the sphenoid and seemed to be more at the sphenobasilar symphysis.
- Diane’s question:
How do you hypothesize a vector can reach the sphenoid from the ovarian scar?
- Stuart's response:
My hypothesis for that is the following:
- The vector going to the left side of the diaphragm (first part of vector in the peritoneum) could have occurred in the following ways:
- The scar from the portal entry creates a vector down to the ovary and sigmoid colon that draws on the ligamentum teres and falciform ligament of the liver that created an inferior medial shift in the liver which, among other things, draws on the attachment of the left triangular ligament (Barral, 2007).
- Or the path they took where they would have moved the sigmoid colon to get to the ovary creates a vector of pull that acts of the colon, that then extends up via the ascending colon to its attachment at the left hemidiaphragm via the phrenicocolic ligament (Barral 2007). The phrenicocolic ligament also attaches to the spleen, and the gastrocolic ligament connects the stomach to the spleen and transverse colon. The spleen could then act as a vector of pull on the diaphragm.
- Or it creates a restriction in the sigmoid fascia that extends up to, and is anterior to, the abdominal aorta, (Barral 2007). This could irritate the inferior mesenteric ganglion or superior hypogastric plexus. This can irritate the ascending and transverse colon creating spasm which puts pressure on the ligamentous attachment of the ascending colon as mentioned before (Barral 2020).
- The inferior vector acts on the left leaflet of the central tendon of the diaphragm (Barral, 2020). This creates a spasm in that portion of the diaphragm as the nervous system attempts to minimise the inferior pull.
- This creates a vector of pull that acts on the mediastinum/pericardium which then pulls on up into the neck via the buccopharyngeal fascia terminating at the attachment point of pharyngobasilar fascia. The attachments of the pericardial ligaments could be where the vector from TR2 is coming from, along with the deep fascial lamina from the neck.
- The extra cranial compression from the nightly bruxism and the left deviation of the TMJ creates a stronger vector on the left side of the sphenoid/temporal bone and SBS. Possibly, the bruxism made the left articular capsule stiff. This draws the hyoid laterally adding to the pull created from below. This then creates the twist in the cranium. Possibly the body was coping with this before. However, the extra sympathetic nervous system activity creates a situation where the system can no longer cope with added stress (e.g. exercise fatigue). Finally, the extrinsic system can no longer cope with the compensating for the hip/pelvic/lumbar spine instability. Hence the back pain doing a deadlift when the system is fatigued.
The only thing I can’t figure out is why the cranium was in a RICT. Everything should pull it into a LICT. The other thing that could be involved causing the vector from the left diaphragm is the ventral Vagus nerve. It sits on the caudal side of the diaphragm and passes through the crus of the diaphragm. It passes through the jugular foramen and attaches to the medulla oblongata. So that could potentially create another intracranial twist. I have treated a few patient’s in the past who have had a RICT, but the left ventral Vagus nerve is the vector that needs to be treated to fix it. There are still years of anatomy learning ahead to understand the relationships! When you see how much things move within the body just with breathing, these internal vectors make more sense. And it doesn’t seem so far-fetched that you can have an intrapelvic vector pulling on someone’s cranium.
The main thing I will note here, though, is the power of ISM in not letting you get lost. I am not certain I would have treated Mrs B as effectively if I just relied on palpation or listening. So the fact that I can layer visceral listening into the ISM system and not feel confused gives you, and the patient, a lot more confidence to find the little things that will make a big difference.
- The vector going to the left side of the diaphragm (first part of vector in the peritoneum) could have occurred in the following ways:
The SBS was released by stabilising the occiput and taking the sphenoid into further compression with increased left rotation and nutation and waiting for a change. Stylian (2022) and Barral and Crobier (2019, 1999, 2007a, 2007b) agree that it is often better to take the barrier of restriction into a direction of ease before taking into a direction of tension. Once a change was felt, the sphenoid was taken into right rotation and counternutation while stabilising the occiput. The pharyngobasilar fascia attaches to the basilar part of the occiput, the lower part of the posterior sphenoid and to the petrous portion of the temporals, (Barral and Crobier, 1999). As mentioned by Barral and Crobier (1999), these superior insertions cross over the sphenobasilar symphysis, which explains the consequences of a caudal vector on the cranium.
- Diane’s question:
So, this isn’t a SBS (sphenobasilar symphysis) strain lesion then? My question above remains and may be answered by now. How does this vector get to the ovary?
- Stuart's response:
The strain from the inferior fascial restrictions lead to the compression of the SBS. So, it was an SBS lesion, created by an inferior visceral vector as well as an intracranial vector. However, once the long vector was taken care of the SBS lesion remained, meaning it needed to be treated as well. However, had I not taken care of the caudal vector it would likely have come back. Also, I’m not sure if releasing this first would have yielded good results. It may not have let go.
- Diane’s comment:
I meant it wasn’t a non-physiological strain lesion of the SBS but a compression lesion that could be addressed by releasing a long vector and not the symphysis itself.
A passive correction of the cranium yielded a vector from the left TMJ, impacting the left temporal bone. The temporal bone on the left was immediately drawn anteriorly on release. This remained after the release of the sphenoid, which was now congruent with the cranium. The left TMJ was release intraorally by mobilising the barriers of resistance in the articular capsule. The superior part of the lateral pterygoid attaches to the articular capsule and to the sphenoid, which can be treated by treating any articular barriers in the capsule of the TMJ, (Fernandez-de-las-Penas and Mesa-Jimenez, 2018;, Liem 2004). A fascicle of the masseter muscle was released along the posterior portion of the zygomatic arch.
- Diane’s question:
Why? What lead you to this muscle? It has not been named as a relevant vector to this point. Was there a tender point or a vector of further restriction on the left temporal bone?
- Stuart's response:
The left temporal bone was still getting drawn anteriorly with a passive correction of the cranium. Palpation of the TMJ and towards the zygomatic process of the temporal bone yielded a stiff fascicle of deep masseter.
The deep part of masseter attaches to the posterior one third of the zygomatic arch and to the articular capsule, which would explain the vector acting on the left temporal bone, (Liem, 2004).
- Diane’s question:
Good hypothesis; however, did you feel the direction/location of this vector with a passive mobility test of the temporal bone? Every treatment we do must have an assessment test and clinical reasoning to justify it in ISM.
- Stuart's response:
Yes I would correct the cranium by bringing the temporal bones to midline. Once the inferior vector and SBS were treated, the sphenoid was congruent with the cranium. The temporal bones remained in a right ICT. After each treatment I would correct the cranium, release and listen. I would follow the first dominant vector that act on the cranium. At this point it felt like the deep masseter.
The remaining vector that remained with a passive correction of the cranium indicated the right tentorial membrane was restricted near the right transverse sinus at the parietomastoid suture. Upon a release and listen I could feel the right temporal bone get drawn back into posterior rotation. The left temporal bone rotated anteriorly after the right temporal bone began to rotate posteriorly. The right temporal bone held the dominant vector acting on the cranium. A restriction in the right tentorial membrane was acting on the right temporal bone.
This was released by stabilising the occiput and firstly rotating the right temporal bone into more posterior rotation until a release was felt, and then rotating the right temporal bone into anterior rotation. This could have been a remnant of the restriction felt at the sphenoid and left temporal bone initially via the twist it would have created in the falx and then into the posterior attachment of the right tentorial membrane, (Liem, 2004; Surgueef 2007: Stylian, 2022).
After the treatment was finished Mrs B was re-assessed. She felt much better, and far more relaxed. During the meaningful task assessment, The left hip was the first site of impairment followed by the left SIJ, and then L5. The left hip was now anterior to the right but did not translate anterior to the acetabulum, the left SIJ unlocked at the end of the task after the left hip, and L5 rotated to the right as the SIJ unlocked. The rotation at L5 was less when compared to the initial screening. She was not fully stable but was significantly improved.
The findings in the thorax (FU1 and FU2)/cervical spine and cranium were also gone. The foot, again, pronated with the hip losing control. The arm had corrected as the shoulder girdles were neutral.
Align
No taping was required for Mrs B post session as a connect cue was adequate for pelvic control in the task. Had Mrs B been in pain or needed to deadlift in the near future, I could have taped the hip into a posterior glide to facilitate more optimal biomechanics.
Connect
Given the left hip, left SIJ and L5 were still not full corrected in the task, I deduced there was a lack of coordination between the muscles of the pelvic floor, TrA and the sacral/lumbar fibres of deep multifidus. With time being quite short at this point in the treatment session I chose a cue for contraction of the pelvic floor to try to correct the remaining findings. A cue for a “20% lift of pelvic floor” improved the loss of control of the hip, SIJ and L5 in the meaningful task.
To try to find effective connect cues for the abdominal wall or pelvic floor I will often use a percentage of effort or score out of 10 to obtain an optimal contraction. Through experience I have found that when patients are left to their own devices they will often try “too hard” to recruit, for example, TrA. By giving the patient’s a quantifiable measure that ties in with the best visualisation cue, I have found this helps to achieve better outcomes. In Mrs B’s case, a “lift” cue for pelvic floor was enough to illicit a contraction of the lower fibres of TrA; however, Mrs B’s initial reaction was to contract too hard leading to contraction of internal oblique (IAO). When given the quantifiable measure of “20% effort”, this corrected the over recruitment of IAO. I chose this cue for the following reasons:
- I had treated a part of the pelvic floor.
- Mrs B had an intrapelvic restriction.
- Mrs B had given birth in the past.
- Cueing a pelvic floor contraction should also lead to a co-contraction of TrA.
- Diane’s question:
What about the deep fibres of multifidus at L5? I suspect that the pelvic floor and TrA would control the left hip and left SIJ but not L5 – you likely needed dmf to come on for this. Did your pelvic floor cue result in co-activation of the dmf? This is a super long assessment and treatment session; I would be surprised if you had time to get through all of this in 1 hour!
- Stuart's response:
Yes, that’s why I said I was running low on time/running over a bit. I don’t know if the cue resolved any coordination issues with deep multifidus. It seemed like the best correction at the time as it improved the task and made Mrs B feel more secure in the task, so we just went with it. As I mentioned earlier, it would have been interesting to see if TrA and Dmf were actually coordinating together as that was a hypothesis, I had in my mind for why I couldn’t get a good correction of the lumbar spine.
- Diane’s comment:
With a typical one hour new assessment session, I find I often get to finding the driver(s), start an initial treatment on the primary drivers, and then leave them with a partial home program. I never promise to get into treatment in the first session. If people leave with a better understanding of the relationships between their impairments and that treatment will begin during the next session, then I am happy with what I have gotten done.
Mrs B was then sent home with the following homework:
- Side lying thorax rotation to improve the articular glide in mid thorax.
- Practice hip hinging with a “20% pelvic floor lift” cue each time. Currently she could do 5 reps before feeling fatigued in the pelvic floor and losing control of the hip, which she would palpate as she did the hinge movement. Her goal was to be able to do 3 sets 15 reps with at least 1-2 minutes rest between sets.
- Deep box breathing (with a 4 second count in/hold/out) before bed.
- Diane’s comment:
Interesting that in the session you released a left hip to pelvis vector but didn’t give any homework to maintain this even though the left hip was a co-driver with the cranium and TR2 (was TR2 treated at all, or did it release with the cranium or something else? It seems to have been dropped here). You released multiple vectors in the cranium for the sphenoid, left and right temporal bones with no homework to maintain this release. The homework for release maintenance was for TR8 which didn’t have much of an impact on anything else? Additionally, you gave her a connect cue and movement practice which was without a motor control assessment, which is fine for this session when time was running out. I would expect a more complete assessment of the pelvic floor, TrA and dmf on a subsequent session to confirm your ‘intuition’.
- Stuart's response:
Everything from L5 up seemed to have been corrected with the visceral, cranial work and the release of TR8. I tend to follow Barral’s recommendations with regards to cranial and visceral work in that it’s best to just let the body work itself out. I haven’t found anything so far that creates any meaningful changes between sessions if people are cranial drivers either. I’m certainly open to any suggestions!
- Diane’s comment:
I suppose it depends on what the vector/system impairment is. For articular cranial restrictions (OM or SSP suture) I will teach them a home self-mobilizing technique. For sinus congestion leading to cerebellar tentorium vectors, I will teach them how to drain the system and give them SNS down-regulation practice (much like the box breathing you gave her). For the type of visceral vector, you found – I may have given her a movement practice with a cranial correction whenever she found a task tightening up between sessions that was in relationship to that vector. This is more about empowering people to understand that there are things they can do to treat themselves.
- Stuart’s further comment:
Also, I doubted in a week she would manage to create another long visceral vector or create the same level of compression on the cranium. So, I wasn’t too worried about giving homework for that. As some of the peritoneal vectors terminated at the diaphragm, I figured thorax rotation would also help to mobilise the internal vectors.
I figured thorax rotation and stability exercises for the hip/SIJ and lumbar spine would make Mrs B happy anyway. If the patient has come in quite highly strung about their issues, I will tend to follow the notion of “give them a bit of what they need with a bit of what they want”. Mrs B was quite a complex case, so I chose what I thought were the biggest wins in terms of ease of execution and aligned with her cognitive beliefs. In the past I have found if I try and get too tricky with homework, I can lose the patient.
So, with time pressing, and going on my intuition, I went for what I thought had the biggest chance for success with Mrs B in terms of compliance and for resolution of the issue. Although she understood why I treated her jaw and cranium, I’m not certain she would have been happy with jaw exercises. If I had more time, I would have certainly been happy to get a much clearer picture of what was happening with regards to motor control. But yes, a more thorough investigation of the motor and timing was necessary.
- Diane’s comment:
I think it is important to state for the readers that having an expectation to be able to find every driver, further assess every driver, provide treatment for every driver as well as a motor control assessment and then give them things to do at home is unrealistic. These reports are NOT about a perfect assessment and treatment session. They should be about reality in practice and knowing when a session is complete, even if the assessment or treatment is not – because that is our reality in practice.
- Stuart's response:
I think when you write down all this detail, it seems like I did a lot. But really, the treatments themselves don’t take long. Again, because I can hone in on the driver that has the most impact with ISM I can, for example, do 30 seconds of manual therapy and the person can get up and go “wow I feel so much better!”. But I agree with what you said, you can’t get the patient walking out perfect in one session. Plus, sometimes they come back and there are 10 other things that popped after you released the first layer of dysfunction.
Follow Up Treatment Sessions
A week later, on the second treatment Mrs B said she felt a lot better. She felt no tension in her jaw upon waking. She had addressed the stressful aspects of her life and no longer felt overwhelmed. The tightness in her spine was gone as was the stiffness in her mid-thorax.
Mrs B’s back pain was also gone; however, she mentioned she still did not feel “stable” or confident to load her lower back. She wasn’t convinced that it was back to normal, and the feelings of instability were still a part of her cognitive beliefs. She mentioned that she had a tightness in the back of her hip that she couldn’t stretch, and it seemed to become more noticeable when seated. It was a localised pain, that didn’t radiate down the leg.
Although she had mentioned sitting as a problem, I still chose the deadlift for the meaningful task assessment. This was carried out in a similar fashion to the first assessment i.e., unweighted.
Standing Start Screen Functional Unit 1 Findings
Pelvis: The pelvis was in left TPR and left IPT
Hips: The hips were now congruent with the left TPR
Thorax: TR8 was rotated to the left and translated right, TR7 rotated right and translated left
Unweighted Deadlift Functional Unit 1 Findings
Pelvis: During the task the pelvis remained in a left TPR with an unlocking of the left SIJ. This happened at the end of the range of the task i.e. 100%.
Hips: The left HOF moved further anterior relative to the pelvis and the right hip and did so before the SIJ unlocked i.e. at 90%.
Lumbar: L5 increased its rotation to the right with the unlocking of the left SIJ.
Thorax: TR7 & TR8 both increase their rotation and translation at the end of the range of the task i.e. at 100%.
Correcting the hip alone did not correct the pelvis or thorax. Correcting the hip and pelvis improved TR7 & TR8 and the task but Mrs B did not feel comfortable. I needed a co-correction of the left hip, pelvis for control (using the connect cue) and thorax at TR8 to correct the task. Correcting TR8 corrected TR7. This time I was able to get a full correction of TR8.
FU#1 Drivers: Co-drivers: Left hip, pelvis, thorax (TR8)
Further assessment of the left hip
Active Mobility
Same findings as first session.
Passive Mobility
A passive mobility test done in supine at the angle of the loss of control revealed a vector that extended from the sacrotuberous ligament to the posterior side of the obturator internus tendon as it wraps around the back of the ischium and attaches to the greater trochanter. Further assessment via palpation of the vector revealed it was the sciatic nerve. It had a restriction in its mobility within the tissue. There was no lateral glide of the sciatic nerve.
Stecco (2015), says that the obturator fascia continues with obturator internus covering the superior and inferior gemelli. This fascia attaches sacrotuberous ligament and attaches over the quadratus femoris, (Stecco, 2015). This fascia is meant to provide a sliding surface for the sciatic nerve, (Stecco 2015). In the prior treatment session, I had treated the obturator internus but not this part of the membrane.
My hypothesis was that the sciatic nerve was restricted in the fascial membrane mentioned previously, which had become stiff and was preventing the normal slide of the sciatic nerve. This was likely from the chronic overuse of obturator internus.
Active Control
As was noted in the screen task the left hip moved anteriorly at 90% of the task. After release of the sciatic nerve the hip no longer translated anteriorly in the task.
Further Assessment of the pelvis
Active Mobility
The left innominate rotated posteriorly relative to the left side of the sacrum with less amplitude than the right in the open chain test of a OLS. However, it still moved freely in the movement. This indicated it was unlikely to be an articular vector acting on the left SIJ.
Passive Control
This test was conducted with the joint in its close packed position. I tested this before testing passive mobility. I did this test to ensure Mrs B understood that her pelvis had no ligamentous compromise.
- Diane’s comment:
This assumes that there are no restrictive vectors and that you can get the SIJ in the close pack position, otherwise you will get false positives with this test. Usually, passive mobility tests and release techniques are required before the joint mobility is sufficient to test Passive Control.
- Stuart's response:
I always get these terms mixed up. I think I need to compartmentalise them as pre and post treatment assessments. Active/Passive mobility pre-treatment. Active/Passive control post treatment.
- Diane’s comment:
Active control is part of your ‘finding the driver’ part of the assessment (alignment, biomechanics and control) so I would disagree that active control or passive control is only after treatment. If the story is one of recent trauma, then passive control may be the first thing you do.
Passive Mobility
I brought the pelvis into a symmetric position by bolstering the left leg and the left innominate was anterior. I then did a glide of the joint into the first barrier of restriction focusing on either to the superior, middle, or inferior portions of the joint. A listening from gliding the superior, middle, and inferior portions of the left SIJ posteriorly in the plane of the joint gave a medial and cephalad vector that headed towards the loops of the small intestine and the root of the mesentery. This was done by loading the SIJ passively and then releasing and listening. The middle part gave the strongest vector. The root of the mesentery is a strong piece of fascial tissue that attaches to the back body wall and supports the small intestine, (Barral, 2020). Barral notes that c-section deliveries can cause vectors of pull/adhesion in the loops of the small intestine and root of the mesentery, (Barral, 2006, Barral 2020). The visceral vector acting on the pelvis could have been from the c-section birth 17 years previously.
I confirmed the this by using a Barral listening technique over the pelvis and lower abdomen to confirm the vector. These vectors feel like soft pieces of marshmallow trapped in the pelvis with a thick tight barrier drawing them towards the spine.
Active Control
The SIJ lost control at 100% of the task after release of the vectors. This was corrected with a 50% belly button to spine cue. This is described after the release below
Further Assessment of the thorax (TR8)
Active Mobility
Increase translation/rotation during the meaningful task. This occurred after the hip and pelvis gave way in the meaningful task.
Passive Mobility
The 8th thoracic ring could be fully corrected this time. On release of the ring there was a strong visceral vector drawing the ring into left rotation and right translation. The vector drew the rib in towards the liver with an inferior pull towards the pelvis.
Due to the involvement of a visceral vector, I used a Barral listening technique on the abdomen to determine what the visceral restriction was. It was the splenic flexure of the ascending colon where it attaches to the diaphragm behind the liver. This vector feels like a like a lump resting behind a large ham. The lump has an inferior pull on it.
Active Control
After release of the visceral vectors acting on the ring, the ring was stable in the task. It did not translate even with a loss of control at the pelvis.
Passive Control
Not necessary
2nd Session Treatment of the Drivers
Release
I released the sciatic nerve first using a Barral technique that takes the hip slowly into flexion while holding the sciatic nerve in the direction of restriction. This involves waiting for the inspiration phase or expansion phase of the nervous system to move the hip, stopping in exhalation or contraction. A passive correction of the hip yielded no further vectors.
I then released the root of mesentery using a Barral technique that involves gripping either side of the membrane, drawing it anteriorly and then taking it into directions of restriction or ease until a release is felt. A passive correction of the left SIJ still gave an intrapelvic vector that with some pelvic listening turned out to be some loops of the small intestine. They were released by grasping the restricted loops and gently taking them into directions of resistance and ease until they released. A passive correction of the SIJ yielded no further vectors.
I lastly treated the thorax restriction by treating the splenic flexure of the descending colon where it attaches to the diaphragm. This was done in sitting and involves lifting the splenic flexure of the colon with the patient in thoracic flexion. Then slowly having the patient extend, stopping when tension is felt in your fingers until the patient is fully neutral in sitting again. After the release I palpated the thorax and could no longer feel the translations at TR7 & TR8. An active mobility test demonstrated optimal biomechanics.
I re-assessed Mrs B in the meaningful task. She noted that her hip felt “lighter” now and she could breathe better; however, the left SIJ was still unlocking at the end of the range i.e., 100% of the task. The thorax and hip findings were corrected. When I manually corrected the SIJ Mrs B felt better. We tried the “20% pelvic floor” lift cue we had previously used but found this was no longer effective in the task.
I now needed to do an assessment of the motor control of the pelvis. I tested the recruitment ability of transversus abdominis in supine.
Motor Control Assessment and Active control of the pelvis
In supine when cued for the “20% pelvic floor lift” I found the middle and lower portion of the left side TrA was not co-contracting. We tried a belly button to spine cue and found she
overactivated internal oblique. I cued for “50% belly button to spine” and this corrected the IAO overuse. I then tested the cue in the task. This time we found she could control the left SIJ effectively in the task with this connect cue.
Connect
Mrs B’s connect cue was “50% belly button to spine” during the task practice.
Move
Mrs B was then sent home with homework to work on regaining control of the left SIJ while practicing the meaningful task. She could do 8 repetitions before she lost control of the left SIJ. Her goal was to reach 3 lots of 15 repetitions to improve the strength endurance of TrA in the task. We spent time ensuring she understood what it felt like when she wasn’t using an effective strategy. Her hip no longer translated, so she needed to understand what it felt like to have control versus losing control. This helped to allay the fears of her spine simply being “unstable”. She now felt like she had control of the issue.
Follow Up Sessions
The next treatment session yielded no suboptimal alignment, biomechanics or control or any body region during the meaningful task assessment in an unweighted deadlift. So, we added weight and noted she just felt weak. She could control the movement from a stability perspective. She just lacked confidence and had lost some conditioning. From this point, the treatment sessions focused on improving strength and control of the hip, lumbar spine, and abdominal wall in a progressive overload manner until she felt confident to load her spine. Now she was stable, she was keen to address anything that might be weak and would prevent her from making progress in the future.
In the next few sessions as squatting and general barbell/pull up bar loading were part of the movements she would encounter in CrossFit we also assessed these and found the foot ended up being a driver in a squat task. The hand grip on the left side needed to be strengthened too. These tasks were tested with weight after Mrs B had done some strength work in the gym again.
With this progressive overload program, and homework to fix the various weakness that developed from the years of compensating, Mrs B returned to CrossFit classes around 3 months after her initial injury. Since then, she has reported that she has felt none of her old issues and feels more confident to lift without fear of injury.
References
Barral J.P. (2020) Advanced Visceral Manipulation: Neuroendocrine approach to the abdomen, Barral Production, Florida, USA
Barral J.P. (2006) Urogenital Manipulation -revised edition, Eastland Press Inc. Seattle, USA
Barral J.P. (2007) Visceral manipulation – revised edition, Eastland Press Inc. Seattle, USA
Barral J.P. (2007) Visceral manipulation II – revised edition, Eastland Press Inc. Seattle, USA
Barral J.P., Crobier A. (2013) Manual therapy for the cranial nerves, Barral Productions, Palm Beach Gardens, Florida, USA
Barral J.P., Crobier A. (2012) Manual therapy for the peripheral nerves, Barral Productions, Palm Beach Gardens, Florida, USA
Barral J.P., Crobier A. (2019) New manual articular approach; Cervical Spine, Barral Productions, Palm Beach Gardens, Florida, USA
Barral J.P., Crobier A. (1999) Trauma: An osteopathic approach, Eastland Press Inc. Seattle, USA
Bogduk N. (2012) Clinical and radiological anatomy of the lumbar spine, 5th Edition, Elsevier Ltd. United Kingdom
Chaitow L. et al. (2014) Fascial dysfunction: Manual therapy approaches, Handspring Publishing Ltd. East Lothian, Scotland
DeStefano L. (2011) Greenmans principles of manual medicine”, 4th Edition, Lippincott Williams & Wilkins, Baltimore, USA
Feigl G., Hammer G., Litz R., Kachlik D., (2020) The intercarotid or Alar Fascia, and other cervical fascias, and their adjacent spaces – a plea for clarification of cervical fascia and spaces terminology, Journal of Anatomy, Vol 237, pp. 197-207
Fernandez-de-las-Penas C. Mesa-Jimenez J. (2018), Temporomandibular disorders: Manual therapy, exercsise, and needling, Handspring Publishing Ltd. East Lothian, Scotland
van Greinsven H., Strong J., Unruh A.M. (2014) Pain: A textbook for health professionals, 2nd Edition, Elsevier Ltd. United Kingdom
Hengeveld E., Banks K. (2014) Maitland’s vertebral manipulation: Management of neuromuscloskeletal disorders volume 1, 8th Edition, Elsevier Ltd. United Kingdom
Hodges P.W., Cholewicki J., Van Dieen J.H. (2013) Spinal control: The rehabilitation of back pain state of the art and science, Elsevier Ltd. United Kingdom
Kurz, T. (2016) Science of Sports Training: How to plan and control fof peak performance, 2nd Edition, Stadion Publishing, Island Poond, USA
Lee D. (2016) Diastasis rectus abdominis: A clinical guide for those who are split down the middle, Learn with Diane Lee, Surrey, Canada
Lee D. (2018) Thorax: An integrated approach, Handspring Publishing Ltd. East Lothian, Scotland
Lee D., Lee L.J. (2011) The pelvic girdle: An integration of clinical expertise and research, Elsevier Ltd. United Kingdom
Levangie P.K., Norkin C.C. (2011) Joint structure and function: A comprehensive analysis, 5th Edition, Davis Company, Philedelphia, USA
Lewis J. (2016) A.T. Still: From dry bone to living man, Dry Bone Press, Gywnedd, UK
Liem T. (2004) Cranial Osteopathy: Principles and Practice, 2nd Edition, Elsevier Ltd. United Kingdom
Marlien E. (2021) The new approach to the vagus nerve and autonomic system, Barral Productions, Palm Beach Gardens, Florida, USA
McPartland J., Skinner E. (2004) Cranial osteopathy: Principles and practise, Elseiver Ltd. United Kingdom
Paoletti S. (2006) Fasciae: Anatomy, Dysfunction and treatment, Eastland Press, Seattle, USA.
Pool-Goudzward A.L, Kleinrensink G.J., SnidjersC.J., Entius J., Stoeckart A. (2001), The sacroiliac part of the ligament, Journal of Anatomy, Vol. 199 pp. 457-463
Porges S. (2011) Polyvagal Theory: Neurophysiological foundations of ermtions, attachment, communication, self regulation, Norton and Company Inc. New York, USA
Richardson C., Hodges P., Hides J. (2004) Therapeutic exercise for lumbopelvic stabilisation: A motor control approach for the treatment and prevention of lower back pain , Elseiver Ltd. United Kingdom
Schleip R. et al. (2012) Fascia: The tensional network of the human body, Elseiver Ltd. United Kingdom
Stecco C. (2015) Functional Atlas of the human fascial system, Elseiver Ltd. United Kingdom
Stylian G. (2022) Dig-on Osteopathy: Module 1 – pediatric masterclass, In person lecture series, Narrabeen, Sydney
Sergueef N. (2007) Cranial Osteopathy for infants and adolsecents: A practical handbook, Elsevier Ltd. United Kingdom
Shuenke M., Schulte E., Schumacher U., (2010) Thieme Atlas of Anatomy: Neck and Internal Organs, Georg Thieme Verlag, Stuttgart, Germany
Sims J.A., Moorman S.J. (1996) The role of the iliolumbar ligament in low back pain, Medical Hypothesis Vol. 46 pp. 511-515
Sutherland, W.G. edited by Wales A.W. (1990) Teachings in the science of osteopathy, Rudra Press, USA
Upledger J.E. (1987) Craniosacral therapy II: Beyond the dura, Eastland Press, Inc. Seattle, USA
Upledger J.E., Vredevoogd J.D. (1983) Craniosacral therapy, Eastland Press, Inc. Seattle, USA
Viehofer F.A., Shinohara Y, Sprecher C.M., Bronek M. Boszczyk, MDc , Buettner A., Benjamin M., Milz S., (2015) The molecular composition of the extracellular matrix of the human iliolumbar ligament, The Spine Journal, Vol. 15, pp 1325-1331
Wheeless C. (2023) Wheeless Textbook of Orthopaedics
Skills Demonstration
Case Study Author
Clinical Mentorship in the Integrated Systems Model
Join Diane, and her team of highly skilled assistants, on this mentorship journey and immerse yourself in a series of education opportunities that will improve your clinical efficacy for treating the whole person using the updated Integrated Systems Model.
We will come together for 3 sessions of 4 (4.5) days over a period of 6-8 months with lots of practical/clinical time to focus on acquiring the skills and clinical reasoning to put the ISM model into practice. Hours of online lecture and reading material and 12 hours of in-person lecture are...
More Info