Story
- Mrs. O complained of a problem of urinary incontinence since 2nd delivery (2.5 years ago) when initiating the movements with vertical loading like sitting up from chair, walking and turning the direction on standing. She has never seen doctor about this issue.
- She has unstable feeling like ‘wobbling’ in both hip joints when weight bearing on her legs, especially starting the movements like starting walking, turning her body direction and trotting. This feeling started only on right side about 4 months ago and now feel on both sides. The feeling on right is much bigger than on left.
- She has the developmental dysplasia of the hip on both side.
- Her doctor didn’t find other thing like arthritis on MR imaging in her both hip joints.
- Lately she often has the urinary leakage and the feeling ‘wobbling’ in her hip joints at same time.
- When tightening up her pelvic floor muscles and hip muscles, she realized that she can prevent those symptoms.
- She has a wish to do something good for her body like physical exercises, however she actually can not exercise or work out because she always feels tired.
- She has 2 kids (1st labor- 5 years ago). She got them by vaginal birth and had episiotomy only when giving birth her 1st baby.
Meaningful Complaint
Urinary leakage and the wobbling in both hip joints especially in right side when starting the movement like standing up, walking, turning the body direction, unless activating muscles of pelvic floor and hip muscles intentionally.
Cognitive and/or Emotional barriers to consider
Mrs. O believes that she needs to contract her muscles strongly on pelvic floor and on hip joints to prevent leakage and hip wobbling when moving. She also believes that her joints are too ‘loose’, because people often indicated when taking the courses for physiotherapists that she had hypermobile joints. She thinks that her symptom on her hip joints is caused by that issue, and that belief seems to make her think about necessity to strengthen those muscles.
Diane’s question
What experience does she have (told in her story) that supports her cognitive belief that her pelvic floor and hip muscles are weak and what tests could you do to confirm or negate this belief?
Miwako’s answer
She has had many experiences that the symptoms were less when contracting the pelvic floor and hip muscles. From those experiences, she believes that she doesn’t have enough strength of the muscles. And, although she has the developmental dysplasia of the hips and she realizes the strengthening of the hip muscles are needed, she doesn’t usually do any exercises for the hips.
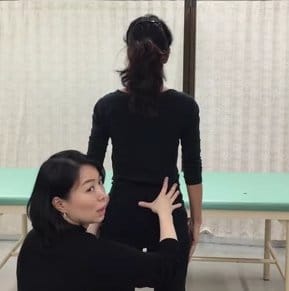
I assessed the screening tasks in detail based on her meaningful task. In order to confirm the movement strategies optimally or non-optimally, I found the failed load transfer sites during the tasks, corrected them and found out the two drivers for her at last. And I led her to realize that she could perform those tasks without those symptoms and firm contraction of the hip muscles during the meaningful tasks.
Diane’s further question
Much later in this case report under Other Tests you tested the strength (Grade 0-5) of the psoas muscle. Did this also help to address her cognitive beliefs or were they addressed mainly during performance of her screening tasks. Did she continue to believe her hips and pelvic floor were weak after your assessment?
Miwako’s response
Yes, I wanted to make sure her belief was confirmed or negated. Sometimes I see patients with developmental dysplasia and they have weakness of hip muscles. The weakness is sometimes truly weakness and sometimes just appearance (when you teach how to use they can output enough power like the case left hip). I think the true weakness resulted from their movement strategies, and the combined training of changing the strategies and the muscle strengthening is effective for them to keep the hip healthy.
Meaningful tasks to improve function and performance goals
Initiating of walking, turning the body direction on standing, standing up from sitting and trotting without leakage and hip wobbling.
Screening Tasks Pertaining to the Meaningful Task
These were chosen as screening tasks, because it realized that the issues happened when she changed the posture and shifted the weight with loading.
Standing Posture Findings
- Very compressive posture with forward head, long thoracic kyphosis and posterior tilted pelvis
- Obviously apical breathing
- Head: Left Intracranial Torsion
Diane’s question
What position are the left and right temporal bones in relative to each other in a left intracranial torsion? Did you assess the position of the sphenoid and if so was its position congruent or incongruent to the temporal bones?
Miwako’s answer
Left temporal bone is rotated posteriorly and right temporal bone is rotated anteriorly in relative to each other. Her eyes looked deeper on left side, so I concluded the position of the sphenoid was congruent to the temporal bones positions.
- Cervical spine: C5 translated to right/ rotated to left, C6 translated to left/ rotated to right
- Thorax: the 2nd thoracic ring translated to right/ rotated to left and 3rd thoracic ring translated left / rotated to right, the 5th thoracic ring translated left/ rotated to right
Diane’s question
List the cervical segments and thoracic rings that are in a position that is congruent with the cranium and those that are incongruent.
Miwako’s answer
C5 and the 2nd thoracic ring were congruent with ICT, and C6, the 3rd and 5th thoracic ring were incongruent with ICT.
- Pelvis: Left Transverse Plane Rotation (TPR). This was congruent with ICT.
- Hips: Both femoral heads translated anteriorly (bigger right side than left). This was congruent with pelvis IPT.
Standing posture response to corrections of sites of failed load transfer:
- Correction of C5 completely corrected the positions of C6 and the 2nd and 3rd thoracic rings. It also improved the position of the 5th thoracic ring. Then adding a correction of the right femoral head (right hip) totally corrected the left TPR of pelvis, the position of left hip, and the the 5th thoracic ring. She felt she had bigger and easier breathing with just the C5 correction.
Hypothesis of the drivers for this task
From my findings, it was suggested that C5 and right hip were co-driver. C5 correction resulted in realigned C6, the 2nd and 3rd thoracic ring position. Correction of right hip was needed to get the corrected positions of the 5th thoracic ring and pelvis.
Sitting Posture Findings
The positional findings in sitting were identical to those noted in standing with exception of the left hip.
- The femoral head on right was translated anteriorly and the one on left was positioned center (corrected from the standing posture).
Correction of C5 completely corrected the positions of C6, the 2nd, 3rd thoracic rings and improved the position of the 5th thoracic ring. Then adding correction of right femoral head corrected the 5th thoracic ring on sitting. She felt she had bigger and easier breathing with C5 correction similar to her experience in standing.
Hypothesis of the drivers for this task
From my findings, it was suggested that C5 and right hip were co-drivers. C5 correction resulted in realigned C6, the 2nd and 3rd thoracic ring position. Correction of right hip was needed for the 5th thoracic ring to be corrected.
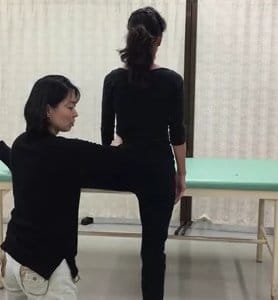
Standing up from sitting
- Neck extended, thoracic & lumbar kyphosis increased, pelvis further posterior tilted and lower abdomen bulged before lifting the buttocks up from chair.
Diane’s question
What does the lower abdomen bulging suggest with respect to the motor control strategy she used for this task and why?
Miwako’s answer
Her movement strategy during the task ‘sit to stand’ was the one flexed the spine predominantly in early phase. Usually in the early phase of this task optimally, it is needed to flex hip joints while holding the body extended against the gravity. She had poor control of the muscles to keep the trunk extended, and it suggested that strategy caused the intra-abdominal pressure which go down and front.
Diane’s further question
Of all the abdominals, which one is mostly responsible for controlling ‘bulging’ of the abdomen when pressure increases? This is a great clinical thing to look for because when we witness bulging in any part of the abdomen it suggests that this muscle did not activate appropriately.
Miwako’s response
I think that Transversus Abdominis is the most responsible muscle to keep the abdominal wall drawn in. With right hip and C5 correction the bulging disappeared, and it didn’t appear after the vector releasing. So I didn’t test TrA function. When I checked whether she had DRA or not, and I did not find it on her and she was able to contract well (slide it to each side equally).
Diane’s comment
If correcting drivers improves the performance of the abdominal wall and all visible bulging/doming goes away, and if pelvic and lumbar control is restored, there is not need to do a detailed examination of the abdominal muscles. If the SIJ had continued to lose control and/or if bulging of the abdomen in any of the quadrants persisted, then an abdominal wall assessment would be warranted.
- C5 further translated to right/rotated to the left, C6 further translated to left/rotated to the right
- The 2nd thoracic ring rotated to left/translated to the right and 3rd thoracic rings further translated to left/rotated to the right, and the 5th thoracic ring further translated to left/rotated to the right
- Loss of control of Sacroiliac Joint (SIJ) on both sides
Diane’s question
When she sat in the chair did you test her SIJ control? You note in her sitting posture that her pelvis was in a left TPR. Was this associated with an IPT (intra-pelvic torsion) or did one or both SIJ’s lose control as she sat?
Miwako’s answer
No, I didn’t test her SIJ control in sitting and during sitting down. She has left IPT in sitting, and both SIJ of her lost control as soon as lift the buttocks up from the chair.
Diane’s question
The finding of her SIJs losing control when she went from sit to stand suggests that her pelvis was in a left TPR and associated with an IPT (in sitting) and had not lost control during her stand to sit. Why? What did her pelvis do with respect to the TPR when she stood from sitting?
Miwako’s answer
I chose the task from sit to stand as a screening tasks, because one of the meaningful task for her was to initiate the movement from sitting (Diane – perfect clinical reasoning for developing a meaningful assessment that is relevant to the patient’s goals). It was suggested from the interview that the tasks which are needed to exert the strength would be assessed, so this task was given from relaxed sitting position. The task ‘sit to stand’ is required more motor control when starting the movement compared to the task ‘stand to sit’, because ‘sit to stand’ is the task to change the direction of the movement with resisting the gravity. This might have been caused the FLT in right hip and both SIJ from sit to stand. The task ‘stand to sit’ is required a different movement strategy and if that task or ‘squat’ would be tested, it may be found other findings. (Diane – I hadn’t thought about the loads being different and perhaps higher going from sit to stand as opposed to stand to sit – great hypothesis for why her pelvis ‘gave way’ moving from sit to stand and not from stand to sit).
- Femoral head on both sides translated anteriorly
Correction of the right hip resulted in full of control of both SIJs and better alignment of the left hip. Also, when the right hip was corrected the 5th thoracic ring translated less; however, there was no change in the alignment of C5, C6 and the 2nd and 3rd thoracic rings. Adding a correction of C5 resulted in improved alignment and control of the 2nd, 3rd, 5th thoracic rings and C6. C5 correction made the posture extended (not collapsed).
Hypothesis of the drivers for this task: Primary driver – right hip, Secondary driver C5
Diane’s question
In the prior 2 tasks (standing posture, sitting posture) you had to correct both C5 and the right hip and you hypothesized that they were co-drivers. In the sit to stand task, you had to correct both C5 and the right hip yet you hypothesize the hip is primary and C5 is secondary. Can you provide a definition of the difference between a co-driver and a primary/secondary driver especially when the same sites of the body are found responsible?
Miwako's answer
As you mentioned this, I think I had to call this ‘ co-driver’. My understanding is this; the co-driver is that each driver is responsible equally. When there are two drivers and they’re called the primary / secondary, that means primary is responsible for more than 50% and secondary less than 50% and you can get bigger impact when you correct the Primary driver.
I wrote the driver for the task ‘weight shift to right’ is Driver1 & 2 which means (for me) they’re co-driver. To be honest, I don’t know why I wrote primary/secondary.Diane’s response
Yes, that is the accurate definition of the difference between a co-driver and a primary/secondary driver. Mrs. O appears to have a co-driver for all tasks evaluation so far.
Standing weight shift to right
From the findings noted in standing posture above, the following occurred when she shifted her weight to the right
- C5 further translated to right/rotated to left, C6 further translated to left/rotated to right
- The 2nd thoracic ring translated to right/ rotated to left and 3rd thoracic rings further translated to left/rotated to right, and the 5th thoracic ring further translated to left/rotated to right
- Loss of control of right Sacroiliac Joint (SIJ)
Diane’s question
What motion did you feel between the right innominate and the right side of the sacrum that led to your conclusion that the right SIJ had lost control during this task?
Miwako’s answer
I felt the right innominate rotated anteriorly relative to the right side of the sacrum.
- Right femoral head further translated anteriorly and right femur internally rotated
- Right foot pronated (the calcaneus everted and the talus plantar flexed and rotated internally) and this was a congruent with the motion of the right femur.
- Correction of right hip resulted in full of control of the right SIJ, right hip and right foot position, and she experienced the feeling in right hip disappeared and the translation of 5th thoracic ring was less. Adding a correction of C5 resulted in full of control on C6, the 2nd, 3rd and 5th thoracic rings.
- With butt gripping (which was usual way for her to reduce the feeling “wobble”), the right femoral head translated anteriorly on standing and stayed there on weight shifting to right.
- DRIVERS: Driver1-right hip, Driver2- C5
Diane’s question
You list the drivers as 1 & 2. Were they co-drivers or was one primary and the other secondary?
Miwako’s answer
C5 and the 2nd thoracic ring were co-drivers.
Standing weight shift to left
- C5 further translated to right/rotated to left, C6 further translated to left/rotated to right (both translations/rotations were less than when shifting to right)
- The 2nd thoracic ring translated to right/rotated to left and 3rd thoracic ring further translated to left/rotated to right, and thoracic 5th ring further translated to left/rotated to right
- Pelvis further rotated to left in the transverse plane
- Loss of control of left SIJ
- Left femoral head further translated anteriorly
- Correction of right hip on static standing posture resulted in full of control of left SIJ and pelvic position and resulted in less translation of 5th thoracic ring during the task. Then adding correction of C5 during this task, it was resulted in full of control on C6, the 2nd, 3rd and 5th thoracic rings.
- DRIVERS: Driver1- C5
Diane’s question
For the left weight shift task a primary driver of C5 is listed. However, prior to the C5 correction a correction of the right hip was done. Why do you hypothesize, therefore, that only C5 is the driver?
Miwako’s answer
Sometimes I’m confused with the meaning of ‘the Driver’. In this case, I corrected right hip on standing, but I didn’t hold it during the task. Is this called ‘the driver’ for this task, too? I thought that what is called ‘the driver’ for a movement task is the one you need to keep the correction or encourage the optimal biomechanics during the task. I didn’t realize I haven’t been able to clarify about this. Thank you Diane.
Diane’s response
One of the purposes of doing the ISM certification is just this. To help all of us clarify language and definition confusion and solidify the principles of this approach. Whether you have to maintain a manual correction of a body region to identify that region as a ‘driver’ is irrelevant (I think). We don’t have to hold the foot position to see the impact of this correction on for example the cranium. We ask the patient to maintain the correction after we put it there. Whether they can, or not, is another matter. So, if Mrs. O was able to maintain the improved position of her right hip after you released your manual correction as she shifted her weight to the left, then I would consider this right hip as a component, or driver, for this task. If her hip translated back to its anterior position and was there when she shifted her weight, then it wouldn’t be a driver because it wasn’t in a corrected position during the task. I hope that makes sense!
Vector Analysis of the Drivers and Underlying System Impairments
The following system vectors were noted on vector analysis of the relevant drivers:
It was found two drivers (C5 and right hip) and they were co-driver.
- C5
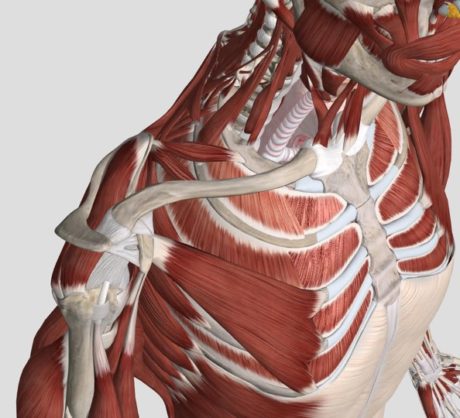
Neural 1- Over-activation of a fascicle of the scalenus posterior attaching to C5 on right. (This fascicle attaches to 2nd rib and rotates 2nd rib anteriorly on right, and thus creates left TPR of the 2nd thoracic ring)
Diane’s question
I agree that this is a common finding when there is over-activation of a fascicle of scalenus posterior. Why does the fascicle anteriorly rotate the 2nd rib and not posteriorly rotate it?
Miwako’s answer
I think this is because of the attachment site on 2nd rib. My understanding about the anatomy of scalenus posterior is that the attachment site on the 2nd rib is the superior, lateral and just a little posterior portion and the dorsal side, it creates a vector to rotate the 2nd rib anteriorly and/or translate C5-7 laterally.
Diane’s response
You are absolutely right! Check out this amazing picture of the anatomy of this complex region. Note how the fibres of serratus posterior attach to the posterior aspect of the 2nd rib and therefore upon activation will pull the posterior part superiorly and thus anteriorly rotate the rib. Another muscle to note is the first fascicle of serratus anterior attaching to the 1st rib. It is a strong first ring rotator and/or scapular ‘tipper’.
Miwako’s answer
Thanks for the great picture Diane!
I think the fascicle of the serratus anterior on 2nd rib is scapular tipper too! This fascicle is also a big tipper of the 2nd thoracic ring, isn’t it? The muscle is very interesting!
Neural 2- Low activation of Diaphragm (Correction of C5 created bigger abdominal and costal movement on breathing)
Diane’s question
While we may not always understand the underlying mechanism for findings can you explain how correcting C5 could create ‘bigger abdominal and costal movement on breathing)?
Miwako’s answer
Not sure, but I hypothesized that the phrenic nerve from C3-5 impacted the activation of the Diaphragm. When the Diaphragm works better during breathing, you can see the movement in the lower part of the trunk, not in the upper part. C5 translation may cause the inhibition of the phrenic nerve and it could make the Diaphragm dysfunction. Sometimes you find TrA activity gets better with lower thoracic ring correction. As one of the reason for this, it may be suggested that the lower thoracic nerves work better when a ring is corrected and the tissues around the ring is repositioned. I thought same theory with this. I guess this is one of the possibilities, I don’t know how I can investigate this though.
Diane's response
I don’t either but it’s interesting to postulate on these things.
- Right hip co-driver with C5.
- Neural 3- Over-activation of the Obturator internus (which creates a vector to push femoral head anteriorly)
- Neural 4- Low activation of right Psoas major (which causes the right femoral head is harder to maintain the center in acetabulum)
- Articular- Shallow acetabulum on hip (which creates condition to move anteriorly easier)
Other Tests
Manual Muscle Testing (MMT) for Psoas
- On right hip: 3 (fair), and 4 (good) with connect cue for psoas
- On left hip: 4 (good), and 5 (strong) with connect cue of psoas
- Very hard to keep the condition with connect cue for psoas
Active Straight Leg Raising Test (ASLR)
- Right leg was much easier to raise with lower thoracic general compression
- C5 correction made also much easier to raise right leg, and the best hands-on was to do both C5 correction and lower thoracic compression together.
Diane’s question
The lower thorax did not show up in any other task as being influential (a driver). Can you hypothesize how compressing the lower thorax can impact the right hip (which has been noted to be relevant to other vertical loading tasks)?
Miwako’s answer
This is the meaningful task aside. As I answered in the above question, I hypothesized that the phrenic nerve had been impacted by C5 translation and the Diaphragm had been dysfunctional, and I thought it might cause the apical breathing and also the deficiency of oxygen and it made her feel tired. I wanted to confirm this to explain to her in the way was be focused on the diaphragm and also in the way she could feel easily. The diaphragm attaches from the 7th-12th rib to the ventral side of lumbar spines, and in my opinion the compression (like you create a vector to make a group gently) on the lower thorax can mimic a vector of the diaphragm. With C5 correction and the compression on the lower thorax got the improvement on this task. I thought that it suggested she needed a vector more in lower thorax. To clarify something has been caused, sometimes I do tests putting the meaningful task aside.
Diane’s response
Perfect reason to do this. Also, the diaphragm connects to the hip through psoas therefore by increasing general compression of the lower thorax you may be influencing both a fascial and neural component of the psoas and thus the hip.
Hypothesis
Mrs. O has symptoms of urinary leakage and wobbling hip joints when initiating some vertical loading movements like standing up from sitting, walking and changing the direction of her body during standing. When she does those movements with contracting muscles of pelvic floor and around hip joints, she doesn’t feel wobbling on her hip joints and often doesn’t have the leakage. Based on my clinical findings, my hypothesis is that the imbalance of muscle activities on vertical loading tasks was underlying.
From the findings with corrections, there was a co-driver for her screening tasks, the right hip and C5. Correction of the right hip on static postures resulted in full of control of left hip and the SIJs during screening tasks. The positions of the 5th thoracic rings were better, but still translated. C5, the 2nd and 3rd thoracic rings didn’t change at this time. Adding correction of C5 during the screening tasks resulted in full of control of the thoracic rings as well. This suggests that right hip and C5 was co-driver.
Diane’s comment & question
To determine a true co-driver, you would have the same result if you reversed the order of correction i.e. correct C5 first and then the hip. I’ll let you add how this differs from a primary/secondary driver situation in the question I asked above. My question here is: Why does it matter? How does knowing you have a co-driver vs a primary/secondary driver influence your treatment planning:
Miwako’s answer
When you find a co-driver, you need to treat them and remove those non-optimal condition simultaneously in order to get the best result. If you find two drivers and they’re primary/secondary, you need to plan the treatment for the primary driver first and then for the secondary. When you treat the primary driver, you can get better result but it’s not enough. When you work on the secondary driver, you can get the best result. The treatment for primary driver is priority.
Loading tasks during work increased after she changed her position 2 months ago, and this may have resulted in a non-optimal change in her movement and muscle recruitment strategies. On the right hip, obturator internus, which has a vector to push femoral head anteriorly, had the augmented activity while psoas, which works with obturator internus to keep femoral head centered, had compromised activity. Furthermore, she has the developmental dysplasia of the hip on both sides and has disadvantageous hips structurally (articular system impairment). Collectively, these can create loss of control of right hip.
On clinical observation, it was found that her usual breathing pattern was apical and it appeared that the activation of her neck and upper thoracic muscles were increased. The primary vector of the C5 driver was the left scalenus posterior. Correction of C5 also restored her collapsed posture and facilitated the activation of the postural muscles of the trunk (TrA and the back deep extensors). C5 translation can affect the phrenic nerve and has the potential to impact function of the diaphragm.
It is suggested that the Diaphragm is needed to create vector more from the result of ASLR test, and this may be the Diaphragm has sustained to be dysfunctional for a long time.
Miwako
Not sure I understand what you mean in this sentence?
As I mentioned in the question and the answer above, in my opinion the meaning of ASLR-test with the compression on the lower thorax creates a similar vector with the Diaphragm. C5 correction improved the breathing pattern and impacted ASLR-T, and the compression on the lower thorax got better result. From these findings I concluded the diaphragm might be dysfunctional. I thought that dysfunction could cause the deficiency of the oxygen and this might relate to her feeling ‘always felt tired’. However, there are nothing demonstrates these thought.Diane
I understand now, thanks.
Treatment Plan
R: Driver 1- Right hip: right obturator internus; Driver 2- C5: right scalenus posterior
A: Align right hip – best cue was to ‘relax your butt, widen sitz bone, and then put your femoral head in the socket.’ C5- ‘relax your shoulder, open your chest and float your head’.
C: The correction of C5 and the right hip resulted in full control of all sites of failed load transfer as well as improved recruitment of the diaphragm, TrA and other muscles to keep good posture. So after releasing and aligning C5 and right hip, we moved to ‘move’ piece.
Connect cue for Psoas got better result, and it was given connect cue when training for Psoas ‘Connect a guy-wire from thigh inside, coming up and to the back of belly button’.
M: Incorporate align cues on standing, squat and then weight shift. Progress with theraband or stepping in order to increase load.
Incorporate align cues, and deep and slow abdominal breathing.
She needs to continue the loading activities for work and have no feeling of wobbling on her hips (without butt gripping) and also no feeling about to have the leakage with optimal alignment and biomechanics on right hip and C5. It will be needed to keep the training if optimal strategies are to become automatic. It was found that the improvement of function about the Psoas and other postural muscles with corrections of right hip and C5, but the strength and the endurance of postural muscles would be needed more for her work. With increasing of physical activities on daily, progression can be considered.
Follow up treatment sessions
September 28
After first visit, she didn’t have any experience of urinary leakage at all and realized that she had a habit to go to the bathroom lots of times a day. Regarding the symptom of the wobbling in hip, the feeling in left hip was disappeared and the one in right hip has been gradually reduced. She has kept training as much as she can since first visit, but also she has felt the difficulty going on a ‘special’ exercise at home daily because she can’t have enough time.
Meaningful Complaint
The wobbling in right hip is still felt when starting only walking without connect cue consciously.
Screening Tasks Pertaining to the Meaningful Task
1. Standing Posture
- Better. Can keep tall position on standing.
- Looks still compressive posture with long thoracic kyphosis unconsciously
- Breathing pattern: Not see apical breathing
- The 5th thoracic ring translated to left/rotated to the right
- The femoral head on right is translated anteriorly
- Correction of the 5th thoracic ring resulted in realigned femoral head on right.
- When Creating tall posture on standing consciously, the correction of the 5th thoracic ring is harder and the femoral head is further translated anteriorly.
- Compared to first visit, ICT was disappeared and C5, C6, the thoracic ring 2nd & 3rd and femoral head on left are realigned.
2. Weight shift to right
- The 5th thoracic ring further translated to left/rotated right
- Right femoral head further translated anteriorly and right femur internally rotated
- Right foot pronated
DRIVERS: Mrs. O is now presenting with a primary driver of the 5th thoracic ring
- Correction of the 5th thoracic ring resulted in full of control of right hip, realigned hip and foot on right and no feeling of the wobbling in right hip.
Vector Analysis of the Drivers and Underlying System Impairments
The following system vectors were noted on vector analysis:
- 5th thoracic ring (primary driver)
- Neural –
- Over activation of External oblique attached to 5th rib on left
- Over activation of Obturator Internus on right
Myofascial – Shortening of the fascial line from right hip to T5th ring (it suggested that the fascia continuity of adductor, pelvic floor, psoas, diaphragm and pleura)
Other Tests
Manual Muscle Testing (MMT) for Psoas
- On right hip: 4 without connect cue (CU), 5(strong) with CU for psoas, and after the treatment 5 without CU
- On left hip: 5 (strong) without any cue
- Very hard to keep the condition with connect cue for psoas
Active Straight Leg Raising Test (ALSR-T)
- Right leg was a little easier raise with lower thoracic compression.
- T5th correction doesn’t make a big difference
Hypothesis
Mrs. O still has the feeling ‘wobbling’ in right hip joint when only initiating walking. She had had same feeling in left hip at first visit, and it’s gone now. Also she had had the urinary leakage last time, and she has been able to move without the leakage since first treatment. Based on my clinical findings at the 2nd visit, my hypothesis is that the symptom was resulted from still existed the translation of the 5th thoracic ring. On standing, the 5th thoracic ring was still translated to left and the femoral head on right was translated anteriorly. Other non-appropriate sites, which were found at 1st visit, were not seen. During weight shifting to right, the 5th thoracic ring further translated/rotated and also the femoral head on right was further translated anteriorly. Correction of the 5th thoracic ring resulted in full of control of right hip during weight shifting, and the feeling in right hip was gone. This suggests that the 5th thoracic ring was the primary driver at 2nd visit.
From the result of vector analysis, it was found that the 5th thoracic ring has two vectors. The first vector is the fascicle of the external oblique attach to 5th rib on left. And the second one is the fascial line and it was expected the part of the deep front line on right side by T Myers, which is from the adductor longus to the pleura through pelvic floor, psoas and diaphragm. The translation of femoral head was found on standing and it was more obvious on tall standing. This suggests that there is a shortened fascial line and it makes a vector between the 5th thoracic ring to hip. The habitual trunk posture of her is slumped position, so this may create the shortened vector inside. After the releasing this vector, psoas on right side was stronger and wasn’t needed the connect cue. It shows that it will be needed to keep the length of the fascial line in order to keep the muscle strength of Psoas on right side. From the result of ASLR-T, the thoracic 5th ring correction didn’t bring any differences and lower thoracic compression made a better change. It suggests that Diaphragm will be needed to keep up strength training in order to maintain a comfortable tall posture.
From the saying at the 2nd visit, it seems that she feels the burden for the home exercise in cognitive dimension, and it suggests that she needs to learn easier way for training. The abdominal breath training with ring correction will be easy way to disconnect between hip and the 5th thoracic ring and restore the length. This will be also the training for the Diaphragm.
Treatment Plan
R: Driver 5th thoracic ring –
- The fascicle of external oblique attach to 5th rib on left
- The fascial line from adductor to pericardium
A: Align the 5th thoracic ring – Best cue was to ‘relax your belly and hang your chest from the ceiling’.
C: Given the align cue and with correction 5th thoracic ring resulted in full control of right hip. So after releasing and aligning the 5th thoracic ring moved to ‘move’ piece.
M: Incorporate align cues on standing and weight shift to right. And progress with theraband in order to increase load. The way is to put the band under the feet, take hold on each side of it with both hands and create the vector to load on trunk. Under loading, shift the weight to right and stand on right leg. The abdominal breathing with self-correction of the 5th thoracic ring on taller posture with extended right hip
Diane’s comment to end the case report: This is an excellent example of how dynamic the body is and that we must be aware that drivers will (and should change) between sessions. We are always required to assess every task and expect there to be changes if we are moving forward towards better strategies for function and performance. Well done, Miwako!
Diane’s comment to end the case report
This is an excellent example of how dynamic the body is and that we must be aware that drivers will (and should change) between sessions. We are always required to assess every task and expect there to be changes if we are moving forward towards better strategies for function and performance. Well done, Miwako!
Skills Demonstration
Case Study Author
Clinical Mentorship in the Integrated Systems Model
Join Diane, and her team of highly skilled assistants, on this mentorship journey and immerse yourself in a series of education opportunities that will improve your clinical efficacy for treating the whole person using the updated Integrated Systems Model.
We will come together for 3 sessions of 4 (4.5) days over a period of 6-8 months with lots of practical/clinical time to focus on acquiring the skills and clinical reasoning to put the ISM model into practice. Hours of online lecture and reading material and 12 hours of in-person lecture are...
More Info