Story
Laura is a physical therapist who is extremely active with both long distance running and rock climbing. Laura reports that she decided to come in for therapy after running a 50 k last week and having a flare up of her chronic left upper thoracic pain. She reports that around 10-12 miles into her race she had an intensification of her usual left sided upper thoracic pain and stiffness to more of a burning pain. She points to the left of the T3/4 spinous process when asked where she feels pain. She reports that besides running she feels pain and stiffness in this area when rotating her trunk to the left.
Laura reports that her relevant history includes a fall off of a rope swing onto her front side when she was a kid which knocked the wind out of her. She reports that after that time she developed some asthma like symptoms which for a time required an inhaler for breathing during exertion. She reports that growing up she always had an awareness of a tightness in her upper thoracic area but it wasn’t until 3 years ago while riding a century ride on a bike that she reports was not properly fitted that she had an intensification of the left upper thoracic pain. Last summer she reports that while doing a lot of sitting and typing for her certification in manual therapy and running an ultramarathon in June 2018 her symptoms became more intense again. She reports that since that time she has continued to run but has had to modify her training and even her running form. She reports that if she starts to experience pain she can stiffen her thoracic spine and decrease her arm swing which helps her get through the rest of the run. She reports that currently she has an awareness of tension in the upper thoracic spine and down the left upper extremity.
Diane’s question:
This story has a very ‘mechanical’ sound to the pain behavior. What key features from the story so far suggests that there may be an element of peripheral and/or central sensitization happening in her nervous system?
Matthew’s response:
The patient has been suffering from some level of symptoms since her childhood. Although they have intensified as of late it has been 3 years since the bike ride that she reports intensified her symptoms. Pain of a duration as long as this has been shown to have a central component. It is also very clear that endurance running is a significant part of who she identifies as. If her symptoms are threatening her ability to continue to have this lifestyle she will likely feed into the central sensitization that is part of her picture. I would also point out that what she remembers as being the original onset of symptoms when she was a child falling off of a rope swing, was a very active moment in her life. Central sensitization will likely be heightened when the patient is engaged in athletic type movements and events such as this as it was the type of event that lead to her injury as she remembers it. Those neural pathways that are triggered by the adrenaline rush of pushing her body and being outside will certainly light up when she is running on the trail pushing herself through a long run.
Past Medical History
Laura reports that her past medial history is significant for an umbilical hernia repair at 5 years old, tonsillectomy and wisdom teeth extraction in high school, irritable bowel syndrome which seems to be exercise induced, occasional anxiety and a left tibial stress fracture in 2011. She also reports that she has been experiencing chronic left sided lower back discomfort which becomes worse with prolonged sitting and can occur with sudden movements like when needing to guard one of her patients.
Diane’s question:
Exercise induced irritable bowel syndrome – the bowel is usually irritated by the ingestion of foods that the individual is sensitive to. Do you have any hypotheses as to how exercise can cause bowel pain?
Matthew’s response:
In conversations with this patient after her initial treatment sessions she reported that she did go through some testing to try to better identify if there were any food sensitivities that were contributing to her IBS. She reported that she came back positive for some of the most common food sensitivities including gluten, dairy and soy. She is working on going through an elimination diet as she would really like to heal her gut and prevent any further damage to the lining which is what she believes might be going on. Because of the connection of the autonomic nervous system to the gut I think that it is very important to consider the impact it may be having on the function of the digestive system. When doing intense exercise the sympathetic nervous system may be going into an “overdrive” situation in which vagal tone is increased. This could have similarities like when the body feels threatened which would slow her digestion further. I think that it will be interesting as we learn more about “leaky gut” and the impact of the tight junctions whether there is a further gapping of these junctions to allow food to move through the lining of the gut when in a sympathetic state. This could further lead to the autoimmune response of someone with a leaky gut. It has become evident recently by the work of Rosenberg that when we are competing in an athletic event there should be a balance between the ventral vagal and spinal sympathetic response which may be off balance with this patient leaning toward a more powerful spinal sympathetic response.
Diane’s comment:
And since the sympathetic nervous system has its origins in the thorax, and the thorax is a primary region for trunk rotation in a runner, it is biologically plausible that there is a somato-visceral component to this story.
Meaningful Complaint
Patient reports that her most meaningful complaint is discomfort which is described as tension in the left upper back which can become more painful and burning at its worst with long distance running and left thoracic rotation. She describes a secondary complaint of long standing left sided lower back pain.
Cognitive Beliefs
Patient reports that she believes that her thoracic stiffness and discomfort may be due to an irritated disc or nerve and that she is unable to touch it because it is inside and deep.
Diane’s question:
What finding in her story supports her belief that there is ‘an irritated nerve’? What symptoms are not present in her story that would support her belief that a thoracic disc is irritated?
Matthew's response:
I would have expected that if a thoracic disc was involved here she would have had some reports of numbness or tingling in the area of the back or possibly wrapping around the torso and even some discomfort in the chest. I would also expect that this would occur more frequently than with more intense and prolonged running. There would likely be a position that if maintained would create these symptoms if there was active disc bulging occurring. We also know from recent research that herniated discs do have the ability to heal and often do so in a 30 day period. Her symptoms have been going on for far longer than this. It is possible that with local irritation, that does not include a disc bulge or herniation, swelling can occur which could compress a nerve further exasperating her pain. She does describe her symptoms at times as “burning” which can be due to an irritated nerve.
Diane’s comment:
Yes, the recent classification of pain suggests that ‘burning’ is a neuropathic pain and almost always involves the nerve, but doesn’t suggest why the nerve is irritated.
Meaningful Tasks
Patient reports that running long distances is a big part of her life for her overall fitness and recreation which is also what is aggravating her middle back. She also reports that trunk rotation to the left creates tension in the left upper back and that prolonged sitting will tend to aggravate her left lower back.
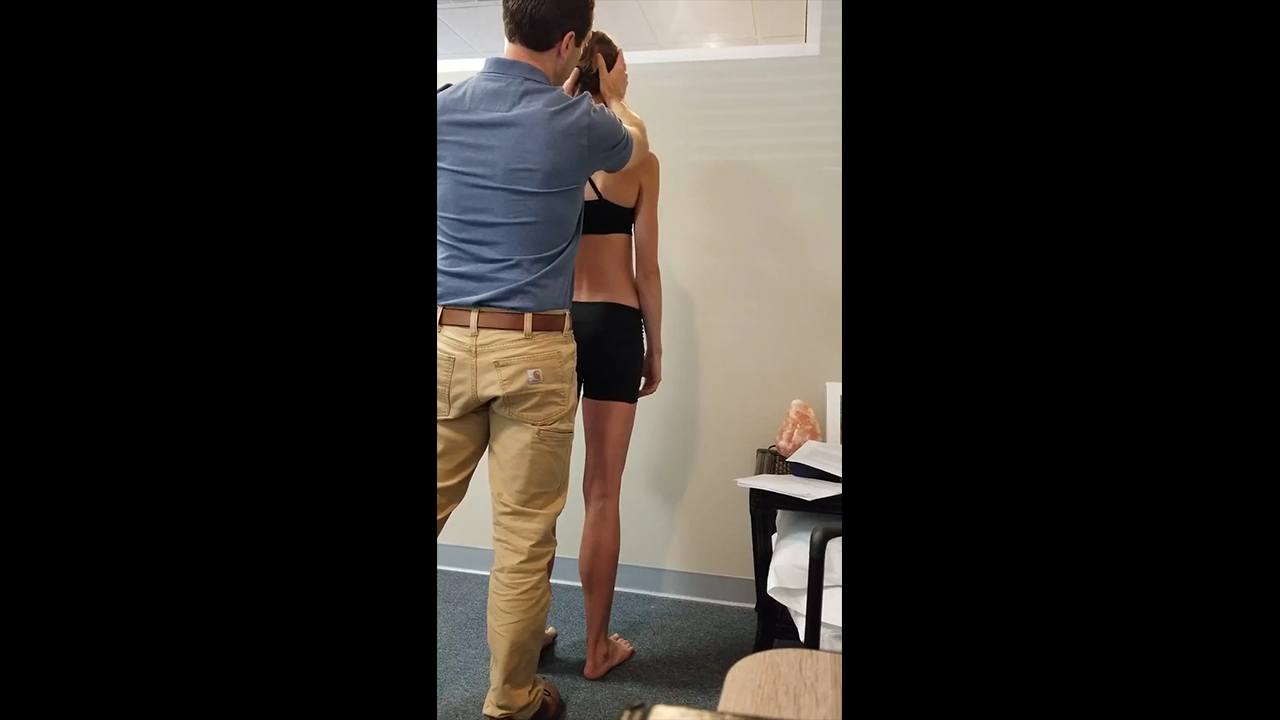
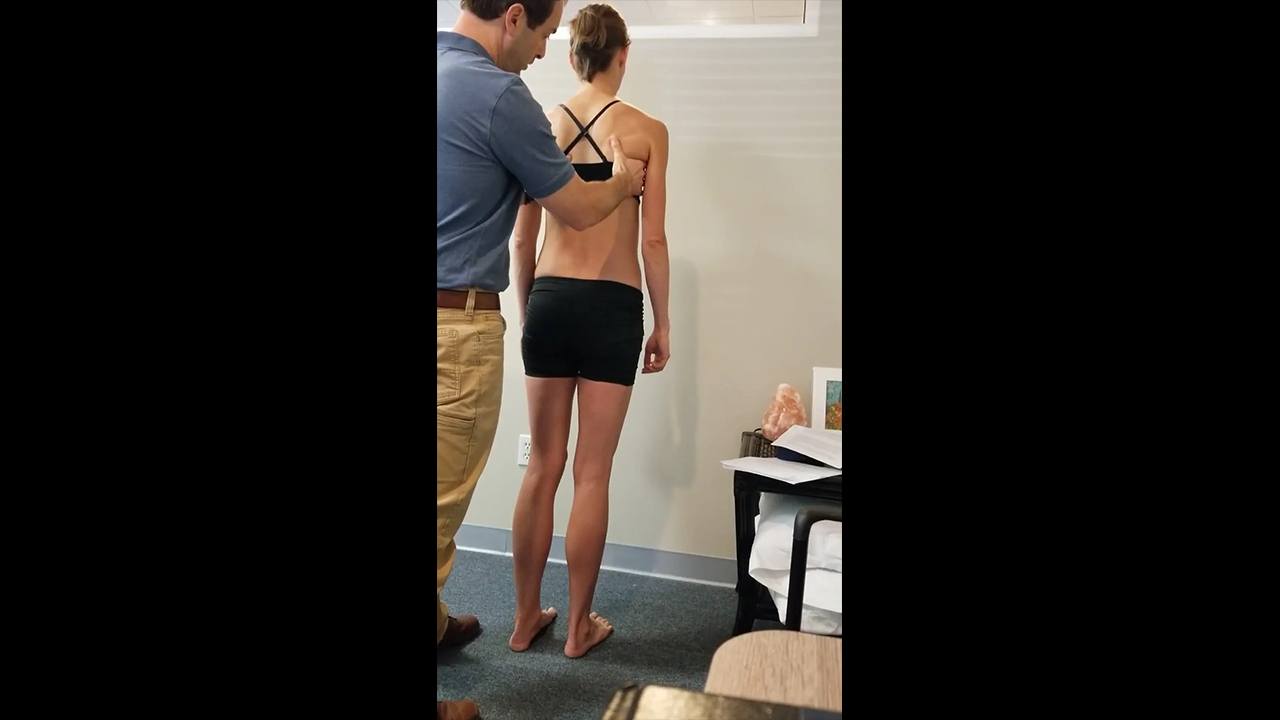
Her screening tasks that were assessed include a standing screen to better understand the position she is starting from, single leg stance which is a component of running as well as trunk rotation to the left which is also a major component of running and something she can reproduce symptoms with in the clinic.
Diane’s question:
What would be appropriate screening tasks to evaluate if this session were to focus on resolving her low back pain with sitting?
Matthew's response:
I would have likely picked squatting as a screening task for her complaints of lower back pain with sitting.
Screening Tasks
Standing Screen
Functional Unit 1
- Pelvis: Is in a transverse plane rotation (TPR) to the left associated with a left intra-pelvic torsion (LIPT)
- Hips: Right hip is anterior (congruent with the TPR of the pelvis)
- Thorax: Thoracic ring 9 is translated left/rotated right (this is not congruent with the position of the pelvis). Thoracic ring 4 is translated left/rotated right (this is congruent with thoracic ring 9 but not congruent with the pelvis) Thoracic ring 3 is translated right/rotated left (this is incongruent to thoracic rings 4 and 9 but congruent with the position of the pelvis). Thoracic ring 3 and 4 are “glued” as correcting one makes the other worse and vice versa. This means that they are unable to move independent of each other and that when one moves in one direction the other will not correct but maintain its incongruent state to the other thoracic ring it is glued to.
Functional Unit 2
- Cranium: There is a right intracranial torsion (the right temporal bone is rotated posteriorly bringing the right mastoid process anterior compared with the left side) with a congruent right rotation of the sphenoid (the sphenoid is felt to be more posterior on the right and more anterior on the left. This can also be seen when looking at the patient from the front as her right eye appears to be more posterior).
- Cervical: C2 is translated right/rotated left (this is incongruent to the position of the cranium); C7 is translated to the left and rotated to the right (this is congruent with the position of the cranium but incongruent with the position of C2.
- Upper thorax: The manubrium is rotated to the right (this is congruent with the position of the cranium and C7 but incongruent with the position of C2) and the ribs and vertebrae of thoracic ring 2 are translated right/rotated left (this is congruent with the position of C2 but incongruent with the position of the cranium, C7 and the manubrium). This reflects an intra-thoracic ring incongruence in that the manubrium should follow the rotation of the vertebra of the ring.
Diane’s question:
Since the manubrium is an integral part of the 2nd thoracic ring what would cause it to rotate incongruent to the ribs and vertebrae of this ring?
Matthew's response:
The 2nd rib articulates with the manubrium at the manubrial-sternal junction on both sides. Since the clavicle and the 1st rib also articulate with the manubrium they along with the 2nd rib can have an impact on the position of the manubrium. There are significant neurological and vascular structures that can become impacted by a lack of mobility of the 2nd thoracic ring. A left clavicle that is retracted will cause the posteromedial aspect of the clavicle to become compressed at the SC joint and slightly posteriorly relative to the manubrium. This could cause the manubrium to rotate to the right if the medial end of the clavicle is posterior enough to the manubrium and imparts a posterior to anterior force on the lateral aspect of the left manubrium.
Diane’s further question:
Below you mention that the left clavicle is depressed (and therefore should be posteriorly rotated). This is consistent with a left intra-shoulder girdle torsion which, if the thorax is congruent would cause the upper thorax to rotate to the left (manubrium included). But the manubrium is rotated to the right and the ribs of thoracic ring 2 are rotated to the left. So your hypothesis above about the clavicle causing the incongruence isn’t making sense to me! Also, if, as you suggest, the left clavicle is causing the manubrium to be right rotated, why wouldn’t the ribs of the 2nd thoracic ring merely follow the manubrium? There must be two incongruent vectors acting on the second thoracic ring to result in a rotation of the manubrium one way and the left and right 2nd ribs rotating another. This finding suggests you won’t have just a primary driver for FU#2 in your next task.
Matthew's response:
I agree that there must be 2 incongruent vectors acting here as the manubrium should have been rotated to the left. I would expect that if that was the case at least one of the vectors was likely coming from the underside of the manubrium. Could this be possible due to the trauma from the fall as a child? In any case I did not fully evaluate the mobility of the manubrium. I am also wondering now whether the manubrium appeared to be rotated to the right but in fact was rotated to the left. It is quite possible that upon palpation the manubrium appeared to be rotated to the right but could have had poor mobility to the right and good mobility to the left upon a spring test for instance. This would have confirmed its position relative to its mobility.
Diane’s response:
YES! I totally think it is possible that when she was ‘winded’ as a child it is biologically plausible that this set up a pull on the ligaments that connect the pericardium to the manubrium. However, if this was the only vector acting on the 2nd thoracic ring all of its bones would be rotating congruent so there are two vectors.
- Shoulder Girdle: The left scapula is downwardly rotated and anteriorly tipped (this is congruent with the position of C2 and ribs and vertebrae of thoracic ring 2. Her left medial clavicle is elevated compared to the right at the sternoclavicular joint (this is congruent with the position of the scapula as I would expect the left medial clavicle to be higher on the side of downwardly rotated scapula as the lateral end of the left clavicle would move inferior on that side gliding the medial end of the clavicle superior at the sternoclavicular joint) .
Diane’s question:
There are two joints that comprise the sternoclavicular joint. At which joint (medial or lateral) does the superior/inferior glide of the medial end of the clavicle occur? At which joint does the rotation of the manubrium occur? What is the potential impact on the structures emerging from the cervical spine of the manubrial rotation and superior glide of the clavicle?
Matthew's response:
The sternoclavicular joint is a synovial-saddle shaped joint that joins the clavicle and manubrium. This joint has a medial and lateral component. The medial and lateral component of the SC joint is separated by an articular disc. Inferiorly the medial end of the clavicle articulates with the first costal cartilage via the costoclavicular ligament. The superior aspect of the joint is reinforced via the interclavicular ligament, anteriorly via the anterior sternoclavicular ligament and posteriorly via the posterior sternoclavicular ligament. The superior and inferior glide that occurs at the SC joint occurs as the medial end of the clavicle glides superior and inferiorly on the lateral aspect of the articular disc that separates the medial end of the clavicle from the manubrium at the clavicular notch – therefore the lateral sternoclavicular joint. The manubrial rotation that can occur would do so at the medial SC joint where the clavicular notch of the sternum articulates with the medial aspect of the disc. There are many structures that can become compressed or have abnormal tension placed on them due to a rotation of the manubrium. These can include the vagus nerve, phrenic nerve, the carotid artery, jugular vein, brachiocephalic trunk, esophagus and trachea as well as many muscles that directly and indirectly attach to the clavicle such as the SCM, pec major and minor, subclavius, trapezius and deltoid muscles.
Diane’s additional comment:
Anything that prevents full rotation of the clavicle will alter tension of the various layers of the deep cervical fascia with the potential to impede venous drainage of the vena nervorum in the brachial plexus with the consequence of neuropathic symptoms in the upper extremity.
Functional Unit 3
- Feet: Both calcaneii are laterally rotated (L>R) relative to the respective talus which are plantar flexed and adducted relative to the respective calcaneus causing the hind foot to be in a position of pronation. The L midfoot appears to be in a position of pronation in standing but is supinated when the hind foot is placed in neutral. This appears to have more of a folding orientation in which the medial column is internally rotated and the lateral column is externally rotated relative to the 2nd Assessment of the individual joints of the mid and forefoot was not performed and would be necessary to determine the ability of each individual foot bone to move into both internal and external rotation and determine any mobility limitations. An assessment on whether or not there was a talar tilt was not performed. If this was done at the time of evaluation it would have assessed the ability of the talus to tilt medially and laterally at the talo-crural joint and whether the talus was compressed medially or laterally at the talo-crural joint.
Diane’s comment:
Excellent update on the foot terminology Matt!
The standing screen acted as a general assessment of where the patient presented in weight bearing. This was not chosen as a meaningful task as it does not correlate with her meaningful complaints as well as single leg stance and thoracic rotation would. She also does not present with any unlocking of her SIJ in standing and thus any corrections in standing would not have any meaning on her complaints or functional stability.
Single leg stance on the left
Diane's question:
What in the story/findings so far suggested that you just needed to assess the left single leg stance?
Matthew's response:
In an ideal situation I would have assessed both left and right single leg stance as running has both of these as part of the activity. This patient has both left sided pain which is also reproduced by left trunk rotation. The gait cycle is a complex activity that requires a stable trunk that allows controlled mobility throughout the body. During single leg stance on the left most notably mid stance to toe off which requires full posterior depression of the pelvis (PNF language) or left lateral tilt of the pelvic ring (ISM language) and subsequent left hip extension, internal rotation and adduction, the trunk will be moving through left rotation. Since her symptoms correlate with left trunk rotation left single leg stance was chosen for assessment.
Functional Unit 1
- Pelvis: There is an unlocking of the L SI joint when in single leg stance on the left. This occurs immediately as patient lifts the right foot off the ground.
- Left Hip: The left hip remained centered within the acetabulum during left single leg stance.
- Thorax: When going from standing with both feet on the ground to single leg stance on the left, thoracic ring 3 maintains its position of translated right/rotated left and thoracic ring 4 maintains its position of being translated left/rotated to the right. Thoracic ring 9 maintains its position of translation left/rotated to the right. In standing it was determined that thoracic rings 3 and 4 were glued and when correcting either thoracic ring the alignment of the other worsened. Ring stack and breath was performed in single leg stance on the left and this allowed both ring 3 and 4 to release their positions and come into neutral.
The driver for Function Unit #1 is the Thorax (Thoracic ring 4)
When the manual correction of the two glued thoracic rings (3 & 4) was released, thoracic ring 4 was the first to move into translation to the left and rotation to the right and then thoracic ring 3 moved into translation to the right and rotation to the left. When the thorax (thoracic ring 3 and 4) was corrected the L SIJ was able to maintain a stable position and did not unlock and thoracic ring 9 moved into a more neutral alignment. Manual correction of the pelvis did not correct the thorax.
Functional Unit 2
- Cranium: The right ICT continues to be present
- Cervical: C2 further translates right/rotates to the left, C7 further translates left/rotates to right
- Upper thorax: The manubrium remains right rotated and the ribs and vertebrae of thoracic ring 2 remain left rotated.
- Shoulder girdle: The left scapula remains anteriorly tipped and downwardly rotated. This places the left medial clavicle in a position of being glided superiorly at the left SC joint with the left clavicle as a whole being depressed.
The driver for Functional Unit #2 is the Cervical spine (C2)
A correction of C2 improved the position of C7 and seemed to improve the R ICT via visual inspection of the R orbit being less deep. Correction of C7 did not correct or improve the position of C2. A correction of the ICT did not improve C2.
Diane’s comment/question:
But what about the second thoracic ring and shoulder girdles? The 2nd thoracic ring has great interest for me as there is an incongruent rotation within the ring. The manubrium is rotated right and the ribs/vertebrae of the second thoracic ring are rotated to the left. What did a co-correction of the manubrium and TR2 do to C7, C2 and the ICT and visa versa?
Matthew's response:
I am not sure why at the time of the evaluation TR2 and the scapula were not given more consideration but it may have been because their positions did not get worse during the task of single leg stance. Looking back it should have been assessed whether or not C2 corrected the manubrium, TR2 and the positon of the scapula and clavicle and whether a co correction of the manubrium, TR2, the scapula and or the clavicle would have improved the other segments in functional unit 2 further which would have indicated a co driver being present. It is feasible to think that the anteriorly tipped and downwardly rotated scapular position was causing the left medial clavicle to elevate and compress at the SC joint. This could have been creating an environment in which the medial clavicle was in a sense pushing the manubrium into right rotation especially if the medial clavicle was slightly posterior at the SC joint.
Functional Unit 3
- Feet: The left calcaneus moved further into lateral rotation relative to the talus and the talus further plantar flexed and adducted (hindfoot pronation). This caused the left navicular to plantarflex and the medial column of the foot to externally rotate. There is the appearance that the talus did tilt laterally , compressing the superior-lateral aspect of the talus into the inferior lateral aspect of the distal tibia and fibula.
The driver for Functional Unit #3: Since the left foot was the only region assessed in functional unit 3 and it is a site of impairment it is the driver for functional unit 3.
Summary of Functional Unit Drivers:
- FU1: Thorax (Thoracic ring 4)
- FU2: Cervical Spine (C2)
- FU3: Left Foot (hindfoot)
Final whole body driver for left single leg stance: Cervical Spine (C2)
The patient reported that her left lower extremity and foot stability returned in left single leg stance when the correction for C2 was performed. She reported that she felt more stable on the left foot and she was able to maintain a neutral arch (the core muscles of the foot seemed to activate with this correction). It was noted that when C2 was corrected her L SI joint maintained stability and the left innominate did not anteriorly rotate in relationship to the sacrum. Looking back at this visit the thorax (thoracic ring 4) should have been evaluated for its corrected impact on C2 as well as for the patient’s experience as well as the impact of the correction of C2 on thoracic ring 4.
Diane’s comment:
Good reflection. You had already noted that correcting TR 3 & 4 resulted in restored control of the left SIJ, so if correcting C2 improved TR4 then you would have a clearer understanding of the relationship between C2, TR3 & 4 and the left SIJ.
There may have been a co-driver in this situation in which there would have been a much better improvement in the patient’s experience as well as on all sites of impairment with both corrected instead of just assuming that C2 was the primary driver for all functional units.
Diane’s response:
Excellent reflection Matt! Also, if you don’t have any information about the within ring incongruency of TR2 and its relationship to C2, this would be another consideration.
Trunk Rotation to the Left
Left trunk rotation is limited by 50% with reports of L upper thoracic stiffness and discomfort at the time of evaluation.
Functional Unit 1
- Pelvis: Maintains intrapelvic torsion as she rotates to the left. Although the right innominate rotates anterior and the left innominate rotates posterior relative to each other, the sacrum maintains an optimal relationship with the innominate on each side; in other words the sacrum remains nutated relative to the innominate bilaterally throughout the movement of twisting to the left. Biomechanics and control of the pelvis was optimal for this task.
- Hip: The right hip starts further anterior than the left at the start of the twist and moves with the pelvis anterior while the left hip maintains its centered position in the acetabulum moving posterior in space. This is suboptimal biomechanics for the right hip.
- Thorax: There is maintenance of thoracic ring 3 position of translation right/rotation to the left as well as thoracic rings 4 and 9 being translated left/rotated to the right. During the twist it was felt that thoracic ring 4 further translated left/rotated right and became “stiff” under my left hand. This did not occur with thoracic ring 9 and to a much lesser degree thoracic ring 3. This is suboptimal biomechanics for the 4th and 9th thoracic rings.
Driver for Functional Unit #1 is the thorax (Thoracic Ring 4)
Since there was maintenance of the intrapelvic torsion in this task the pelvis was ruled out as a driver for this task.
Diane’s comment:
It may be more appropriate to say that the biomechanics and control of the pelvis were optimal for this task meaning that the pelvis is not a site of impairment so not considered for driver assessment since its performance was optimal.
Correcting the right hip did not have any effect on the patient’s symptoms or her ability to rotate to the left nor did it change the alignment or biomechanics of thoracic rings 3, 4 or 9. Correction of thoracic ring 9 had no effect on the alignment or biomechanics of thoracic ring 3 or 4 or the R hip. Thoracic rings 3 and 4 were glued and the correction here was accomplished with the ring stack and breathe technique. When thoracic rings 3 and 4 were corrected the patient was able to perform full trunk rotation to the left without any symptoms. The correction of thoracic rings 3 and 4 corrected the alignment and biomechanics of thoracic ring 9. At the time of the examination I did not assess the impact of the ring correction on the right hip position. In order to differentiate whether thoracic ring 3 or 4 was the priority ring in this unit a correction was made again using ring stack and breathe. Once thoracic ring 3 and 4 were able to move independent on each other and brought to a neutral position I gently released the correction with my hands and felt that thoracic ring 4 had a sudden (prior to thoracic ring 3) movement into translation left/rotation right followed by a gentler translation of thoracic ring 3 into translation right/rotation left. This indicates that thoracic ring 4 is primarily creating the environment that is impacting the position of thoracic rings 3 and 9.
Functional Unit 2
- Cranium: Right ICT with congruent right rotation of the sphenoid persisted. This did not change from the neutral standing position into left trunk rotation. This is incongruent biomechanics for this task.
- Cervical spine and upper thorax: C2 remained translated right/rotated left with left trunk rotation. C7 remained translated left/rotated right with left trunk rotation
- Upper thorax: The manubrium remained right rotated and the 2nd ribs and T1-2 remained left rotated during the task.
- Shoulder girdle: was not assessed at the time of evaluation
Driver for Functional Unit 2 is the Cervical spine (C2)
Correction of the cranium did not have an impact on the task and the patient’s experience of left trunk rotation. Correction of C2 did correct the right ICT as well as C7. Correcting C7 had no impact on C2 or the cranium and correcting the cranium did not have an effect on C2. As in the task of single leg stance on the left, the manubrium and thoracic ring 2 were not corrected to see what their impact on the other areas of functional unit 2 would have been. Correcting C2 had an impact above and below but did not correct thoracic ring 2 or the manubrium. This again may have been a case where C2 and the second thoracic ring could have been co drivers or thoracic ring 2 a secondary driver in functional unit 2. The primary driver in functional unit 2 was determined to be C2. With that said C2 did not improve the range of motion of the patient’s left thoracic rotation and the patient reported that it did not change her experience.
Diane’s comment:
In the left single leg stance task, correcting C2 improved TR4 and restored control of the left SIJ; however, in this rotation task correcting TR4 improved the task and not C2. This is highly suggestive that TR2 and the incongruent alignment within this ring was indeed involved in this task.
Functional Unit 3
- Feet: During left trunk rotation the patient’s left foot was able to fully supinate and her right foot was able to fully pronate. This is what an efficient foot and ankle would do during a twist to the left. No further assessment of the foot and ankle was performed at this time as there did not appear to be any limitation in their ability to move efficiently with the twist.
Summary of Functional Unit Drivers for the Whole Body Left Standing Twist Task
Priority of Unit Drivers #1 and #2: Thorax (Thoracic ring 4)
When thoracic rings 3 and 4 were corrected, the patient’s cranium and cervical spine corrected as well. This indicates that thoracic ring 4 is the primary driver for functional unit 1 as well as functional unit 2. The feet demonstrate optimal function in the left body twist, therefore TR 4 is the final driver for this task. A further assessment of correcting the manubrium and thoracic ring 2 could have been done at this point to determine its impact on C2 and TR4. If a correction of the manubrium and TR2 corrected C2 and TR4 this would have been the primary driver for both functional unit 1 and 2.
Diane’s comment:
Or TR2 may have been a co-driver.
Further Assessment of the Drivers, including Vector Analysis
Assessment of the above screening tasks determined the following drivers:
- Single leg stance on the left: Cervical spine (C2)
- Trunk rotation to the left: Thorax (Thoracic ring 4)
It is possible that thoracic ring 4 may have been a co-driver for single leg stance on the left. This was overlooked at the time of her visit but in any event both C2 and thoracic ring 4 were further assessed.
The lack of assessment of thoracic ring 2 and its impact on C2 and TR4 makes it difficult to completely rule out TR2 as a driver, co-driver or secondary driver for either task.
Further assessment of C2 and TR4 could include some or all of the following: active and passive mobility as well as active and passive control testing. In order to further assess CR2 and TR4 vector analysis was used during both active and passive mobility tests to determine which system the impairments were located. This can be in the visceral, neural, articular or myofascial systems.
Impact of Drivers on Motor Control Strategies: This could assess the impact the driver’s position on the ability for the core to initiate a core first contraction under load as well as its impact on the core’s strength and endurance.
Further Assessment of C2
During standing and single leg stance on the left the following was noted:
Positional findings of the bones and joints of the craniovertebral region:
Right intracranial torsion: OA joint- the occiput is rotated right and side flexed to the left relative to C1. Arthrokinematically, the right occipital condyle is posterior on C1 and the left occipital condyle is anterior on C1.
C2/3: C2 is rotated to the left, side flexed to the L and translated to the right, relative to C3. Arthrokinematically, the right inferior facet of C2 is superior-anterior-lateral and the left inferior facet of C2 is inferior-medial-posterior on C3.
AA joint: The AA joint is rotated to the right when C2 rotates to the left, side flexes to the left and translates to the right relative to C1. Arthrokinematically, the right superior facet of C2 is anterior on the right inferior facet of C1 and the left superior facet of C2 is posterior on the left inferior facet of C1.
The cranium is congruent with the position of C1 (relative to C2) but the cranium and C1 are incongruent with the position of C2 in its relationship to C3.
Active range of motion: decreased rotation of the head and neck to the right (70%) more than to the left (80%).
Diane’s question:
Was this limitation noted at C2-3 or the AA joint?
Matthew's response:
The limitation was at the AA joint.
Interestingly in supine, C2 was translated left/rotated to the left relative to C1 (AA joint) which limits mobility in the left extension diagonal. This is opposite to what was found in standing and likely indicates that C2 is adapting in the upright, gravity dependent position. changing the demands placed on the system.
Diane’s comment:
This is why mobility assessment in the position of the meaningful task is so relevant in ISM. The vector that is perturbing the alignment and biomechanics of the AA joint is not present in the supine position! The AA joint is supposed to be the most adaptive joint in the neck and here, it is evident it is performing well, in that the joints between the atlas and axis are not limited; however, there is a vector of force that appears in the standing and left single leg stance that prevents mobility of the AA joint and this has the potential to impact head and neck function when running – especially when the head and neck rotation is considered in relationship to what the upper thorax (including TR2 and TR4) have to do when we run.
Passive mobility: In order to determine what system impairment was limiting the mobility of the AA joint a passive mobility correction combined with listening on both the correction and release of the correction (vector analysis) was performed in sitting. The AA and the C2-3 joints were able to be corrected through C2, ruling out an articular restriction at both segments and when the correction was let go, a pull was felt from the right side of C2 up into the sub cranial region that coincided with the right rectus capitus posterior major (RCPM) (neural vector). What this felt like was a pull to the right side of the occipital bone down to the spinous process of C2 which is the origin and insertion of the RCPM creating what felt like an anterior glide of the right superior facet of C2 on C1.
When this muscle was palpated, it was reported to be quite tender and a hardness was felt. No active or passive stability tests were performed at this time. If the vector was determined to be due to joint stiffness and a joint mobilization technique in this area were indicated upper cervical ligamentous testing would have been performed prior to this.
Hypothesis
The tension in the R rectus capitus posterior major was likely creating tension at C2 pulling C2 into a left rotated position relative to C1. It is biologically plausible that this change in alignment at C2 could change both the dynamics of the nervous system and the neural firing patterns to create dysfunction in both the neural and fascial systems ultimately limiting the patient’s ability to maintain stability in her L pelvic girdle and foot. This was likely creating a situation in which centrally the nervous system was unable to guide the body into how to create core stability at various regions in the body with this task.
Further Assessment of Thoracic Ring 4
Active and passive trunk rotation as a whole to the left was limited to 50% and the left rotation of TR4 was limited to less than 10%. Patient also reported tension in the upper to middle left thoracic region with both active and passive trunk rotation to the left. Palpation of thoracic ring 4 during active and passive left trunk rotation revealed a hardness that was felt under the hand as the thoracic ring further translated to the left. A correction of thoracic rings 3 and 4 was performed in standing and when let go thoracic ring 4 was pulled into right rotation with corresponding left translation. Passive listening at this time revealed that thoracic ring 4 was being pulled into left translation by a vector coming from the front of the left chest wall in the region of the pec minor muscle. The fact that both the 3rd and 4th thoracic rings could be fully corrected rules out an articular restriction at either thoracic ring.
Diane’s question:
Considering the anatomy (origin and insertion) of the pectoralis minor muscle, over-activation of the fascicle to the left 4th rib may be thought to posteriorly rotate the rib and thus result in left rotation/right translation of the 4th thoracic ring. And yet, you are correct, this muscle does tend to result in left translation/right rotation of the relevant thoracic ring. How do you reconcile this?
Matthew's response:
The pec minor originates from the anterior aspects of ribs 3 to 5 near the costal cartilage and inserts into the medial/superior aspect of the coracoid process. I believe that the angulation going from lateral (coracoid) to medial (anterior rib near costal cartilage) biases a translation over a posterior rotation on the left side. The subsequent translation that will predominate will cause the entire ring to rotate to the right and not the left.
Diane’s comment:
I never thought of that mechanism! I’ve always suggested that it is easier for pec minor to move the scapula (tilt the scapula anteriorly as this patient has) than to lift the thorax and that as the scapula anteriorly tilts and the muscle shortens the left rib would anteriorly rotate thus inducing the entire thoracic ring rotation right/translation left.
The left pec minor muscle was palpated at the level of the left 4th rib and it was very tender to palpation and felt to be overactive with a hard quality (neural vector). Further assessment in side lying was performed and it was determined that the functional joint between the left pec major and pec minor was limited in its ability to allow these two muscles to slide on each other or their muscle play.
Diane’s question:
What type of system impairment would this be classified as?
Matthew's response:
The overactivation of the fibers of pec minor to the L 4th rib would classify as a neural system impairment. The lack of muscle play due to adherence between the pec major and pec minor on the left could be classified as a myofascial impairment.
If a costo vertebral joint was the reason that this thoracic ring was rotated it would have been difficult to correct and a vector would have taken the therapist to the posterior aspect of the ring at the joint. Since this was not the case no joint mobility testing was performed.
Diane’s comment:
Excellent clinical reasoning!
Hypothesis
The overactive fascicle of the L pec minor was likely creating a pull on the left 4th rib that pulled the 4th thoracic ring into a position of right rotation (the left rib moving into left translation and subsequent anterior rotation). This likely caused thoracic rings 3 and 4 to become compressed and glued limiting their ability to move on each other and limiting the patient’s ability to rotate her trunk to the left around this dysfunction.
Diane’s question:
Glued rings are usually secondary to intercostal or multifidus/rotatores vectors but I can see how pec minor could cause ‘gluing’ of rings 3 & 4 IF there was overactivation of fascicles to both the third and 4th ribs.
Matthew's response:
It is very possible that what I felt was over activation of both 3rd and 4th rib fascicles of pec minor on the left. What I felt was that the 4th ring moved first which may indicated that the rings although glued, when corrected were able to move a little bit independently on each other and why the 4th ring moved first. Wondering if there could have been overactivation of the multifidus/rotatores as well but this was underlying what the pec minor was doing which was the primary vector.
Initial Treatment Session
Patient’s initial treatment session consisted of release of the R rectus capitus posterior major along with instruction in self release of the rectus capitus posterior major and axial elongation with gentle resistance to C2 in both supine and sitting for her neuromuscular re education. After treatment patient was able to perform her L single leg stance without unlocking of the L SIJ and was able to maintain a neutral arch on the left foot and neutral C2 alignment.
Release of the left pec minor muscle was performed in right side lying and patient’s breath was utilized as a functional movement pattern to facilitate this release and awareness of this area. When patient returned to standing she had full L trunk rotation without any pain. She was made aware of the left 4th rib and was instructed to monitor this rib for any further translation to the L if she finds that her L rotation becomes tight again. She was instructed to self-assess this if she starts to develop pain during a run. She was also instructed in self mobilization of the left pec minor muscle and encouraged to create some space in this area when practicing her left rotation. Patient was also educated on potential postural reasons why she may be having these issues both in her car, at home and work.
Followup treatment sessions
The patient was seen for 2 additional treatment sessions spaced 2 weeks apart with the first follow up being 2 weeks after the initial session. When she returned for her first follow up session she reported that she has been running a fair amount and noticed less pain in the left upper thoracic region and that her pain came on later in the run than she was used to. She also reported that her L thoracic rotation continued to improve and that she was generally much more comfortable throughout her day.
Objectively, during her first follow up session she demonstrated a significant improvement in her left thoracic rotation with TR4 being able to rotate to the left 90% before feeling the rib lose its springy end feel. She also demonstrated maintained stability of the left SI joint with single leg stance on the left. These sessions continued to focus on manual techniques to release the suboccipital muscles as well as the L pec minor muscle. At her 3rd treatment session she demonstrated full rotation to the left of TR4 with a springy end feel noted.
Postural training was also a big part of these sessions. Training her alignment started in standing and progressed to walking and running at home and focused not only on the position of TR4 but on the relationship of her thorax over her pelvis. Attention was placed on stacking the rib cage in a vertical position over the pelvis. The patient was able to feel the impact of neutral alignment on the forces transferring through her body into her base of support/feet. Once she was able to move toward a neutral standing posture with minimal cuing alignment with one foot in front of the other was trained. This was followed by training in proper weight shifting and weight acceptance onto the forward leg. She tended to lift her thorax into a backward bending position when she progressed forward over the front leg and was trained in maintaining a vertical positon of her rib cage. Her home program included repeated weight shifting while looking in a mirror to maintain a vertical rib cage and was also instructed to monitor the position of TR4 at times to make sure there was not a tendency for this ring to move back to its left translated position/right rotated. She was then instructed to pay attention to her alignment with her walking throughout the day. By the third session she reported that she had been running with much more awareness of the position of her thorax and felt that she was able to maintain a vertical alignment for most of her runs. She reported that when fatigue set in she noticed the tendency to lift her sternum. This was likely due to more of a strength and endurance issue and she was asked to avoid her running past the point of being able to maintain her alignment in order to build up her tolerance to running with good alignment.
Conclusion
Although Laura was only seen for 3 treatment sessions we were able to identify some key issues that limited her ability to run more efficiently and to perform her left trunk rotation. A follow up email from her a couple months later indicated that she had done a marathon and did not have any appreciable discomfort in her thoracic spine during this race. She reports being very happy with the outcomes and plans to slowly increase her running mileage paying close attention to her alignment. We also discussed the importance of cross training and the idea of balancing her training with some additional strength and mobility training. We also discussed the idea of having a true off season from running to allow her body to rest and recover.
Skills Demonstration
Case Study Author
Clinical Mentorship in the Integrated Systems Model
Join Diane, and her team of highly skilled assistants, on this mentorship journey and immerse yourself in a series of education opportunities that will improve your clinical efficacy for treating the whole person using the updated Integrated Systems Model.
We will come together for 3 sessions of 4 (4.5) days over a period of 6-8 months with lots of practical/clinical time to focus on acquiring the skills and clinical reasoning to put the ISM model into practice. Hours of online lecture and reading material and 12 hours of in-person lecture are...
More Info