Story
Ms. CS was assessed on January 31, 2024 at Habitat Health in Vernon, BC. She is a 28 year old female that works as a Licenced Nurse Practitioner at an Extended Care Facility. She currently does not engage in any recreational or sporting activities and reports low stress levels in her personal and professional life, although she marked anxiety in her intake form. She used to work as a Care Aid before becoming a nurse and reports perceiving her current job as less physically demanding. Her current position involves distributing medication which requires standing in front of the medical cabinet with her arms held at shoulder height and looking down while she is organizing medication. She then has to walk short distances to deliver the medication to the residents. Occasionally she is the only nurse on staff and needs to attend for medical exams of the residents for any urgent issues. She reports spending 90% of her work shift on her feet either standing or walking and identified her position in front of the cabinet as most irritating for her current presentation and in the past, causing tension in her neck with rare headaches (2-3 per month).
Her complaints on initial visit were severe soreness over the left shoulder/neck area that started overnight 3 days prior to the assessment with no apparent causation factors. She also noted swelling in the supraclavicular area on the left, severe tenderness with palpating the trapezius area (she asked her partner to massage her shoulders and was surprised at finding this focal point of tenderness) and occasional sharp shooting pain radiating down the left arm to the elbow. The soreness in the neck area was reported as constant, throbbing and she could not identify a position that relieved the symptom even at night. She reported using OTC anti-inflammatories and ice both of which helped the symptoms temporarily.
Her goal was to be able to return to work with no pain and to be able to find a rest position that would allow her to sleep uninterrupted.
Past Medical History
Ms. CS reports ongoing neck and bilateral shoulder tension related to work demands as described above with occasional headaches that start in the occipital region. She also reports having rare episodes of migraines (2-3 per year). While working as a Care Aid in the past, she had low grade low back discomfort related to lifting and carrying. This has improved since changing her career but her low back can get fatigued at the end of a work shift. She has attended physiotherapy for neck and left shoulder symptoms following a work injury in January 2022, her symptoms improved with 2 sessions then she discontinued the treatment. She denies any other MSK injuries or accidents.
Other medical interventions include tonsillectomy and adenoidectomy as a child, asthma, anemia, varicose veins which were not discussed in detail during the initial visit.
- Diane’s question:
There are three phenotypes of pain; nociceptive, neuropathic and nociplastic. Which features from this story qualify as nociceptive and which as neuropathic and given that she has experienced ‘tension in her neck’ with headache ‘in the past’ how do you know there isn’t also some nociplasticity present in this presentation?
- Mara’s response:
Nociceptive pain is pain arising from noxious stimuli to the peripheral tissues that are mechanically or chemically altered. In this story, the words “soreness” and “tenderness” used by the patient to describe her pain would point to this phenotype as well as description of swelling, which would indicate an inflammatory process. The patient also reports that use of medication and ice decreased her symptoms temporarily. Typically, the nociceptive pain has a predictable change with mechanical load.
Neuropathic pain is pain related to changes in the sensory nerves, and the description of the occasional sharp shooting pain radiating distally could be features of this phenotype.
Nociplastic pain is pain perpetuated in the central nervous system even in the absence pf a peripheral stimulus. This is usually present in chronic pain situations and the main features are widespread areas that cross over multiple dermatomes, no relationship with mechanical load and descriptive words such as burning, deep throbbing. It usually presents along a large emotional dimension and could present with an increased sympathetic nervous system activation. In this presentation, the fact that her pain was “constant, throbbing and she could not identify a position that relieved the symptom even at night” could potentially indicate some nociplastic features.
- Diane’s comment:
Most chronic case so have a ‘blend of phenotypes of pain’ as you describe.
Cognitive and or Emotional Beliefs
During our interview and throughout the assessment, I was able to identify some recurring cognitive beliefs around pain that I believed needed to be addressed. Ms. CS was focused on her goal of decreasing pain and was not able for the past 3 days to observe what exactly she was doing, or not doing, to change the pain levels. As she experienced in 2022 with her previous episode, she expected her symptoms to be quickly relieved with local treatment of the soft tissues and was not prepared to problem solve during the interview. Once the reason for the thorough assessment following ISM principles were explained, she admitted that a long term resolution would be of interest to her and was more cooperative. She did not seem to have a strong emotional component in her presentation and was quite pragmatic in her description if her symptoms, likely a result of her profession, but did report her mood to be affected by the lack of continuous sleep for the past 2 nights.
- Diane’s comment:
There is more information in the paragraph above that suggests an element of nociplasticity here. What am I referring to?
- Mara’s response:
Her inability to increase or decrease her symptoms with motion, position change or rest could be seen as features of nociplastic pain.
Meaningful Complaint
In summary, Ms. CS has pain in her left side of the neck to the left shoulder, in the anterior and posterior regions with occasional sharp shooting, electrical pain from her left lateral shoulder to the elbow. The pain is constant and is made worse by sustaining an upright position, she did not identify a particular motion or task that she could not perform due to pain. When resting in supine or sidelying, she reported the pain improving but not completely resolving. The sharp shooting pain would occur randomly, usually with sudden motion and she was not able to identify a particular movement that could reliably reproduce this pain.
Her symptoms suggest a nociceptive phenotype, but the description of the sharp, shooting pain radiating distally from the main area made me include a neuropathic pain phenotype, although the typical presentation of tingling and numbness was missing. I was considering a restriction of nerve mobility in the area as a source of these symptoms and not a nerve conductivity issue.
Meaningful Task
As Ms. CS could not identify a particular motion or activity that was related to her symptoms, I performed an active ROM screening for the neck and found that the right side flexion motion was significantly restricted, worsened her pain and reproduced the sharp shooting pain into her arm. We decided together to use this as a meaningful task.
Screening Tasks
I chose the start screen position in standing as this is how she spends most of her work day.
Screening task was right side flexion of the neck, as identified above
Functional Unit #1 (FU#1)
Start Screen: Standing
I started the assessment of FU1 in standing even though her symptoms were related to FU2 so I could identify if she had a stable pelvis and see where the thorax was located in space. On reflection, I could have started in FU2 and assessed the FU1 after finding a driver there.
- Diane’s question:
What finding in the pelvis would require you to always start in FU#1?
- Mara’s response:
When one of the sacro-iliac joints is found to be unlocking either in the start screen or task positions, the FU#1 should be assessed first to determine the driver. If the pelvis is unstable in weight bearing (in the sense that the sacrum and innominate bone joints are not in their expected relationship when under load), changes will be made by the body in FU#1 and 2 to adapt to this and the assessment findings will be influenced by this adaptation.
Pelvis: The pelvis was rotated to the left in the transverse plane, both sacro-iliac joints remained locked in standing (sacrum nutated relative to each innominate). This corresponds to a left intra-pelvic torsion (IPT).
Hips: The right hip was anterior to the left, following the pelvis, the right (R) femoral head was found centered to the acetabulum.
- Diane’s question:
In ISM, we often use the term congruent when one body region is found to be ‘following’ another body region. In what other context do we use the term congruent, or incongruent, and why is congruence relevant in ISM?
- Mara’s response:
The terms congruent or incongruent can be used to describe the relative position of two body regions either in the start position or while the body is in motion. In a static position, when two body regions are rotated in different directions, we would describe this as “incongruent”. Another situation is when observing the behaviour of a body region while in motion, knowing the expected movement that should occur. For example, when lowering into a squat the expected motion of the tibia is internal rotation relative to the femur, if the tibia is found to be externally rotating during this motion, then we would describe this as “incongruent” as the motion of the tibia is incongruent to the task.
Thorax: The lower thorax was R rotated/ left translated as a unit, I could not identify a particular ring that was rotated more relative to the others, this was the first incongruent finding where the thorax was rotated in the opposite direction to the pelvis.
The sternal region of the thorax was also right rotated and I was able to palpate TR5 as being the most right rotated/left translated ring.
- Diane’s question:
Would you consider this finding (TR5 being the most right rotated/left translated ring) to be significant enough to then assess the impact of a correction of this on the pelvis? How could a TPR of the pelvis be in relationship to her neck tension/pain and headache?
- Mara’s response:
Finding, and noting incongruencies, is a great way to guide the process of assessment, as this highlight things that are outside of pattern. As TR5 was the ring that was most rotated/translated, I used it to assess the relationship to the pelvis, but as seen below, correcting the pelvis did not change the position of TR5 and vice versa.
The relationship between a TPR of the pelvis and neck pain/headaches can be seen two ways. One is through an “intermediate” stop, such as TR5 where a rotation of the pelvis could cause one of the rings in the upper thorax to also rotate through tension in the long spinal muscles such as iliocostalis, then this ring would be in relationship to a cervical segment or the cranium causing the symptoms. Another way is to look at the dura that envelops the brain and the spinal cord and anchors on the sacral periosteum. Any change in the position of the sacrum could cause “torsion” or tension of this tough structure that is transmitted to all of the anchor points (C2-3, foramen magnum).
Lumbar spine: L5 was L rotated following the pelvis, the change in rotation between the incongruent pelvis and low thorax occurred gradually in the high lumbar/TL junction.
Screening Task: Right side flexion of the neck
Pelvis, Hips and Lumbar spine: No changes were noted in the hips, pelvis and lumbar region as expected.
Thorax: TR5 rotated further to the right into the task (worsened).
Driver for FU#1
Pelvis, supported by the following:
Correcting the pelvis (derotation in transverse plane) corrected the R hip, although there was no change in thoracic alignment, particularly TR5.
Correcting the TR5 did not change the pelvis, although it significantly improved the subjective experience of the task (right side flexion of the neck). As noted in my discussion with Diane in the Clinical Reasoning Form that preceded this written report, there could have been a rotation of TR3 that I missed as it was very hard to palpate this ring both in the axilla or over the anterior chest. My first interpretation was that the TR5 was the driver of this unit based on this subjective change, but on further analysis, TR5 did not change the rest of the thorax or the pelvis, so biomechanically it is not the driver. Onto functional unit #2 (FU#2) ….
- Diane’s comment/question:
In ISM, a body region driver improves the biomechanics of other sites of impairment AND also improves the patient’s experience of the screening task. In this case, her experience was best improved by correcting the alignment of TR5; however, this did not restore alignment of the pelvis, nor the hips, in standing. After considering how the pelvis can impact the neck tension and headache above, what is your clinical reasoning now as to why I think the pelvis is still a body region to consider going forward? And yes, definitely time to consider FU#2!
- Mara’s response:
The pelvis still needs to be considered as a potential driver considering the direct relationship between the sacral, cervical and cranial attachments of the dura sac. If I had chosen the pelvis as the driver for FU#1, I would have then assessed the impact of correcting the pelvis on the cranium or the cervical spine, bringing more clarity to this relationship.
As we will see further down, I was not able to fully correct the TR5 due to an articular vector, so this could explain why I did not get a significant change in the pelvis and vice versa, so the TR5 and pelvis could still be in relationship.
Functional Unit #2 (FU#2) Findings
Start Screen : Standing
Cranial region: The cranium was in a R intracranial torsion (with the occiput rotated to the right, the right temporal bone posteriorly rotated and the left temporal bone anteriorly rotated) with a congruently right rotated sphenoid, C1 and C2 were right rotated/left translated.
- Diane’s question:
The occiput is not capable of pure rotation to the right. What other motion occurs at the OA joint in conjunction with right rotation of the occiput? Did the ocular, auditory and oral lines appear horizontal? If so, then something within this cranial region has to compensate for this conjunctive motion. I doubt the AA joint was purely right rotated. Why? To answer this question, I am looking for the coupling of motion at the OA, AA and C2-3 joints that would explain how the ICT, C1 and C2 can appear to be all right rotated without the head massively sideflexed. (Hint: it’s about the atlas and it’s osteokinematics between the occiput and C2).
- Mara’s response:
At the OA joint, the rotation of the occiput relative to the condyles of C1 is a conjunct motion occurring with contralateral side flexion, so when the occiput rotates to the right, it also should side flex to the left, tilting the head to the left. Due to the banked articular surfaces of the C1, the side flexion motion is relatively small, with most motion occurring in an anterior to posterior direction.
At the AA joint, rotation is coupled with contralateral side flexion, while at the C2-C3 joint side flexion and rotation are coupled ipsilaterally. There is no pure side flexion at the AA joint.
When considering C1 motion and position relative to both the occiput and the C2, it can be seen as a “washer” that fills the space and adapts its position to minimize ligamentous tension between the two. Due to alar ligaments, rotation of the occiput is also associated with AA joint rotation in the same direction.
With all things above considered, a right rotation of the occiput would be associated with a small amount of left side flexion on the C1, a right rotation of the C2 with a right side flexion at the C2-C3 joint.
During assessment, I palpated the C1 and C2 to be left translated (transverse processes more prominent on the left) and assumed they would be right rotated but I did not note whether the head was side tilted.
- Diane’s comment & further question:
Well done, you are so close Mara! When the atlas rotates on C2, it descends and this slackens the alar ligaments and thus allows the atlas to potentially sideflex left or right. The OA and C2-3 joints do not have this motion variability and when the occiput rotates on the atlas it must sideflex contralaterally, and when C2 rotates on C3, it must sideflex ipsilaterally as you note above. The adaptable AA joint is the washer in between the occiput and C2 and to maintain the head in neutral in all 3 cardinal planes it will relatively rotate and sideflex to maintain this alignment. So the atlas must neutralize any residual sideflexion (left or right) and all of the right rotation of the occiput and C2; therefore while it may ‘appear’ to be right rotated – it is likely carried there in space by the occiput and C2 and your interpretation of this hands on data acquisition is that it is right rotated but is it? Why do I say it must be left rotated relative to C2, and not right rotated? The direction of its sideflexion is not predictable with this ‘left brain analysis’.
- Mara’s response:
After looking closer at the biomechanics of the region, it is unlikely that all of the segments were right rotated, and likely the C1 was left rotated on C2 as the head was not in an obvious side flexion. With the C1 left rotated relative to C2 and under the occiput, it’s left transverse process would have moved more posterior and I incorrectly interpreted that as a left translation.
- Diane’s comment:
You got it!! Your HODA (Hands on Data Acquisition) was correct but your interpretation (last A in HODA-A (Dr. Jo Abbott) was not supported by the known biomechanics of the region.
Cervical region: C2 to C5 were right rotated/left translated, C6 was left rotated/right translated. This was the first incongruent finding in FU#2.
- Diane’s comment:
Even more reason for me to wonder about the findings of the atlas. Everything from the cranium to C5 is right rotated. Given what you know about coupling of motion in the cervical region – why isn’t her head massively right sideflexed? Do you think one segment i.e. C6 is capable of reversing all the other segmental sideflexion?
- Mara’s response:
Yes, when all the cervical segments appear to be right rotated, this must induce a right side flexion of the head and neck and C6 alone would not have enough mobility to reverse all of this side flexion. I must have missed another incongruent segment, likely C1, that would have compensated for all the side flexion to maintain the ocular line parallel to the horizon.
- Diane’s response:
You got it!!
Shoulder girdles: Both clavicles were depressed but no rotation was found; upon further analysis of the case I realize this is an incongruent finding as everything else except C6 was right rotated, so the shoulder girdles should have followed that rotation, especially of the TR1 and 2.
- Diane’s comment & question:
I totally agree with this reflection; If the shoulder girdles were aligned congruent with the general right rotation of most of the cervical and upper thoracic segments, what would the anticipated rotation be of the right and left clavicles?
- Mara’s response:
When the shoulder girdle as a whole is right rotated, the right clavicle would be posteriorly rotated relative to the manubrium while the left clavicle would be anteriorly rotated.
- Diane’s comment:
We usually check the relative rotation between the left and right clavicle and not the manubrium which can be variable, so relative to each other you are correct.
Thorax: both TR1 and TR2 were right rotated.
Screening Task: Right side flexion of the neck
Cranial region: no change in the RICT. With a head and neck rotation task we expect the cranium to show some degree of mobility, with a right intracranial torsion when the head is turning to the right for example. I was not sure if the cranium would normally go through this change in a side flexion task. My instinct is to say no as there is not a lot of side flexion occurring at the cranio-vertebral region that would pull on the cranium. C1 stayed right rotated/left translated during the task, C2 translated to the right as expected during this motion.
- Diane’s comment & question:
I agree that there should be little change in the ICT during right sideflexion of the head; however, it doesn’t occur as a pure movement at the OA joint. What is the conjunct rotation of the occiput at the OA joint during right sideflexion of the head? Would this induce an ICT and if so, in which direction with right sideflexion?
- Second question:
How much do you think the atlas can translate at the AA joint given the anatomy of the anterior atlanto/dens joint? Can C1 sideflex relative to C2 if it is stacked in a neutral position? Why not? Therefore, what has to happen at the AA joint to allow sideflexion of the atlas on C2? When we talk about C2 translating – we have to consider that this is not at the AA joint but rather at C2-3. So when you say “C2 translated to the right as expected” in right sideflexion at which joint is this occurring?
Give me a hypothesis as to what should occur at the OA, AA and C2-3 joints in right sideflexion of the head and upper neck – what is the coupled motion of sideflexion and rotation at each joint. Then, we can discuss this more to see if her biomechanics are congruent to the requirements of the task.
- Mara’s response:
1. During a right side flexion task, at the OA joint there is a conjunct left rotation of the occiput which would induce a left ICT, and this should have reversed the R ICT present in the start position.
2. As noted in my answer above, due to the presence of the alar ligaments, there is no pure side flexion at the AA joint, side flexion occurring as a conjunct motion with rotation. So, if the start position is neutral, there should be no lateral translation and no side flexion. If the start position is in right rotation, I am inclined to believe that the right convex articular surface of C1 would glide posteriorly while the left articular surface would glide anteriorly. Both the right and the left sides would also move inferiorly off the “shoulders” of C2 articular surfaces. This inferior movement would decrease ligamentous tension between the C1 and C2 and therefore allow some lateral and anterior/posterior movement. The coupling of side flexion and rotation seems to be slightly controversial in the literature, with both ipsi and contralateral coupling being accepted, and I believe both scenarios are possible, depending on the start position (more in flexion or extension). If the occiput rotates to the left as noted above, it will induce a left rotation vector to the C2 through the alar ligaments, and this would result in a relative right rotation between the C1 and C2.
During a right side flexion task, the expected biomechanics of the upper cervical are as follows:
At the OA joint the right side flexion of the occiput on C1 would induce a left rotation of the occiput and therefore a reversal of the right rotation found in the start position. At The AA joint, if the start position is in neutral, there should be no side flexion available. Since the start position is in right rotation of C1 relative to C2, some lateral movement is possible for a slight right side flexion, which would be associated with a further right rotation of C1 on C2. At the C2-C3 joint, the right side flexion would be associated with a right rotation of the C2.
In my statement above (“C2 translated to the right as expected during this motion.”) I was referring to C2 translating on C3, and the statement is incorrect as a right rotation of the C2 on C3 would induce a left translation.
- Diane’s comment:
That is exactly the point I was hoping you would pick up – the direction of translation you reported “C2 translated to the right” means that C2 was rotated left and sideflexed left on C3 – this is incongruent with the requirements of this task.
Cervical region: C2-C5 had limited motion in right side flexion (the arthrokinematic motion expected was left translation), this could be due to the fact that they were already right rotated/left translated and no more left translation was available. C6 was also restricted in range during the task and no translation was palpated.
- Diane’s question:
To clarify, C6 started in right translation/left rotation. Which sideflexion would this position be coupled with? What should C6 have done in this task?
- Mara’s response:
In the cervical spine rotation and side flexion are coupled ipsilaterally, so when C6 is right translated/left rotated, this would normally couple with left side flexion. The meaningful task was right side flexion, so the expected motion of the C6 would be to translate left and slightly rotate right (as pure side flexion is not possible due to the orientation of the facet joints). During the task, C6 moved minimally towards right side flexion and I did not feel the expected left translation.
- Diane’s further question:
Now that we have sorted the error in interpretation of C2-3 (it was right translated and therefore left rotated/left sideflexed incongruent to the requirements of the right sideflexion of the head and neck task), can you think of another hypothesis as to why C2-5 had ‘limited motion in right side flexion’?
- Mara’s response:
The right side flexion of the head and neck task could have also been restricted in the C2-C5 region due to the incongruent motion of the C2 on C3, where C2 was translating to the right and inducing a left rotation/left side flexion motion.
- Diane’s comment:
Exactly!
No change in shoulder girdle position, TR1 and TR2 also did not change during the task.
- Diane’s question:
What is the coupled pattern of sideflexion/rotation for TR1 & TR2 in this task? If they are right rotated, is this congruent with the requirements?
- Mara’s response:
During the right side flexion task, the motion would occur as far down as TR2, with right side flexion being associated with a right rotation/left translation, so their start position in right rotation is congruent with the task and they would not be expected to change in the task.
- Diane’s comment:
All correct, except TR1 doesn’t translate relative to TR2.
- Mara’s response:
Thank you for the reminder, in the vertebro-manubrial region there is limited translation and anterior-posterior arthrokinematic motion.
Driver for FU#2:
Cervical driver, segment of interest C6 supported by the following:
Cranial correction made no changes in other areas.
Correcting C6 significantly improved the range of right side flexion and associated symptoms. It did not change TR1 or TR2 position or the C1 position, I could not assess the cranial response to this correction.
- Diane’s question:
What was the barrier to being able to assess the response of the cranium to this correction? I think it is a critically missed part of this. On reflection, can you think of a way that you could assess if the RICT changed with the correction of C6? C6 did not change TR1 or TR2 or C1, so, you certainly have some secondary regional drivers in this unit other than C6.
- Mara’s response:
I used both of my hands with a key grip to distract and derotate the C6 then held my right finger pads on the anterior tubercles of the right transverse processes and the thumb on the posterior transverse process. This freed up my left hand to palpate the impact of this correction on the other areas. When palpating the cranium with one hand, I could only palpate one mastoid process at a time and this was not accurate enough for me to determine if the ICT was changing or not.
One way I could have assessed this better was to ask the patient to either hold the C6 corrected so I could use both my hands on the cranium or to place her thumbs on the mastoid processes and note any change when I released the C6 correction.
- Diane’s comment:
Another way is to hold C6 as you describe with your right hand, then pronate your left forearm so that you can palpate the left mastoid process with your left thumb and the right mastoid process with either the index, middle or ring finger (whichever reaches). Then when you release the correction of C6, palpate/listen to what happens to the RICT. If the ICT returns to the right, it means your C6 correction improved the cranium. If the ICT doesn’t change, then there was no impact on the cranium with this correction of C6.
Correcting TR1 or TR2 did not change C6, cranial region or the experience of the patient. I did not test TR1 relative to TR2 as I was looking for incongruencies.
- Diane’s question:
With the new information about C2, my remaining question would be whether C6 corrected C2. It probably did otherwise you wouldn’t get a positive experience response in the task.
- Mara’s further comment:
I agree since correcting C6 did not change the position of C1, something else must have corrected above it to account for the significant increase in the range of side flexion available.
- Diane’s comment:
I suspect it was something in the cranium.
Relationship of Drivers from FU#1 and FU#2
At this point of the assessment, I still considered TR5 as the ring of interest for FU#1 so I assessed the relationship between TR5 and C6 as both of them had a significant impact in improving the neck right side flexion and the subjective experience. Correcting TR5 improved C6 partially in standing, correcting C6 did not change the position of TR5. Best correction was TR5 and C6 together; therefore they were co-drivers.
- Diane’s comment:
I would still really want to know the impact of this co-correction on the TPR of the pelvis; why?
- Mara’s response:
As discussed above, the pelvis could be in relationship to the FU#2 driver through tension in the dura, and nothing else improved the TPR of the pelvis.
- Diane’s comment:
This would bring us full circle to the cranium again.
Upon reflection, this could be interpreted as an acute neck driven neck pain and further assessment of the FU#1 could have been done later as the TR5 is not biomechanically the driver for FU#1.
Functional unit #3 (FU#3) Findings
I did a quick visual screen of the FU#3 lower extremity and no significant impairments that would require further assessment were found.
I also did an active ROM screen of the upper extremities (before assessing for drivers, when we were looking for a screening task) and no restrictions or alignment impairments were noted.
Considering the neuropathic pain presentation noted above, I decided to test the drivers in the context of neural tension. The upper limb tension test for the median nerve was positive in standing with a reduction of available elbow extension and pain reproduction in the familiar area of the neck and shoulder. Correcting the TR5 and C6 did not change the tension in the median nerve. My interpretation was that the changes in position and biomechanics of these two regions were not due to excessive neural system tension, in other words, they were not compensating for a neural system impairment, which allowed me to move on to further assessment of these two regions.
- Diane’s question:
How did you rule out that the C6 position was not secondary to neural tension as opposed to C6 causing the neural tension? Perhaps this position is a way that the MSK system is reducing traction/tension on the right emerging nerve root. There is a classic sign/symptom that happens when correcting C6 if this is the case – what is it? It is fundamentally how ISM helps us to differentiate MSK causing neural tension vs the nerve itself causing MSK malalignment.
- Mara’s response:
If correcting the C6 would have caused an increase in neural tension (in this case less available elbow extension with ULNTT for the median nerve) then the interpretation would be that the rotated position of C6 is a compensation for the neural tension, so the MSK system is “shortening” to adapt to the neural tension. On the other hand, if correcting the C6 position improves neural tension (more ROM available with ULNTT) then we can assume that the rotated position of the C6 is causing the neural tension.
So in short the two scenarios would be:
- nerve tension causing MSK malalignment: correction of the segment worsens neural tension
- MSK malalignment causing neural tension: correction of the segment lessens neural tension
In this patient presentation, correcting the C6 made no change in the median nerve tension, therefore my interpretation was that the neural tension and C6 were not in relationship (one causing the other). The median nerve dynamics could be restricted in other regions along the pathway (clavi-pectoral space, under pectoralis minor etc.) The purpose of this test for me was to confirm that the change in position of C6 was not due to neural tension so I could continue along with my hypothesis of C6 and TR5 being the drivers.
- Diane’s comment:
Perfectly reasoned!
Further Analysis of the Drivers
Thorax driver: (TR 5 priority ring)
Active Mobility
TR5 was assessed with thoracic rotation and breathing motions. The posterior rotation of the left rib expected during inhalation and left rotation motions was found restricted.
- Diane’s comment and question:
Active mobility testing in ISM is in relationship to the requirements of the meaningful task. For Ms. CS her meaningful task is standing, so what are the active mobility requirements of TR5? To answer what the active mobility of TR5 was, we need to know if she could actively (no assistance from you) rotate her TR5 how far and which way?
- Mara’s response:
The MT did not require any motion of the thoracic spine but the active mobility test would assess the ability of TR5 rotate to the left to neutral from the right rotated position. I assessed active thoracic rotation in standing (cueing no motion of the pelvis) and palpated the motion the transverse processes relative to the segment above (T5 relative to T4) for the zygapophysial joints and the motion of the rib relative to the transverse process for the costo-transverse joints. The same palpation was used during inhalation, which would have required the left rib to posteriorly rotate (same motion needed to bring the TR to neutral). The findings were that during inhalation and left rotation the left 5th rib was restricted at the costo-transverse joint into inferior glide.
- Diane’s comment:
The palpation you used was to assess the arthrokinematic mobility and while not incorrect, it is usually confined to further assessment of the articular system and we are not there at this point in the evaluation. To further assess active mobility of a thoracic ring, we first need to know what are the requirements of the meaningful task (right HN sideflexion) and based on her improved experience in the task when you corrected the TR5 and returned it to a neutral position, I would suggest what we want to know is whether she could by herself (active mobility) ‘return’ the TR5 to a neutral position as you suggest above “the active mobility test would assess the ability of TR5 rotate to the left to neutral from the right rotated position”. So the test we are looking for here, is to palpate the entire ring as we normally do, ask her to rotate left and see if, with no facilitation, TR5 can actively left rotate to neutral or does it stay in right rotation.
- Mara’s further comment:
I did this full ring palpation during left thoracic rotation and found that the ring moved towards left rotation but did not return to neutral. I then palpated the zygapophysial joints and the costo-transverse joints during thoracic rotation and inhalation with the findings above. I probably did not need to test both motions, but I wanted to confirm my findings.
Passive Mobility
When attempting to correct this ring, distraction was achieved relatively easily but I could not fully de-rotate it, which could have influenced some of the findings of the driver assessment.
- Diane’s comment:
This is the finding that precedes any arthrokinematic active mobility testing.
- Mara’s response:
Chronologically, I did the passive mobility testing feeling the whole ring and trying to correct it before the active mobility testing. I added the note here as it pertains to passive mobility.
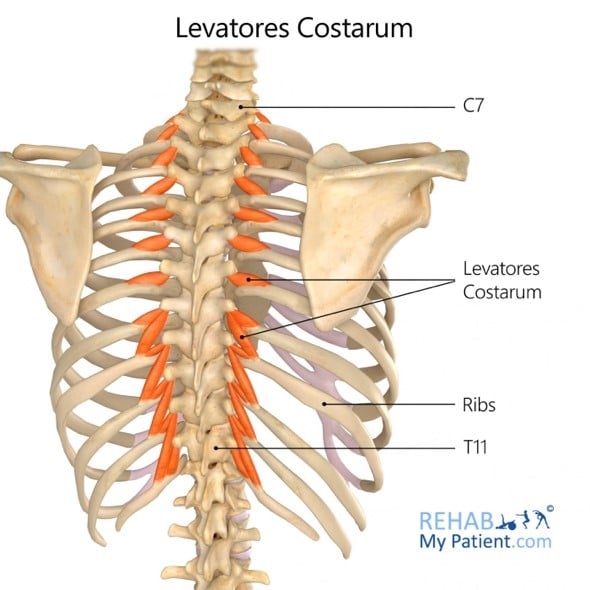
Passive mobility of TR 5 was assessed with a correct, release and listen technique (Passive Listening). The ring was gently distracted bilaterally and a posterior rotation force was applied to the left rib, passive listening of this revealed a short hard vector on the left rib, which I interpreted as an articular system impairment although a partial correction was possible. On release, a short neuromuscular vector was felt on the posterior aspect of the left rib suggesting a short paraspinal muscle (left Levator Costarum) and another on the antero-lateral aspect of the rib pulling laterally, which I palpated as a fascicle of the left Serratus Anterior muscle. To further assess the specific location of the articular vector, I placed the patient prone and assessed the costo-transverse and zygapophysial joints of the thoracic ring 5 and found that the inferior glide of the left rib relative to the left transverse process of T5 was restricted.
- Diane’s comment and question:
OK, let’s back this up a bit and following the dominant listening on release of the corrections for the proper order of treatment. You could only get a partial correction of TR5. Could you correct this ring to neutral? If so, there is enough articular mobility for the task. Does the task require left rotation? Were you trying to correct this ring beyond neutral? So, the amplitude of this partial correction is important – why? How does it dictate whether the articular system was treated first?
Let’s stay with the assumption that you couldn’t get TR5 to correct to neutral. TR5 is right rotated/left translated. What are the arthrokinematic requirements of both the left and right zygapophyseal (T4-5) and costotransverse joints (5th CT joints) for the task given the start position of this ring? How would you use sagittal plane motion to test which arthrokinematics glide to further assess at the T4-5 zygapophyseal joints and how would you use inhalation/exhalation to further assess the 5th CT joints before you tested the arthrokinematics glides at all.
- Mara’s response:
When attempting to correct the TR5, I was able to distract it from TR6 and when I applied a lift under the anterior aspect of the left rib, a partial derotation occurred (estimated to 50% to neutral). With increased lift under the left rib, I was able to obtain slightly more derotation (maybe to 75%) but this was difficult to maintain and with prolonged hold it did not improve (waited and waited). On release of this hold, I was able to feel the neuromuscular vectors described above (Levator Costarum and Serratus Anterior). My interpretation was that the first barrier was neuromuscular and second barrier was articular.
When TR5 is right rotated/left translated and it needs to rotate left and translate right to neutral for the task.
Arthrokinematically the following are needed for this task:
- the left T4/T5 zygapophyseal joint glides inferiorly
- the right T4/T5 zygapophyseal joint glides superiorly
- the left 5th costo-transverse joint glides inferiorly
- the right 5th costotransverse joint glides superiorly
During flexion both the right and the left zygapophyseal joints should glide superiorly while during extension they would glide inferiorly. With inhalation, both costo-transverse joints would glide inferiorly while during exhalation they would glide superiorly.
- Diane’s response & question:
So to clarify, from the passive listening, even though there wasn’t full passive mobility available for the requirements of the task, the short neuromuscular vectors were felt to be stronger than the articular vectors and therefore based on this would be treated before the articular vectors?
- Mara’s response:
I am not sure if “stronger” would be the right term for what I felt.
During the ‘correct’ part I felt that with distraction and a slight lift of the anterior aspect of the left rib, the ring moved to about 50 % of the range from right rotated/left translated position towards neutral. I was able to move it a bit further towards neutral by applying more posterior rotation force to the left rib but this slight increase felt hard to maintain and felt ‘forced’. Further correction was not possible and the resistance to my hand felt articular (short hard vector). On the ‘release and listen’ part I felt the short neuromuscular vector of the Levator Costarum first (like a spring pulling back) then the Serratus Anterior vector pulling the ring into further left translation.
In other words the articular vector was what did not allow for full correction, then on release I was able to feel the neuro-muscular vectors.
Active Control
At this point I did not assess the Active Control of the TR5 as I wanted to first release the articular vector in order to get a more accurate finding. On the second visit, once the vectors were released, she was found to fail at maintaining the TR5 corrected while abducting her arm but with the connect cue in place, the active control of this ring was established. The patient’s presentation did not warrant testing the passive control of this ring as there was not trauma in the history.
Cervical Driver: (C6 priority segment)
Active Mobility
Active Mobility of C6 was assessed during head and neck rotation bilaterally. The starting position of C6 was left rotation/right translation, during left active rotation the segment moved further into left rotation while during right active rotation there was limited right rotation of this segment, about 50% of the expected range.
- Diane’s question:
Is it necessary to test left rotation of the head and neck? Is this in relationship to the requirements of her meaningful task? Is 50% of the expected range of right rotation enough to bring C6 to neutral? Is there an active mobility restriction for this task?
- Mara’s response:
Active left rotation of the neck would not bring any relevant information for the assessment, thank you for noting that. The right rotation; however, would test the ability of this segment to return to neutral and continue further into right rotation/left translation, motions which are coupled with the task of right side flexion. During active right rotation, C6 moved past neutral into about 50% of the expected normal range, so yes, there is an active mobility restriction for the task.
Passive Mobility
Passive Mobility of C6 was tested in supine with the therapist’s hands contacting the transverse processes of this vertebra and it was found that further left rotation was available, as found with active mobility, but the right rotation was restricted with a vector from the posterior aspect on the left side towards upper thoracic (Posterior Scalene) and a secondary vector on the posterior aspect towards upper cervical region.
- Diane’s question:
It is well known that strategies are task specific; therefore the vectors you found in supine may have no relevance to the strategy Ms. CS uses in standing for her work. Why not test passive mobility of the cervical spine like you did TR5? It would have been much more meaningful of an assessment and the vector found relevant to how she organizes her spine in gravity.
- Mara’s response:
Yes, I can understand how changing the position could change her recruitment strategy and my findings during passive mobility testing but I do not have the skills to do this in standing as I never attempted it. Old habits are hard to break and I see how I just assumed that we always test passive mobility in supine for the neck region.
- Diane’s comment:
We did this in sitting in the ISM Series. I think it is important to at least have the neck in its same relationship to gravity.
Active Control
C6 Active Control was tested on the second visit after the vectors on this segment were released and the neutral position was obtained. The left arm lift task was used to determine the ability to control this segment with the increased load of arm motion, it is expected that C6 should maintain its neutral position. I palpated C6 while the patient actively flexed her left arm to 90 degrees and no rotation or translation was noted at the C6.
Passive Control
Passive Control of C6 was not tested as the history did not indicate any past trauma to the area.
Initial Treatment Session
Release
I then proceeded to palpate the left Serratus Anterior and found that the fascicle attaching to the left 5th rib was hypertonic, this neuromuscular vector was released with a “release with awareness” technique where the fascicle was placed in a shortened position by stabilizing the rib with one hand and moving the scapula towards the insertion point, the patient’s attention was brought to the area and asked to soften the muscle under my fingers on each exhalation. Once the tone of the fascicle was felt to decrease, a stretch to this tissue was introduced by moving the scapula away from the attachment on the rib while still stabilizing the 5th rib.
C6 – The same “release with awareness” technique was used for left Posterior Scalene muscle in supine, where the cervical spine was side flexed to the left to shorten the muscle. Then the fascicle from the left transverse process of C6 was palpated while asking the client to soften the area under my fingers, followed by a stretch where the C6 was moved into right side flexion, left translation while stabilizing the muscle attachment on the second rib. After this technique, I reassessed C6 position in supine and sitting and it was neutral, with the C5-C2 region still in right rotation. No further vectors were felt at this time.
Align
On reassessment, C6 did not need an align cue as its position had returned to neutral after the release. TR5 however was still right rotated/left translated in standing but it was easier to correct passively. While holding the corrected position, I asked the patient to try to maintain this by imagining more space between the ribs while the head would float towards the ceiling and she was able to actively maintain the neutral position of the TR5 for one full breath. Passive support from rigid taping could have been useful to maintain the alignment of this ring, but due to time restraints and the fact that she showed good understanding of the self-correction, I decided not to apply it on this visit.
Since her sleep and ability to rest had been impacted, we discussed alignment of the neck and thorax in her preferred right sidelying position, ensuring that the entire cervical spine was well supported on the pillow, with a small rolled towel placed in the pillowcase. Thoracic and pelvis positions were also discussed and I suggested placing another pillow between the knees and the ankles to ensure no rotation would occur. A comfortable position was found for the left upper extremity, with the elbow supported on the side of the trunk and her fist resting on the bed.
Connect
I showed the patient how to palpate the left 5th rib and gently lift it on an inhale, feel it get “sucked in” and line up with the rest (this would indicate the translation would ‘reduce’) then using a suspension cue at T5 (“imagine a fish hook lift this segment just one millimetre”) to try and maintain it for 2-3 slow breaths, and repeated every hour at work or every time she would return to the medical cabinet.
Move
No intervention that used motion was introduced at this point, on the second visit, left shoulder abduction while maintaining ring alignment was used to ensure the repeated task of lifting this arm would not change TR5 alignment. She would still be able to palpate her left 5th rib to check on the alignment of the ring first or if the sensation of heaviness/fatigue would occur.
Home exercise plan
After the first visit, the only home exercise was to correct TR5 and hold the connect cue for 3 slow breaths, to be done every hour at work.
- Diane’s question:
What was the impact on the meaningful task of right sideflexion of the head and neck after the treatment of this initial session?
- Mara’s response:
After the treatment session the patient was able to sideflex the head and neck to the right through normal range with no pain in the neck or towards the shoulder.
Follow Up Treatment
On the second visit, CS reported full resolution of the acute left neck/shoulder pain with a return to the ongoing tension sensation that was generalized to the neck and upper back regions, which she had been experiencing for a long time. She noticed that when standing at the medical cabinet her elbows would have to be lifted to almost shoulder height and maintained there while performing small tasks such as placing pills in small containers. This would cause a sensation of weakness and fatigue in her left shoulder that would exacerbate by the end of the shift, she also mentioned that this sensation was familiar to her and had occurred prior to the acute neck pain episode.
I chose a new meaningful task of left shoulder abduction to 90 degrees and reassessed her FU# 1 and 2 with the following relevant findings:
FU#2
Start screen position: standing
Cranial region: R ICT, left rotated sphenoid, slight right rotation/left translation of C1 and C2
Cervical region: all right rotated/left translated, increasingly more rotation towards lower cervical spine.
TR1 left rotated, TR2 right rotated/left translated.
Shoulder girdle was left rotated, the head of the humerus was centered in the glenoid.
- Diane’s comment:
Start screen changes from initial session of note: C6 is no longer incongruent to the other cervical segments; however, the sphenoid is now incongruent to the ICT (I still doubt the position of C1 to C2 at the AA joint – see comments above in prior session) and TR1 is incongruent to TR2 and C7.
Screening task: left arm abduction to 90 degrees
During the task, the TR1 further left rotated, TR2 remained right rotated, the cervical spine returned to neutral, the left clavicle further posteriorly rotated and scapula had expected amount of upward rotation for the task.
Correcting the TR1 corrected the TR2 and the shoulder girdle position and improved the sensation of weakness for the patient. Correcting the cranium did not change the alignment of the cervical spine or upper thoracic rings, nor did it improve the subjective experience. I chose TR1 as the driver for FU#2.
- Diane’s question:
When correcting the cranium, did you do a co-correction of the incongruent sphenoid and the ICT? Why do you think the sphenoid is suddenly (between one session) rotated incongruent to the ICT – what could have potentially happened to cause this?
- Mara’s response:
When correcting the cranial region, I distracted the cranium off C1, distracted the mastoid processes apart and moved the left temporal bone into posterior rotation while pushing the left sphenoid forward. So yes, I did a full correction of the cranium including the incongruent sphenoid.
As for the position of the sphenoid, it is interesting to note that TR1 has also changed position from right rotated to left rotated between sessions. My hypothesis is that the buccopharyngeal fascia, which attaches to the sphenoid and to the anterior aspect of the upper thoracic vertebral bodies through the anterior longitudinal ligament, could be the structure that induced this change in sphenoid position, as everything else stayed the same in the upper cervical and cranium.
The sphenoid is also an attachment for the dura, see my answer below regarding the possible relationship between the sphenoid and the pelvis.
- Diane’s comment:
I totally agree!! If the buccopharyngeal fascia was the dominant vector, in addition to sphenoid rotation, you may have noticed a sideflexion of the sphenoid (one eye lower).
FU#1
Start screen position: standing
Pelvis R TPR with no unlocking of the sacro-iliac joints bilaterally, left hip anterior to the right.
Lower thorax right rotated.
Middle thorax also right rotated with TR5 most right rotated/left translated.
- Diane’s comment/thought:
Interesting that the sphenoid has changed rotation as has the pelvis, the hips again follow the pelvis and TR5 has remained consistently right rotated in both sessions.
Screening task: left arm abduction to 90 degrees
The pelvis and the hips did not change from the initial position.
The thorax remained right rotated as a whole, TR5 further rotated right/translated to the left.
Correcting TR5 corrected the rest of the thorax and the pelvis and significantly improved the client’s reported fatigue/weakness in the shoulder. She said her arm felt light and strong and she felt she could hold it in abduction “forever”. Based on these findings the TR5 was chosen as the driver for FU#1.
I then assessed the impact of correcting the TR5 on the FU#2 driver – Thorax (TR1). While holding TR5 corrected, TR1 was found in neutral position as well as TR2. This led me to pick the TR5 as the primary driver for the left arm abduction task. I was able to easily correct this thoracic ring so the articular vector released on the first visit was no longer present, which could also explain why I did not get good corrections below in the lower thorax and pelvis on the first assessment.
- Diane’s question:
Do you have a hypothesis as to what is causing the sphenoid to be incongruent to the ICT now and why the pelvis is in a RTPR vs left?
- Mara’s response:
The change in pelvis position between the two sessions, after releasing the articular vectors on TR5, makes me consider the pelvis as an adaptable segment that is able to unwind all of the right rotation found in the thorax. It was interesting to note that the pelvis was not correcting with the Driver correction (thorax, TR5), which makes me believe that the pelvis rotation is more a functional response rather than in inherent impairment. The hips are following the rotation of the pelvis, so they would not be the cause of this change. Although I screened the FU#3 (lower legs and ankles) in the first session and did not note any significant abnormalities, the pelvis could be in relationship to other impairments.
Another way to look at this change is to note that both the sphenoid and the pelvis have changed rotation, bringing the relationship between the two through of the dura system. The cranial dura mater has attachments both to the occiput and the sphenoid as well as the sacrum. Tension or torsion in the dura could cause a relative rotation of these bones.
- Diane’s comment:
A very plausible hypothesis.
The passive mobility tests for TR5 as described above found normal mobility of the segment. Passive mobility was tested and combined with a correct, release and listen technique. As mentioned above, the correction was easily achieved and on release the first motion felt was compression followed by an anterior rotation of the left rib with vectors to left Serratus Anterior and one on the posterior aspect of the left rib going up towards the neck.
These neuro-muscular vectors were released using a release with awareness technique for the serratus anterior and Dry Needling for the longer vector, which I was not able to identify at the time but later assumed it could have been iliocostalis coli, also called iliocostalis cervicis.
Here is where I returned to the active control test for TR5, now with no articular or neuromuscular vectors affecting it. As expected, TR5 remained right rotated/left translated but it no longer went into further rotation during the task of left shoulder abduction. I corrected the TR5 and asked the patient to maintain this position using her connect cue of imagining a fish hook slightly lifting T5, continued to palpate TR5 and applied resistance to her elbow to increase the load for abduction. The ring remained in neutral position and she was able to maintain this for one cycle of breath before failure.
The patient reported that she was able to self correct TR5 and hold it for 3 breaths since the last visit, so I increased her load to include left shoulder abduction and hold for 1-2 breaths if possible.
Home Exercise Program Summary
- Self correction of TR5 with shoulder abduction and hold for 1-2 breaths every hour
- Self correction of TR5 only and hold for 5 breaths (arm by the side) later in the day when above exercise is feels hard or she fails to maintain.
- Self release the left Serratus Anterior, she was able to do this by placing her right hand in her axilla, palpating the tender fascicle, pushing the shoulder blade back with the same hand while the arm was dangling. I asked her to imagine peeling the muscle off the rib and pushing the scapula away without allowing the ring to translate/rotate. She was to do this whenever she felt the ring would not easily correct.
The plan for further visits was to continue to increase load through the left arm, by placing a small 2-3 lbs weight in the hand while holding the arm in abduction at 90 degrees to challenge the control of the TR5 and working more with isometric/sustained positions as this more closely relates to her work position.
Conclusion
Reflecting on the application of ISM principles in this case, I was able to observe my own faulty thought patterns such as biasing the best correction to the area that improved the task subjectively the most and not necessarily the best objective biomechanical correction. On the other hand, the resulting treatment was still effective for the acute phase of the presentation, as well as for identifying the Driver for the more chronic/ongoing presentation and being able to follow up with the appropriate connect cue and progression for exercises that will enable the patient to perform her work tasks without the risk of periodically aggravating her symptoms.
Reflecting back on this case, it seems that the TR5 had the most influence over the other regions, even in two separate meaningful tasks, and its position did not change between the two sessions. In the first visit, with a more “acute neck” presentation, TR5 was only able to partially correct due to presence of articular vectors, and a co-correction of C6 was necessary to improve the task of right side flexion of the neck. For the second visit, with the articular vectors released, it was easier to observe the behaviour of the TR5 in relationship to the other areas and to the meaningful task. This highlights the expected behaviour of a Driver, where other areas (sphenoid, TR1 and pelvis) changed their start position between sessions, adapting to other impairments. Treating the driver resulted in significant improvements both in symptomatology and functional abilities of Ms. CS and she was able to feel and control the TR5 through various tasks afterwards, increasing her self-reliance especially regarding her positioning at work.
- Diane’s final comment:
Great case Mara and great reflection throughout the ISM certification journey!
Skills Demonstration
Please click here to open related document, ISM Clinical Reasoning Reflection Form for Finding Drivers.
Case Study Author
Clinical Mentorship in the Integrated Systems Model
Join Diane, and her team of highly skilled assistants, on this mentorship journey and immerse yourself in a series of education opportunities that will improve your clinical efficacy for treating the whole person using the updated Integrated Systems Model.
We will come together for 3 sessions of 4 (4.5) days over a period of 6-8 months with lots of practical/clinical time to focus on acquiring the skills and clinical reasoning to put the ISM model into practice. Hours of online lecture and reading material and 12 hours of in-person lecture are...
More Info




