Story
Ms. A is a 42-year-old female who presented to Diane Lee & Associates clinic on the 20th of February 2019 with three meaningful complaints. She reported chronic sacral pain, chronic left groin pain and chronic dyspareunia. The reason for presenting to the clinic is that she was 22 weeks pregnant with her first baby at the time and wanted specialized prenatal management of her pain.
Ms. A reported having sacral pain as a teenager, aggravated by lying down or forward bending. She remembered seeking treatment from a massage therapist during her teenage years. She had to quit her job tree planting due to her sacral pain at 22 years old. There was no traumatic injury or episode that initiated her sacral pain. She was still able to run and resume her activities of daily living. At 28 years old (14 years ago) Ms. A had a snowboarding accident, to which she landed on her left hip. The pain and injury stopped her from running and lifting weights due to left hip and groin pain. She was diagnosed with an anterior labral tear of her left hip via MRA 10 years later. Five years ago, at 37 years old, she had an insidious onset of dyspareunia. She did not have any unprovoked vulvodynia. She reported that her current pregnancy had not changed the severity of her complaints.
Diane’s question:
Ms. A has longstanding pelvic pain with no known initiating traumatic event. There is ‘one piece of information’ in this story so far that suggests she has an over-active pelvic floor, associated with under-active deep fibres of multifidus; which given the lack of major trauma, could be driven by habits or her emotional state. What part of the story so far makes me think this?
Kelly's response:
Ms. A’s meaningful tasks of lying down or forward bending at a young age suggest she had under-active deep fibres of multifidus and an over-active pelvic floor. These tasks require good activity & control of deep fibres of multifidus, as well as the ability for the pelvic floor to lengthen to achieve good hip & pelvic movement. Ms. A presented with signs that suggest a link to dural tension from the cranium to the tailbone & pelvic floor.
Diane’s comment:
I totally agree with your response. For more clarity for the readers, the term above “meaningful task” is being used here in a way that we haven’t explained yet. Can you first define what is meant in ISM by a ‘meaningful task’ and then in this story, describe what is biomechanically meaningful about lying down or forward bending that gives further explanation to your answer as to why these tasks, and her nervous system’s response to these tasks, suggest an imbalance of recruitment of the deep sacral fibres of multifidus and her pelvic floor? Go into a bit more of the osteokinematics required in these tasks and how an underactive sacral multifidus and over-active pelvic floor could be implicated.
Kelly’s response:
In the ISM ‘meaningful task’ is a term used to focus assessment in accordance with what is relevant or meaningful to the patient. A task is chosen by both the patient and therapist that is proving to be symptomatic or sub-optimal. Lying down and forward bending were tasks required for rest and work respectively and performed regularly for Ms. A. These two tasks were most symptomatic to the relevant meaningful complaints, hence were chosen to be her meaningful tasks.
In terms of osteokinematics, lying supine requires the ability for the hips to fully extend, while the pelvis may have some anterior tilt or be in a neutral position. Forward bending requires hip flexion and anterior pelvic tilt. The deep sacral fibres of multifidus and pelvic floor are two muscle groups that assist the osteokinematics of both of these tasks. If they are unable to recruit appropriately an imbalance will occur, a sub-optimal strategy will be adopted and this can (but not always) produce pain or symptoms. Some sub-optimal strategies, or strategies in general are not a problem for a patient, however in Ms. A’s case her strategy for these tasks was producing pain, therefore deemed sub-optimal and these imbalances need to be investigated.
Diane’s question:
What position should the sacrum be in relative to the innominates in both forward bending and supine lying for optimal load transfer through the sacroiliac joints? The deep fibres of multifidus and the pelvic floor are antagonists to the position of the sacrum; one position facilitates control, the other does not.
Kelly’s response:
In a straightforward bend the sacrum should remain nutated relative to the innominates as the pelvic girdle anteriorly tilts to allow the movement. The sacrum should also remain nutated relative to both the innominates in a supine lying position. In neither position should the sacum be counternutated relative to the innominates for optimal load transfer to occur. The deep fibres of multifidus facilitate control of the sacrum, whereas the pelvic floor does not. The multifidus assists sacro-iliac joint control in both a forward bend and supine lying.
Diane’s question:
Can you hypothesize on how her hip injury could contribute to the insidious onset of dyspareunia?
Kelly’s response:
A traumatic injury to the hip joint can impair its neuromuscular control, with a change in activation of the stabilizing muscles. This could be reactive, inhibitory or compensatory. The obturator internus muscle, which is a deep hip external rotator and abductor, attaches to the posterior surface of the obturator membrane, surrounds the obturator foramen and inserts on the medial surface of the greater trochanter. When this pelvic floor muscle is in spasm or inhibited, the global neuromuscular control of the hip can change.
Acetabular labral tears have been shown to be associated with overactivity of the pelvic floor, and vice versa (Groh et al., 2009 & Hunt et al., 2007). Ms. A developed dyspareunia long after the traumatic injury, however if her pelvic floor and hip were not addressed it is very possible that the dysfunction increased over time to become symptomatic in sexual function.
Groh, M. M., & Herrera, J. (2009). A comprehensive review of hip labral tears. Current Reviews in Musculoskeletal Medicine, 2(2), 105–117. doi:10.1007/s12178-009-9052-9.
Hunt D, Clohisy J, Prather H. (2007). Acetabular tears of the hip in women. Phys Med Rehabil Clin N Am.,18(3):497–520.
Ms. A had seen different Physiotherapists, massage therapists and kinesiologists in the past to manage her pain conservatively. She chose to avoid surgery for her hip after diagnosis. She would experience temporary relief with treatment to her low back and hip, but the pain in her sacrum and groin would soon return. Strength training was also painful. Ms. A had been with her husband for 8 years, and intercourse was not painful prior to 5 years ago. In the last 5 years she had the ability to have intercourse, but it was extremely painful and would take from hours to days to subside.
Past history included clinical anxiety, headaches & teeth grinding since she was a child. She has allergies to gluten & diary. She takes Ciprolex.
Meaningful Complaints
Ms. A reported three meaningful complaints at the time of initial assessment:
- Sacral pain
- Left sided groin pain
- Dyspareunia
Diane’s question:
What is the difference between a ‘complaint’ and a ‘meaningful complaint’?
Kelly's response:
A meaningful complaint is one that is relevant to the patient’s experience (sensorial, emotional and cognitive) and the reason they are seeking help. It is a complaint that is important for the patient to change or improve, and selected as a focus of assessment.
Diane’s comment:
Absolutely right! It is the sensation they are using to assess “Am I better?”
Cognitive Belief
Ms. A’s belief was that she has a labral tear in her left hip and her pelvic floor is weak. She believes that the tear caused her hips to compensate and along with her prior sacral pain has contributed to tension in her pelvic floor and hence the dyspareunia. She believes there is a relationship between the tightness in her hips and sacrum. She feels pain in both areas when one or the other is particularly painful.
She is very self-aware and tries to continue her daily activities of living, however found herself always ‘guarding her pelvis & hips by gripping the musculature sub-consciously’.
Diane’s question:
Is there anything in her cognitive beliefs that could cause a ‘barrier’ to her recovery? Are there any tests you would include in your assessment regardless of where the driver was to address these cognitive beliefs?
Kelly's response:
Ms. A’s traumatic labral tear was a big moment in her history and she believes much of her symptoms are linked to that event. Although it is likely a big contributor to her dyspreunia and pelvic pain, her symptoms began long before this injury. Finding other drivers may show Ms. A that relief can come from externally to the hip, and therefore the labral tear may not be the entire picture and could be managed conservatively by addressing all drivers. It would also be wise to include orthopaedic hip tests to rule in or out true signs of articular impingement or impairments.
Diane’s followup comment:
If Ms. A’s cognitive belief is that all her symptoms are related to the labral tear (which physio can’t repair) then it will be difficult for her to take control, and improve function, of non-hip impairments that are impacting the performance of this hip and the behavior of the pelvic floor muscles. If the femoral head is found to be levering on the torn labrum when lying supine or in forward bending AND the pelvic floor is found to be over-active, having her feel a difference in the femoral head position and the recruitment activity of her pelvic floor when an ‘external impairment’ (something other than the hip) is corrected could create a huge breakthrough for this cognitive belief. Even if the hip is the primary driver, if correcting the hip can change the behavior of the pelvic floor muscles, this could still dispel her belief that a faulty structure is causing all her symptoms.
Kelly’s comment:
I totally agree with this comment, and Ms. A would almost be in tears of joy when she felt that relief of a hip correction and the pain dissipate! We would comment regularly on how damage to the hip can’t be changed so rapidly if the labral tear is the only cause of pain.
Meaningful Tasks
Ms. A reported 2 meaningful tasks at the time of initial assessment:
- Forward bending
- Lying down (supine)
Screening Tasks
Standing postural screen
A standing postural screen is important to assess as it provides information on the body’s starting position before many tasks, as well as how the body reacts to weight bearing in space. Standing posture was the precursor to Ms. A’s meaningful tasks of a forward bend and moving into supine.
Functional Unit 1 – pelvis, hips & thorax to the 3rd thoracic ring
Pelvis: Rotated left in the transverse plane (TPR) with a congruent left intra-pelvic torsion (IPT).
Diane’s question:
How did you determine that the intra-pelvic position was a torsion versus one, or both, SIJs being ‘unlocked’?
Kelly’s response:
To differentiate an intra-pelvic torsion from an unlocked SIJ, I palpated the ilium with one hand and palpated the sacrum at the inferior lateral angle with the other hand. I asked Ms. A to unload the side I was palpating by having her shift her weight to the contralateral leg. As she came back to neutral standing (50% weight through each leg) no movement between my hands was observed at the SIJ. For both left and right weight transfers the right innominate anteriorly rotated, the left innominate posteriorly rotated and the sacrum rotated left & nutated relative to both innominates. This describes an intra-pelvic torsion, since the relative position of the sacrum to its respective innominate is nutation. If a loss of control of the SIJ is palpated (for example a right unlocked SIJ in standing) the right innominate would anteriorly rotate, the left innominate would posteriorly rotate and the sacrum would rotate left, counternutate on the right and nutate on the left. This did not happen for either the right or left SIJ.
Diane’s question:
What is the relative difference between the position of the sacrum to its ipsilateral innominate in an IPT vs an unlocked SIJ? What is the main ligament under tension in an unlocked SIJ and how would you test if this structure was a source of the pelvic girdle pain in Ms. A?
Kelly’s response:
In an intra-pelvic torsion the sacrum is rotated towards the posteriorly rotated innominate, and nutated relative to both innominates. In an unlocked SIJ the sacrum is counternutated relative to the innominates. In an unlocked SIJ the long dorsal ligament is under tension due to the counternutation of the sacrum relative to the innominates, and can produce pain in the pelvic girdle. Palpation of the long dorsal ligament both with manual nutation and counternutation of the sacrum in prone lying can be performed to test for re-production of symptoms.
Hip: Left hip anterior relative to the left acetabulum, a finding that was incongruent with the positional finding of the entire pelvic ring (left TPR) and the right hip.
Diane’s question:
Where was the left hip in relationship to the right? Without knowing this we cannot determine congruency of the hips to the position of the pelvis. In your answer, can you define one of the two ways we use the word ‘incongruent’ in ISM that is applicable to this finding/statement.
Kelly’s response:
The left hip was anterior relative to the right hip and relative to the left acetabulum. This describes an intra-regional incongruency, in that the left hip is not following the relative direction of the acetabulum nor the optimal position relative to the right hip. The left hip also has an inter-regional incongruency with the pelvis, in that the left hip does not follow the transverse plane rotation and intra-pelvic torsion of the pelvis.
Diane’s follow up response:
You have identified one definition of incongruent in the response above when you say, “the left hip does not follow the [direction of the] transverse plane rotation and intra-pelvic torsion of the pelvis”. This definition speaks to an understanding of optimal biomechanics and what should happen in a task. The second definition of incongruent is about regions moving in the same direction. For example, left transverse plane rotation of the pelvis and left rotation of the 8th thoracic ring would be a congruent finding; whereas, left transverse plane rotation of the pelvis and right rotation of the 8th thoracic ring would be an incongruent finding. Now then, if the task these findings were found in was forward bending, and then BOTH the LTPR of the pelvis and LTPR or RTPR of the 8th thoracic ring would be incongruent with the requirements of this task. One definition pertains to the position of each region (same or opposite) and the second pertains to consistent with requirements of a task, regardless of the position.
Thorax: Upper thorax regionally rotated to the left, 3rd thoracic ring left translated/right rotated, 4th thoracic ring right translated/left rotated. The 3rd and 4th thoracic rings were not glued together.
Diane’s question:
Given that the upper thorax was rotated to the left in general which of the two noted thoracic rings above are you more interested in correcting first and why?
Kelly’s response:
I am interested in correcting the 3rd thoracic ring, as it is both intra-regionally incongruent with the regional rotation of the upper thorax, and inter-regionally incongruent with the pelvis.
Diane’s comment:
There is no right or wrong answer to this question as long as it is clinically reasoned as Kelly has done here. I would have chosen the 4th thoracic ring since it is congruent with the regional rotation of the upper thorax.
Summary of incongruencies in FU#1
The left hip and 3rd thoracic ring are incongruent with the pelvis and regional rotation of the upper thorax.
Functional Unit 2 – 2nd thoracic ring to the cranium
Thorax: Second thoracic ring left translated/right rotated. First thoracic ring right rotated. The rings were not glued together.
Diane’s question:
Can you explain what ‘glued together’ means and why it is important to know this when two adjacent thoracic rings are translated/rotated in opposite directions?
Kelly’s response:
Glued rings describe when two adjacent rings cannot move independently of one another. If two adjacent rings are translated/rotated in opposite directions it is important to address both rings in a correction, where you gently correct one ring, then stop and correct the other, playing the two off of one another to get an optimal correction. It is equally important to assess which may be a priority ring within the glued rings by slowly releasing the correction & assessing which ring returns to its position first and may pull the other ring afterwards.
Shoulder girdle: Rotated left in the transverse plane (TPR) with a congruent manubrium and right humeral head (anterior relative to the glenoid fossa). Right clavicle elevated and anteriorly rotated, congruent with the direction of rotation of the shoulder girdle and incongruent to the rotation of the first 3 thoracic rings.
Neck: The 4th & 3rd cervical vertebrae were left translated/right rotated. The 2nd cervical vertebra was right translated/left rotated.
Cranial: Right intra-cranial torsion (ICT), sphenoid rotated right which was congruent with the ICT.
Summary of congruencies/incongruencies in FU#2
The 2nd & 1st thoracic rings, the 4th and 3rd cervical vertebrae and the cranial region were congruent with one another, but incongruent with the shoulder girdle and the 2nd cervical vertebrae.
Functional Unit 3 – extremities
Feet: Right foot pronated and right hallux abducted from the midline with a large bunion. Left foot neutral, mid foot & hindfoot stacked, no significant findings.
Knees: Right knee positioned in a reverse screw home mechanism in standing.
Diane’s question:
What does the presence of bony changes (bunion) about a joint tell you about the history of loading strategies for this right foot?
Kelly’s response:
A bunion can be an example of an altered centre of mass over the base of support of that foot, causing tissue overload and changes to intrinsic foot muscle function. Sub-optimal strategies from the foot itself or an external driver can lead to these changes. It’s also a sign that the strategy for loading through that particular foot has been occurring for a long time.
Diane’s question:
What is meant by a reverse screw home mechanism in standing? Positionally, where should the tibia be relative to the femur when the knee is extended and where is it for Ms. A.? Are the right foot and knee congruent? How would you determine within this unit whether the pronated right foot was causing the reverse biomechanics for extension at the knee or if the reverse biomechanics were causing the pronation of the foot, or neither was causing each?
Kelly’s response:
The knee joint is a hinge type, uniaxial joint that allows flexion and extension movements. However there is external rotation of the tibia relative to the femur in last 15 degrees of knee extension due to inequality of articular surface of femur condyles. Reverse screw home mechanism refers to a sub optimal finding of the knee in standing, where the tibia may not be externally rotated relative to the femur, or is rotated internally. Ms. A exhibited a reverse screw home mechanism of the right knee in standing, where her tibia did not externally rotate relative to her femur coming into standing from a small squat. Her right knee and foot were congruent, in that the direction of the foot position and tibia relative to the femur were both left rotated in the transverse plane.
To determine if one finding was causing the other in FU#3 (if a standing/weight bearing task was a meaningful task) one must be corrected, then the other checked for improvement. The foot was corrected by lifting the heel off the ground, stacking the talus on the calcaneus then placing it back down. It may be necessary to hold the foot as well if the motor control is poor once stacked. The left foot & rest of the body is ‘reset’ by marching on the spot once on the left foot. Then the right knee was palpated, Ms. A was asked to do a small squat then stand back up. There was no change to the reverse screw home position of the knee. Then the knee was corrected by weight transferring fully onto the left leg, the right tibia manually externally rotated relative to the femur then the leg placed back down to 50% weight bearing, holding the tibia in place. Ms. A was asked to reset again as above, then the right foot was observed and palpated. The right foot did not change. Neither findings were causing the other.
Diane’s follow up comment:
Excellent! But you would only be doing this if standing was your meaningful task, and it isn’t. But you are right – this is exactly how you would do this.
Summary of incongruencies in FU#3
There were no incongruencies in FU#3.
Summary of incongruencies in all 3 functional units
The incongruencies between each unit of most interest were the left hip and the 3rd thoracic ring (right rotated) with the pelvis (left rotated), and the shoulder girdle (left rotated) with the upper thoracic rings/4th & 3rd cervical vertebrae (right rotated) and the right intra-cranial torsion.
Diane’s comment:
For each screening task, the driver will be found in each functional unit first, the drivers of each unit will be played off one another to determine the region for priority for treatment. The relevant incongruencies will then become clear.
Forward bend
One leg standing was chosen because stance phase is a necessary component of running stride. It allows for weight acceptance and prepares the runner for push off. The right side was chosen over the left because the patient’s symptoms were more obvious and irritable on the right side. Non-optimal alignment, biomechanics and/or control can occur throughout the three functional units of the body during one leg standing and this is identified by observing and palpating body regions during this task.
A forward bend is a vital task for many daily activities such as picking up children or objects, reaching, tying shoelaces and more. In a forward bend (in the sagittal plane) the pelvis should not rotate in the transverse plane, the SIJs should remain in a controlled position, and the hips should not translate relative to the other side or the relative acetabulum. There should be optimal alignment/biomechanics/control of the thorax, neck, cranium and lower extremities. The rings of the thorax should not translate/rotate, but should anteriorly rotate to fold forward. The vertebrae of the cervical spine will typically move into flexion. The cranium should not rotate regionally or intra-cranially if looking straight down and not rotating the head or neck. The extremities remain steady with 50% weight bearing in each leg, knees in extension.
Functional Unit 1 – pelvis, hips & thorax to the 3rd thoracic ring
Pelvis: Rotated further in a left TPR, left sacroiliac joint (SIJ) unlocked early into task.
Hip: Left hip translated further anterior relative to the left acetabulum, a finding that was incongruent with the positional finding of the pelvis (left TPR).
Thorax: Upper thorax regionally rotated to the left remained the same, 3rd thoracic ring left translated/right rotated, 4th thoracic ring right translated/left rotated remained the same.
Driver in Functional Unit 1: Primary driver – left hip
Explanation: Left hip correction reduced pain, improved task & corrected the pelvis & thorax. Correcting the pelvis and the 3rd thoracic ring did not change the position of the left hip, nor changed Ms. A’s symptoms.
Diane’s question:
In ISM, finding drivers helps us to understand multiple sites of impairment in patients with complex stories and persistent pain (like Ms. A.). Can you explain further, as if talking to someone not familiar with the principles of ISM, what the following means in the context of the forward bending task:
Kelly’s response:
- Hip correction: centering the left femoral head into the acetabulum manually
- Improved task: the activity of question becomes easier, or symptoms are reduced, or both
- Corrected the pelvis: the rotation of the pelvis is corrected manually to a neutral position, and may require gentle compression with the hands as well
- Corrected the thorax: the thoracic ring is manually lifted off of the thoracic ring below, then rotated in the opposite direction to where it is found.
Functional Unit 2 – 2nd thoracic ring to the cranium
Thorax: Second thoracic ring left translated/right rotated worsened. First thoracic ring (right rotated) worsened.
Shoulder girdle: Rotated left in the transverse plane (TPR) with a congruent manubrium and right humeral head (anterior relative to the glenoid fossa) remained the same. Right clavicle elevated and anteriorly rotated (congruent with the shoulder girdle), remained the same.
Neck: The 4th & 3rd cervical vertebrae left translated/right rotated remained the same. The 2nd cervical vertebrae right translated/left rotated further.
Cranial: Increased right intra-cranial torsion (ICT), sphenoid rotated right.
Driver in Functional Unit 2: Primary driver cranial region (cranium)
Explanation: Correcting the cranium corrected the 2nd, 1st thoracic rings and the 2nd cervical vertebrae and reduced pain in sacrum and left groin.
Diane’s question:
For clarity, did correcting the cranium completely correct the other sites of impairment in FU#2?
Kelly’s response:
The cranium did completely correct the other sites of impairment in FU#2.
Functional Unit 3 – extremities
Feet: Right foot pronated further, left foot did not change.
Knees: Right knee remained the same in a reverse screw home mechanism.
Driver in Functional Unit 3: no drivers found
Explanation: No corrections successful and did not improve the task, correcting the foot or knee aggravated symptoms
Diane’s question:
Maybe I am assuming too much; however, am I correct in that correcting the lateral rotation of the calcaneus relative to the talus, dorsiflexing/abducting the talus relative to the calcaneus and supinating the mid and forefoot while abducting the first hallux (the foot correction), did NOT change the position of the tibia relative to the femur (undo the reverse screw home mechanism)? Also, an attempt to correct the tibia relative to the femur did not improve the alignment of the hindfoot or forefoot?
Kelly’s response:
Correcting the right foot (correcting the lateral rotation of the calcaneus relative to the talus, dorsiflexing/abducting the talus relative to the calcaneus and supinating the mid and forefoot while abducting the first hallux) did not change the position of the tibia relative to the femur, nor did correcting the right tibia relative to the femur did not improve the alignment of the right hindfoot or forefoot. I was also very suspicious of this, hence tried the correction several times to confirm the finding. Each correction only aggravated Ms. A further!
Overall driver for forward bend: Primary driver left hip, secondary driver cranial
Explanation: Correcting the left hip partially corrected the cranium, relieved sacral & left groin pain the most and improved the task. Correcting the cranium did not correct the hip, however relieved sacral & left groin pain further.
Diane’s comment:
Perfect reasoning for your choice of drivers!
Diane’s question:
In ISM, we use the terms primary, secondary and co for drivers. Here you have determined there is a primary hip, secondary hip. Can you briefly explain the definitions of each:
- Primary driver – The region of the body that when ‘corrected’ improves both the patient’s experience of the task as well as performance of other sites of impairment the most.
- Secondary driver – The region of the body that when ‘corrected’ also improves both the patient’s experience of the task as well as performance of other sites of impairment. It is; however, not as successful as the primary driver, but important to also correct in addition to the primary driver to gain even further improvement of performance of the task. Correction of the secondary driver does not improve the primary driver.
- Co-driver – type 1 – The regions of the body that when ‘corrected’ improves both the patient’s experience of the task as well as performance of other sites of impairment. It also corrects the other driver completely.
- Co-driver – type 2 – The regions of the body that both need to be ‘corrected’ together to improve both the patient’s experience of the task as well as performance of other sites of impairment. Correcting only one of the drivers will not improve the task.
Supine
Lying supine is necessary for rest and relaxation, as well as working tasks for some (e.g. plumber or car mechanic). The inability to lie supine without pain can be quite distressful and disrupt sleep patterns. The pelvis should not be unlocked, and good alignment should exist between the cranium and the pelvis.
Functional Unit 1 – pelvis, hips & thorax to the 3rd thoracic ring
Pelvis: Rotated further in a left TPR, left SIJ unlocked.
Diane’s question:
How did you determine that the left SIJ was unlocked in supine lying vs in an IPT?
Kelly’s response:
An unlocked SIJ was determined by palpating both the ASIS and the sacrum while supine. Ms. A was asked to lift her hips up to allow hand placement under the sacrum before lying back down. The right ASIS was elevated relative to the left ASIS. The sacrum was rotated left, towards the left innominate (ipsilateral side); however, it was nutated on the right side and counternutated on the left side. This describes an unlocked left SIJ. The sacrum is more difficult to palpate in supine and multiple checks were made to determine this.
Diane’s question:
The form and force closure mechanisms (Vleeming & Snijders 1990) work together to prevent shear between the sacrum and innominate at the SIJ. Lying supine is one of the most difficult positions for individuals with pelvic control issues to tolerate because ‘unlocking’ reduces the self-locking mechanism as described by Vleeming & Snijders. What is this self-locking mechanism, which ligaments are tensed when the SIJ is ‘locked’ and which ligament is under more load when the SIJ is ‘unlocked’? Which muscles would likely become overactive when the pelvis is ‘unlocked’? How does this information fit with findings so far from Ms. A’s story and driver findings?
Kelly’s response:
The word sacrum originates from the mid 18th century: from Latin os sacrum, translation of Greek hieron osteon ‘sacred bone’ (from the belief that the soul resides in it, another reason for women’s health Physiotherapists to believe the pelvis is the centre of the universe! Haha).
The sacro-iliac joint (SIJ) is a synovial diarthrodial joint with a high level of stability from the self-locking mechanisms of the pelvis, which comes from the anatomy and shape of the bones (form closure) and the muscles supporting the pelvis (force closure).
Form closure describes the stability of the joint from the design of the pelvic anatomy. The flat and ridged surfaces of the joint interlock together, promoting stability. The symmetrical grooves and ridges allow the highest coefficient of friction of any diarthrodial joint and protect the joint against shearing. The position of the bones creates a ‘keystone’ shape, which adds to the stability in the pelvic ring. Nutation and counternutation movements occur at the SIJ.
Force closure describes the other forces acting across the joint to create stability. Structures with a fibre direction perpendicular to the sacroiliac joint help to create force, and is adjustable according to the loading situation. Muscles, ligaments and the thoracolumbar facia all contribute to force closure.
(Vleeming et al., 1990, Willard et al., 2012).
Tension of the sacro-tuberous, sacro-spinous and iliolumbar ligaments are responsible for ‘locking’ the SIJ. An ‘unlocked’ SIJ puts the long dorsal ligament under more load relative to the other ligaments, as the sacrum is counternutated on the ipsilateral side of the SIJ relative to the ipsilateral innominate.
Muscles that may become overactive to support an‘unlocked’ SIJ may be the hamstrings, pelvic floor, piriformis, multifidus, transverse abdominis, obliques, iliocostalis, longissimus and the gluteals. Ms. A exhibited signs of pelvic floor and hamstring overactivity, in that she reported dyspareunia, trouble relaxing her pelvic floor and tightness in the hamstrings forward bending.
Vleeming A, Stoeckart R, Volkers, ACW, Snijders CJ. Relation between form and function in the sacroiliac joint. Part 1: Clinical anatomical aspects. Spine 1990a; 15(2): 130-132
Willard F.H, Vleeming A, Schuenke M.D, Danneels L & Schleip R. The thoracolumbar fascia: anatomy, function and clinical considerations. Journal of Anatomy 2012; 221(6): 507-36
Diane’s response:
Awesome answer and explanation!
Hip: Left hip translated further anterior relative to the left acetabulum early into hip extension (~40 degrees hip flexion), incongruent with the positional finding of the pelvis (left TPR).
Diane’s question:
When we find the hip incongruent to the TPR of the pelvis, it often indicates that there are two vectors, one rotating the pelvis and another translating the hip. You now have a very consistent finding of incongruence of the hip and pelvis across every task tested so far. Using your pattern recognition from multiple patients you have treated with dyspareunia; does this pattern of consistent incongruence of the hip to the pelvis suggest any particular system impairment or finding to you?
Kelly’s response:
The consistency of the findings for Ms. A and pattern recognition of previous patients suggest that impairments exist in the myofascial and neural systems. It is common clinically to see pelvic floor overactivity or tone and neural dural tension in patients with hip pain or dyspareunia. Pelvic floor overactivity or tone can cause impaired alignment/biomechanics/control of the hip and pelvis as it has direct insertions into both regions and can pull between the two.
Thorax: Upper thorax regionally rotated to the left remained the same, 3rd thoracic ring left translated/right rotated, 4th thoracic ring right translated/left rotated remained the same.
Driver in Functional Unit 1: Primary driver left hip
Explanation: Hip correction reduced pain, improved task & corrected the pelvis & thorax.
Diane’s question:
In supine, when the hip position is corrected the pelvis and thorax cannot immediately adapt to this correction because of gravity and body weight on the table. Did you ask the patient to do anything while the hip was corrected that then facilitated the correction of the TPR of the pelvis and thorax? How did you know that the left hip correction, restored the self-locking mechanism of the left SIJ (part of the required pelvic correction), in other words how did you hold the hip correction and test the control of the left SIJ?
Kelly’s response:
Once the left hip was corrected in crook-lying Ms. A was then asked to lift her hips off the bed into a small bridge, then lower back down into supine as a way to ‘reset’ while maintaining the correction. Once supine was achieved one hand held the left hip correction while the other palpated both the pelvis and the thorax. Palpation of the SIJ was achieved by sliding one hand under Ms. A’s pelvis to reach the sacrum. The sacrum was still rotated left, towards the left innominate (ipsilateral side), however it was nutated on both sides relative to the innominates, in other words ‘locked’. Ms. A was demonstrating a left TPR and a left IPT, rather than an ‘unlocked’ left SIJ.
Functional Unit 2 – 2nd thoracic ring to the cranium
Thorax: Second thoracic ring left translated/right rotated. First thoracic ring right rotated. The rings were not glued together.
Shoulder girdle: Rotated left in the transverse plane (TPR) with a congruent manubrium and right humeral head (anterior relative to the glenoid fossa) remained the same. Right clavicle elevated and anteriorly rotated (congruent with the shoulder girdle), remained the same.
Neck: The 4th & 3rd cervical vertebrae left translated/right rotated remained the same. The 2nd cervical vertebrae right translated/left rotated further.
Cranial: Increased right intra-cranial torsion (ICT), sphenoid congruent.
Driver in Functional Unit 2: Primary driver cranial region (cranium)
Explanation: Correcting the cranium corrected the 2nd cervical vertebrae, reduced pain in sacrum and left groin.
Diane’s question:
And by their absence, do we assume that correcting the cranium totally corrected the alignment of C3, C4, shoulder girdle, right clavicle, 2nd and 1st thoracic rings? This is the requirement of a primary driver.
Kelly’s response:
Yes, correcting the cranium did correct C3, C4, shoulder girdle, right clavicle, 2nd & 1st thoracic rings.
Functional Unit 3 – extremities
Feet: Non-weight bearing in the task, no significant position of the feet that was sub-optimal
Knees: no findings, normal screw home mechanism in supine
Diane’s question:
When the cranium is a driver, it is critical to consider the impact of any cranial torsion on mobility of the dura, and by its extension the perineural structures all the way to the feet. Sub-optimal dural/neural mobility can impact the position of the feet when lying supine (they tend to invert when there is adverse neural tension at the tarsal tunnel). From your findings here, are you saying that the feet were in neutral alignment – was there still a noted hallux valgus – did the right knee biomechanics in extension now revert to normal as opposed to still being in a reverse screw home position? If so, this suggests that the feet and knees are in relationship to something that appears in standing and disappears in supine and so far everything above the knees has remained consistent in all tasks i.e. nothing has changed. This makes the feet suddenly very interesting.
Revisit the findings of the feet and knees and supine just to be sure what you have written is correct.
Kelly’s response:
On revisiting the findings, the right foot was inverted slightly relative to the left foot, and a hallux valgus of the right foot was still present. The knee no longer had a reverse screw home mechanism, and was externally rotated relative to the femur. This may suggest a neural dural system impairment extending to the right foot.
Diane’s response:
Cool heh! The feet can influence things even when not loaded, but here the findings in standing were in relationship to more proximal drivers.
Driver in Functional Unit 3: no drivers found
No corrections improved the task, improved load transfer in other regions or reduced symptoms
OVERALL DRIVER FOR SUPINE: Primary driver left hip, secondary driver cranial region
Explanation: Correcting the left hip at 40 degrees hip flexion then extending to supine partially corrected the cranium, relieved sacral & left groin pain the most and improved the task. Correcting the cranium didn’t correct the hip, however relieved sacral & left groin pain further.
Screening Tasks Summary
Findings from the above screening tasks help guide further assessment and treatment. The purpose of identifying a driver is to prioritize management and sessions efficiently, as well as find the source of the meaningful complaint, and the relationship between impairments when there are many. Ms. A exhibited a case of a primary driver and a secondary driver. A primary driver correction improves both the patient’s experience of the task as well as performance of all other sites of impairment. The secondary driver does not completely improve all other sites of impairment, but may partially improve them; however, correction of the secondary driver further improves the task and patient’s experience.
Analysis of Ms. A’s drivers in her tasks showed:
- Forward bend: primary driver – left hip; secondary driver – cranium
- Supine: primary driver – left hip; secondary driver – cranium
Further Analysis of the Drivers
Further analysis of the drivers was completed to determine the underlying system impairment(s) that were contributing to Ms. A’s sub-optimal strategies for that task.
Assessment of the hip and cranium included active control & mobility tests, as well as passive control & mobility tests. Passive listening (feeling for restrictive vectors) during all tests helped to determine the underlying system impairment(s).
Further Assessment of the Left Hip
Active control: Poor, left hip translated anteriorly at 50% weight bearing in standing, unable to seat hip independently
Active mobility: Restricted by muscle spasm particularly in hip flexion and internal rotation
Diane’s question:
Which of Ms A’s meaningful tasks would this finding be relevant for, standing forward bend or supine lying? Above, in the supine lying task you also noted the following: “Left hip translated further anterior relative to the left acetabulum early into hip extension (~40 degrees hip flexion), incongruent with the positional finding of the pelvis (left TPR)”, so I would suggest that her active mobility into extension is also sub-optimal.
Kelly’s response:
Forward bending would be the most relevant task for the finding of poor active mobility in hip flexion. Ms. A’s active mobility into extension was also sub-optimal in both standing and supine.
Passive control: Passive resistance around the anterior capsule of the hip joint was noted on correction, ligaments were intact and therefore passive control was intact.
Passive mobility: Positive (painful/reproduces symptoms) ‘Flexion, Adduction, Internal Rotation’ (FADIR) test & Thomas test. She had hypermobility of both hips, however the left hip was painful, the right hip was non-painful.
Passive listening #1 – correcting the driver
The left hip was corrected in 40 degrees hip flexion, where anterior translation began. The hip felt difficult to correct, in that there were long and short vectors translating the hip anteriorly, resisting correction.
Passive listening #2 – releasing the correction
On releasing the correction, vectors were felt in the following order; short adductors, psoas, vastus lateralis and obturator internus & externus as part of the neural system, where both tightness & tone were apparent. Relaxation could occur with cueing but there was underlying tone still present particularly in the pelvic floor (obturator internus). There was then a short, firm & deep anterior vector that felt articular.
Diane’s question:
It is no surprise that there is an underlying deep articular system impairment here other than her MRI findings of a labral tear. Why?
Kelly’s response:
The anterior labral tear in the left hip would predispose Ms. A of ongoing shearing and inflammation of the anterior capsule & acetabulum. As a result scar tissue may occur and restrict the movement of the articular joint.
In summary, the left hip showed underlying impairments of the neural system including the anterior dynamic hip stabilisers (adductor magnus, pectineus, obturator internus & externus, vastus lateralis and psoas). There was also impairment of the articular system, being that there was an existing anterior labral tear and potential scar tissue and fibrosis surrounding the tear. Disuse of the hip in fear of pain over the years had caused a significant weakness of the myofascial system around the hip and sacrum.
Further Assessment of the Cranial Region
Active control: No change was noted to the cranium from initial assessment when load was applied (e.g. during a forward bend).
Active mobility: During a forward bend with head & neck flexion the cranium remained in a right ICT with a congruent sphenoid. Head & neck flexion appeared to occur mostly in the lower cervical region, where the upper cervical region seemed restricted in flexion.
Passive control: No findings – all joints between the cranium, atlas and axis were stable to tests for passive control
Passive mobility: Cranium – Restricted right occipitomastoid suture, difficult to distract temporal bone from occiput. Slow correction from posterior rotation to neutral could be achieved. The sphenoid did not need to be corrected, as it was congruent with the ICT.
Passive Listening #1 – correcting the right ICT of the cranium
Correcting the cranium was initially difficult due to a strong pull but successful. A long & strong postero-inferior pull from the right temporal bone to the lower spine or sacrum was felt. There was a dural pull on the sacrum and left hip when the cranium was corrected. This could be felt by asking an assistant to correct the cranium while the lead therapist palpated the sacrum.
Passive listening #2 – releasing the correction
Once corrected and released the left hip translated anteriorly first, then the cranium followed into a right ICT. Ms. A was able to palpate the left hip and announce when the hip began to translate. The vector again felt like a long strong dural vector. To test this theory Ms. A was asked to contract her pelvic floor muscles, and this increased the dural pull on the right temporal bone.
In Summary
The cranium appeared to have a strong dural vector influencing the groin and sacral pain, an impairment of the neural system. There were also short less dominant neural vectors; the right rectus capitis posterior major and obliquus capitis inferior.
Hypothesis
Ms. A was experiencing symptoms likely emanating from the dura and neural systems as a teenager and into her 20’s. Her teeth grinding, clinical anxiety and headaches were associated with these signs, therefore an upregulated nervous system and dural pull down to her sacrum existed. Over time the neural dural symptoms, upregulated nervous system and myofascial tension may have created congestion in Batson’s plexus. Batson’s plexus was first described by Oscar Vivian Batson in the 1940’s as a system of valveless veins (part of the cerebrospinal venous system) connecting pelvic veins and thoracic veins to the internal vertebral venous plexuses (Nathoo et al., 2011). Congestion in this system can result in neural dural tension/congestion between the pelvis/hip and the cranium, which can be felt as a long strong vector between the two and produce a variety of symptoms such as pain. Compression or congestion of nerves from venous congestion can also produce myofascial pain.
Ms. A was able to adapt to these signs and find appropriate strategies until her snowboarding accident at 28 years old. The anterior labral tear she sustained created a disuse and fear avoidance pattern of the left hip and leg, while guarding through the pelvis over 10 years caused her to develop groin pain, sacral pain and dyspareunia most recently.
To date Ms. A has seen a lot of different therapists, however no one has identified the apparent cranial and dural influence on her symptoms. She hasn’t been given release and align treatment immediately followed by appropriate connect cues and movement strategy re-training pertaining to both her hip and cranium together. Ms. A needed release of the vectors first, then staged re-training and loading of both drivers to return to optimal strategies for her meaningful tasks.
Nathoo N, Caris EC, Wiener JA, Mendel E. History of the vertebral venous plexus and the significant contributions of Breschet and Batson. (2011) Neurosurgery. 69 (5): 1007-14; discussion 1014.
Initial Treatment Session
Treatment in ISM is guided by the acronym ‘RACM’; release, align, connect and move. This framework allows for well-rounded management of the driver(s) to achieve optimal alignment, biomechanics and control in the meaningful tasks.
Release
Primary driver (left hip) – release with awareness in order of presentation in passive listening #2; left adductor magnus, psoas, vastus lateralis and obturator externus. Hip traction in a postero-lateral direction with a Mulligan belt was performed for articular vector release.
Secondary driver (cranial) – Dural release by correcting cranium in crook-lye, then Ms. A completing apical & lateral costal breaths. This was then progressed to dural release down to the pelvic floor with pelvic tucks and pelvic floor contractions. This was followed by release with awareness of the right rectus capitis posterior major and obliquus capitis inferior.
Align
Crook-lying (supine with legs straight was too painful unaided), hip in 40 degrees flexion, cranium neutral relative to the neck on a pillow.
Align cue given for the primary driver left hip was to “ imagine your femoral head in your hip melting like butter down into its socket, down to the bed”.
Align cue for the secondary driver cranium was to “let your right and left ears grow wide out to the sides like dumbo the elephant, relax your jaw, let your head rest in neutral position”.
Connect
Connect cues were given to Ms. A to visualise hip stabiliser co-activation. Her cue was to “draw your left hip ball into its socket gently”.
Move
Pelvic tucks with self cranial correction and lateral costal & apical breaths were performed to provide drainage of Batson’s plexus, reduce dural congestion from the cranial region to the pelvis and to gently move the pelvis relative to the left hip. Once this was achieved Ms. A moved onto dural sliding by tucking the pelvis while extending the cranium and then reversing, maintaining the corrections.
Home Exercise Program
- Massage ball release of the left adductor magnus, psoas, vastus lateralis, obturator externus and ischiococcygeus
- Foam rolling of the left vastus lateralis and vastus medialis oblique muscles
- Self align cues to centre the left femoral head and cranium in crook-lying
- Three sets of 15 pelvic tucks with breaths in crook-lying while maintaining the connect cues given in session per day
Followup treatment sessions
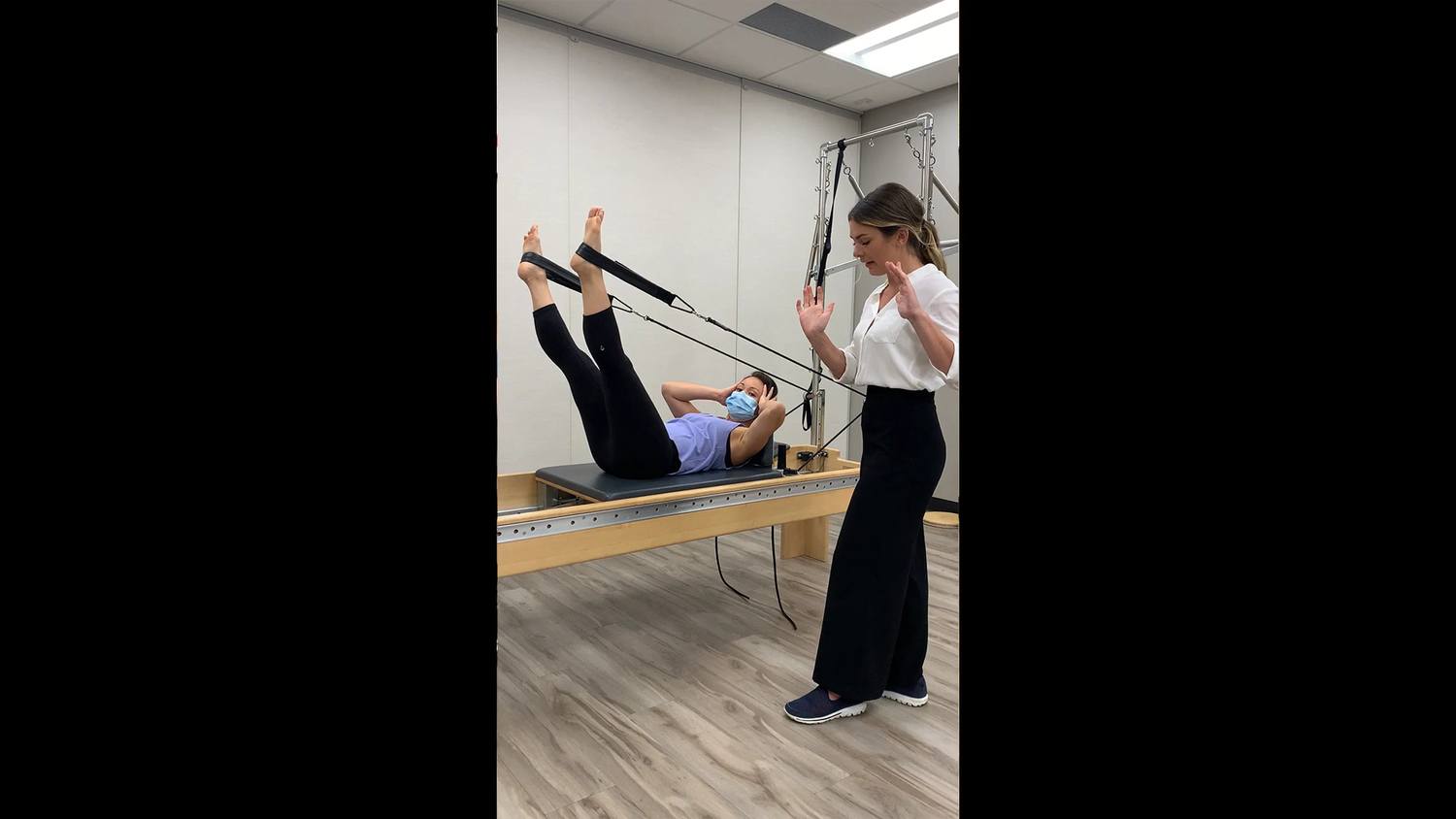
Follow up treatment sessions were focused on progressing Ms. A’s motor control & strategy re-training in the clinic’s Pilates studio. Self release, align & connect cues had significantly improved. Alignment and biomechanics of the primary and secondary drivers had also improved, changing the sensorial experience. However, difficulty still existed in the meaningful tasks to maintain good control. Below describes examples of Ms. A’s movement training to build the motor control capacity of the left hip and cranium.
For motor training there are 3 stages; stage 1, stage 2 and stage 3. There are 3 levels in stage 3.
Stage 1
The ability to produce independent contraction of deep segmental muscles responsible for control of that region, without over-activation of superficial muscles.
Ms. A’s training – Connect cue isometric holds for the left hip in crook-lye, progressing to hip extension then in standing. Cue was to ‘melt the butter’ to allow the hip to centre. Cue for the cranial region was a release cue, ‘imagine your ears are growing wide apart, especially the right ear lobe’.
Stage 2
Strategy capacity training in tasks that have meaning; add load and co-ordinated movement of distal regions while maintaining static position/alignment of region being re-trained.
Ms. A’s training – Reformer tabletop arm series. Maintaining alignment & control of the left hip and cranium but moving the arms against resistance.
Stage 3
Level 1 – Add controlled movement of region being trained in multiple planes.
Ms. A’s training – Reformer leg circles in straps for the left hip. Then static holds mid-air of the legs and a curl up of the head & neck for the cranium. Ms. A had to hold the cranium self corrected for curl ups.
Level 2 – Move the targeted region with either static control or controlled movement of another region.
Ms. A’s training – Reformer side-lying hip abductions with left leg in strap. Static control (against gravity) of the cranium and dynamic control of the left hip are required. Both congruent and incongruent movements of the two drivers needed to be performed.
Level 3 – Progress training to higher equilibrium challenges or unpredictable situations.
Ms. A’s training – Reformer hip & knee extensions + head and neck curl up on footbar in supine. This challenges a higher equilibrium of both the left hip and the cranium together to practice both supine position and a modified forward bend against resistance.
In Summary
Once stage 3 level 3 motor control was achieved Ms. A then progressed to strength training in weight bearing positions, and meaningful task positions. The motor control training began in late 2019, as Ms. A gave birth to her baby boy mid year and needed to be cleared to return to exercise. Interestingly, third trimester pregnancy had improved Ms. A’s meaningful complaints, but they returned postpartum until motor control training could begin. Postpartum stage 3 and beyond training positions involved forward bending (e.g. deadlifts, hip hinges, rotational reaches with load) and supine (e.g. toe taps/heel drags, scissor lifts).
Ms. A is still having ongoing sessions infrequently for maintenance and home exercise progressions, but is actively part of fitness groups where she can successfully do strength and conditioning movements without aggravating her left hip or cranium. Due to the lengthy nature of Ms. A’s story and progress it is predicted that she’ll require ongoing support/maintenance for 1-2 years. Then as she moves through different life stages (future pregnancies, peri-menopause, post-menopause) she’ll experience occasions where she may need more guidance or her meaningful tasks/meaningful complaints may change.
Diane’s comment:
Excellent report Kelly.
Skills Demonstration
Please turn up your volume.
Case Study Author
Clinical Mentorship in the Integrated Systems Model
Join Diane, and her team of highly skilled assistants, on this mentorship journey and immerse yourself in a series of education opportunities that will improve your clinical efficacy for treating the whole person using the updated Integrated Systems Model.
We will come together for 3 sessions of 4 (4.5) days over a period of 6-8 months with lots of practical/clinical time to focus on acquiring the skills and clinical reasoning to put the ISM model into practice. Hours of online lecture and reading material and 12 hours of in-person lecture are...
More Info