Story
Mrs. D is a 44-year-old female, who was referred to the clinic in October 2023 for a pelvic floor assessment to determine the relationship to her right hip and pelvic girdle pain. The story of her right hip meaningful complaint first began 11 years prior after Mrs. D’s description of a traumatic delivery. She described participating in 5 hours of pushing, followed by a failure to progress and having to push the head of the baby back internally to then have the delivery transitioned to an emergency cesarian section. After returning home from her delivery, she described an experience where the muscles around her hip seized up and she was unable to weight bear, or trust, her right leg for a few days. This same event recurred a few days later, with the same pattern, her hip feeling locked into flexion and external rotation followed by a release and feeling of extreme fatigue. Over the last 11 years, Mrs. D reports a similar experience occurring a total of 5 times.
- Diane’s question:
Does Mrs. D experience any right hip or pelvic girdle pain (PGP) in between these episodes, or does the pain resolve completely?
- Kate’s response:
The pain resolves completely between the episodes when she is more sedentary and working a desk job. When she started to increase her activity by participating in Zumba classes and skating, her pain does not completely resolve and lingers between activity. The length of duration often being in relationship to the volume of loading and rest time between.
Mrs. D has worked a desk job until May of 2023, when she decided she was looking for a change and transitioned to coaching ice skating for various ages and skill levels. Mrs. D was previously a competitive figure skater, but had been out of the sport for many years prior to returning to work. To prepare and increase her fitness for skating, she began to participate in Zumba classes and soon after began to notice the onset of right lateral hip discomfort over her greater trochanter while lying in bed. This discomfort started to expand into the Zumba classes where she became aware of soreness and pinching sensation when the hip was moved into internal and external rotation. Because of her prior pain experience with the hip, she discontinued the Zumba due to the fear of provoking her previous hip spasms.
Currently, Mrs. D has transitioned to full time teaching on the ice which requires her to be there six days a week, for 1-3 hour shifts, 1-2 times per day. Mrs. D began to see a Physiotherapist in May to address her hip symptoms from the Zumba and also because they were starting to occur in some of the skating patterns that she was required to teach. Specifically, she noticed with internal and external rotation forces through the hip such as a C-Curve skate move or double skull which requires internal and external rotation of both hips simultaneously. She also reported pelvic floor symptoms of stress urinary incontinence during some of the jumping exercises and occasional heaviness.
- Diane’s question:
Tell me more about the timeline of her stress urinary incontinence (SUI). For example, how long did it take her to regain her continence (or did she) after her pregnancy 11 years ago? Are these symptoms new, intermittent, old etc.?
- Kate’s response:
She reported that her SUI did not occur during or after pregnancy. The onset of SUI was 5 years after her delivery where she started to notice it with coughing and sneezing. With the increased activity through participation in Zumba classes she would notice it with jumping and when she tripped or stumbled unexpectedly during dance moves. Then with the skating, she primarily reported noticing it while jumping. This could suggest that she has not been able to optimize load transfer strategies post-partum which could potentially lead to SUI overtime. It could also indicate that her pelvic floor is compensating for a remote area which may impact its ability to provide optimal support for the bladder.
- Diane’s comment:
Very plausible hypotheses, let’s circle back to this later in the report to see if either of these are valid.
At prior physiotherapy, Mrs. D reported that she received local assessment and treatment of her right hip. Her past treatment plan initially consisted of release work for hip mobility which she reported worsened her experience and symptoms. It was then transitioned to strengthening of hip musculature. After 5 months of weekly treatment, she reported being told that there might be something “inside the hip, stopping it from moving” or “maybe it is pelvic floor related” which then led to the referral to Diane Lee & Associates physiotherapy. It also contributed to new cognitive beliefs.
- Diane’s question:
When local treatment makes symptoms worse, what does this tell you from an ISM perspective?
- Kate’s response:
From an ISM perspective, when local treatment makes the symptom worse it often indicates that you are not working on the primary driver and are potentially treating the area of the body that is compensating or is the victim to the primary driver. A painful region of the body is not enough information to guide local treatment as it does not provide insight into why it hurts or what region of the body should be treated, which is where ISM comes in. In this case, there is a possibility that the increased tone in the hip musculature, which is potentially impacting her mobility, is reacting to a variety of different mechanisms in the body and releasing these muscles to improve her mobility might take away her current strategy of adapting to the drivers or being able to manage load.
- Diane’s response:
Absolutely right!
Past Medical History
Mrs. D has sustained the following injuries in her past:
- Left upper neck injury while bagging heavy groceries in university and reports I persistent reduced cervical range of motion and left sided tension.
- Fall while skating October 2022 in which she sustained a tailbone impact and a concussion.
- Multiple knee contusions while falling in skating.
- Right ankle eversion sprain while stopping with her right hip and foot in external rotation. Required treatment with an air cast and physiotherapy rehabilitation.
- 1 trial of labour followed by a cesarian section. No formal pelvic floor or physiotherapy rehabilitation following. Experience of stress urinary incontinence with jumping on skates.
Mrs. D is healthy and does not have any other previous medical concerns.
- Diane’s question:
Through the lens of ISM, describe a mechanism by which the following injuries could individually, and collectively, contribute to her hip and potential pelvic floor impairment. Following each description, outline how you would identify if one, or any, of these required consideration in her treatment plan.
- The upper neck injury
- The concussion
- The sacrococcygeal joint injury
- The right ankle eversion sprain
1. Upper neck injury
The upper neck is related to the pelvic floor and hip through fascial connections. The neck is supported and surrounded by the deep cervical fascia which can be divided into superficial, middle and deep laminae. The deep laminae, also referred to as the prevertebral layer, surrounds the cervical vertebrae and encompasses the longus coli, longus capituus, scalenes, longissimus, semispinalis and deep multifidus. Anteriorly the deep laminae becomes continuous with the anterior longitudinal ligament of the spine and posteriorly with the nuchal ligament. The anterior longitudinal ligament runs the entire length of the anterior vertebral bodies to the anterior surface of the sacrum where it blends into the anterior sacrococcygeal ligament. The anterior sacrococcygeal ligament serves as an attachment point for the levator ani. It also is in relationship to other pelvic floor muscles such as the piriformis and obturator internus through fascial and muscular connections which also link to the hip. An injury to the upper neck can alter the function of the cervical vertebrae and the muscles attached. This can result in a vector of pull in the deep cervical fascia, and because of the continuous fascial network can have distal impacts on the pelvic floor and hip by altering tension.
Screening head and neck rotation is a test that can be used to consider if the upper neck injury needs further assessment. If correcting the FU #1 driver worsens head and neck rotation then this indicates that further assessment of FU #2 should be completed.
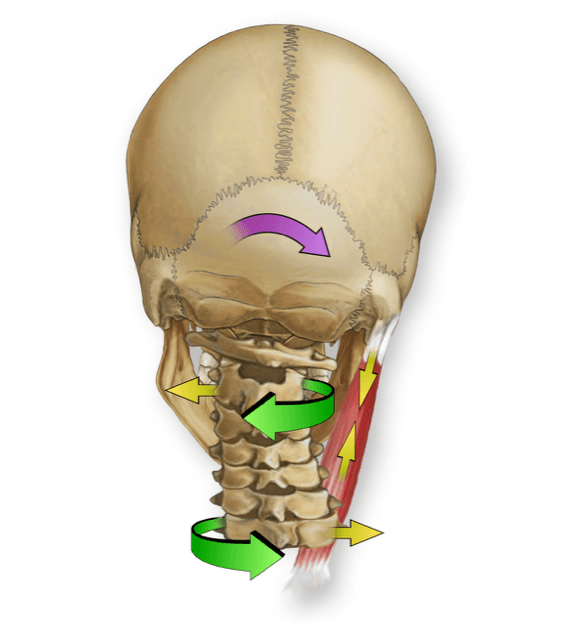
2. Concussion
A concussion has the potential to impact mobility of the cranial sutures which will have multiple impacts. Firstly, lack of mobility in the sutures asymmetrically can place the cranium into an intra-cranial torsion (ICT) which can lead to compression of the OA joint and therefore impact the spinal dura attached to the OA membrane. This could result in a pelvic floor muscle contraction as a reaction which further increases tension on the dural system.
Secondly, lack of mobility of these sutures can impair the primary respiratory mechanism of the cranium. This mechanism is important for the movement of fluid (CSF, venous blood and glymph) through the cranial sinuses. An ICT could impact the drainage of the fluid surrounding the brain causing further back up into the cranial sinus system. Increased congestion can create increased tension in the spinal dura via the backflow into the valveless venous system (Baston’s plexus) of the spine. If the pelvic floor is contracted as a reaction, this can alter the length tension relationship of the muscles of the pelvic floor and therefore their function.
To determine the relationship between the dura and pelvic floor, the patient can start in a hook lie position. A correction can be applied to the ICT and they can contract their pelvic floor. If the spinal dura is not able to elongate, a caudal pull will be felt on the cranium. If there is an asymmetric contraction in the pelvic floor, this may result in the cranium being pulled into an ICT. This can also be extended to assess for the positions required for skating. The cranium can be corrected and the lower extremity can be moved into positions that tension the posterior, middle and anterior extensions of the dura to determine if there is a caudal pull or impaired ability of the dura system to elongate.
- Diane’s comment:
Nice modification of the test Kate! One could also do the test without the cranium corrected first and then assess the impact of the correction. In other words if the correction worsens the dural mobility, then the twist is to offload the dural tension. If the correction of the cranium improves the dural mobility, then the dura is a victim of something else twisting the cranium (suture, any muscle or fascial system attaching to the cranium etc.)
3. Sacrococcygeal joint injury
A sacrococcygeal joint injury can result in inflammation and potentially adhesions around both the joint and the dural system. The dural system continues past the conus medullaris and fuses into the filum terminale which anchors the dural system to the coccyx inferiorly. The previous injury has the potential to create restrictions in dural movement, which will impact the resting tone of the pelvic floor as it may contract and increase tension into the dural system.
This will alter how the pelvic floor is able to function if it is functioning as a reactor to the dural tension. Additionally, if the mobility of this joint is restricted it will alter the length tension function of the pelvic floor muscles that attach to it.
Mobility of the joint could be screened by palpating the coccyx during a pelvic floor contraction. The coccyx should flex when the pelvic floor contracts. If there is an articular restriction then a contraction of the pelvic floor may not result in movement of the joint. If the sacrococcygeal joint is held in flexion due to pelvic floor reaction, then this may alter the movement at the joint.
- Diane’s question:
How would you expect the hip or pelvic floor to change if these two impairments were in relationship?
- Kate’s response:
If the impairment was articular then altering the dural tension or correcting the ICT would not change the pelvic floor. If the impairment was related to dural mobility, correcting the ICT may improve the mobility felt in the sacrococcygeal joint during a pelvic floor contraction.
4. Right ankle eversion sprain
An eversion ankle sprain, which would stretch the medial structures such as the deltoid ligament and tibial nerve, can also impact the pelvic floor. Firstly, if the alignment, biomechanics and motor control are not improved after the injury has healed, there could be altered ankle mobility, alignment and loading strategies. For example, a lateral talar tilt could occur due to reduced form closure in the medial ligaments which could result in lengthening of the medial side of the foot as the talus moves anterior and medial if there is not enough force closure. This would send an ascending internal rotation force up the lower extremity and place the pelvis into a transverse plane rotation, creating asymmetrical muscle tension and recruitment of the pelvic floor muscles. Additionally, if the talar tilt places excessive tension into the tibial nerve this can alter the dural mobility. The foot may shorten into a sickle c shape to offload the nerve and potentially result in more loading on the lateral column of the foot. This position would send an ascending external rotation force to the pelvis creating asymmetrical tension into the hip and pelvic floor. Altered foot alignment, biomechanics and control can have ascending impacts up to the pelvis and hip influencing alignment, biomechanics and also motor control.
A squat can be used to screen the relationship between the ankle sprain and pelvic floor and hip function. Similar to cervical head and neck rotation, a squat can be used to screen the relationship. After finding the driver for FU#1, which changed pelvic and hip function, checking the impact of the driver on the ankle into a squat would determine if further assessment of the foot and ankle would be required. If the alignment, biomechanics or control of the foot was negatively impacted with correction of the FU#1 driver, the foot/ankle would require further assessment.
- Diane’s comment:
Well explained and reasoned! There are many potential contributors to her pelvic floor function and right hip pain.
Meaningful Complaint
Mrs. D reported the following meaningful complaints at the time of assessment:
- Right hip pain – location described as internal (intersection point between the sacral inferior lateral angle and the centre of the groin). Includes symptoms of pinching, locking and “threats of spasm”
- Right pelvic girdle pain: tailbone, sacroiliac joint; Can extend into the lumbosacral junction
- Right hip weakness, fatigue and feeling of instability while skating.
- Diane’s question:
In 1994, Joseph Fortin reported on the specific location of pain referred from the sacroiliac joint. Can nociception from the sacroiliac joint cause pain in the lumbosacral junction? What is the clinical significance of your answer?
- Kate’s response:
No, pain that is nociceptive from the sacroiliac joint results in pelvic girdle pain which was demonstrated to refer over the posterior SIJ and with mapped referral patterns showing pain symptoms into the posterolateral buttock/thigh and into the groin. The SIJ does not cause lumbosacral junction pain through a nociceptive referral. However, the lumbosacral junction can have symptoms as a result of compensatory patterns and altered alignment, biomechanics and control that may occur in response to the nociceptive pattern from the SIJ. This is clinically significant as the lumbo-sacral junction is likely another region of meaningful complaint that is separate to the pelvic girdle pain. It is also a region of the body that is potentially a victim of the driver, which demonstrates the importance of the ISM approach because the location of the pain does not determine the why behind the nociceptive source and location.
The meaningful complaints are primarily aggravated by sitting with legs crossed (externally rotated) for a prolonged period. Also, hip internal and external rotation during various skating drills. Specifically, she noticed in skating C-Cut drills, backwards skating, and reaching down to draw on the ice were most provocative. There is an element of a dosage response as increased time sitting with legs crossed worsened response and more time spent on the ice in provocative drills would result in discomfort extending into the next few days before settling down again.
- Diane’s question:
With respect to the phenotype of this hip/PGP, how would you classify it and why?
- Kate’s response:
The pain classification includes elements of nociceptive, neuropathic and nociplastic pain. The primary pain classification would be nociceptive. Nociceptive pain occurs due to ongoing nociceptive input, and in this case, she has clear aggravating factors related to mechanical loading (skating, Zumba, hip external and internal rotation) and has a loading response in which her pain worsens with increased loading and requires rest to recover. There is also underlying elements of neuropathic pain as she can experience muscle weakness, instability and muscle spasms that might occur due to movements and postures that impact the health of the nerve through tensioning or compression. Lastly, there is nociplastic elements which occur when the nervous system becomes sensitized and nociceptive signalling will occur in the absence of actual injury or threat and can be associated with stress, anxiety and negative emotions. The length of time that Mrs. D has been experiencing hip symptoms extends beyond the timelines for tissue healing and she has also developed fears and stress related to the potential consequences of the symptoms. This has the potential to alter and impact the neural signalling and create sensitization in the system. Emotional states do play a role in function and can impact the musculoskeletal system, for example altered muscle activity that can become hypertonic and increase the force closure and compression in the lumbopelvic hip complex.
Cognitive and or Emotional Beliefs
Mrs. D had a few cognitive and emotional beliefs tied to her meaningful complaints:
- Muscles around the hip were squeezing and causing pain and reduced mobility.
- Muscles around the hip were weak causing instability and the belief that the hip would eventually give out while skating.
- Emotional feeling of lack of trust in her body’s ability to demonstrate movements at work and fear that her previous hip spasms would return. She highlighted worrying about the potential repercussions for her new job if her hip prevented her from coaching.
- Unresolved hip and pelvic floor injury from her pregnancy and delivery. This was further developed by her current physiotherapist who discussed the potential role that the pelvic floor could be playing in symptoms.
Often, in an initial assessment for someone with Mrs. D’s meaningful complaint, I would first start with an ISM assessment as she has already had local hip assessment and treatment. A local assessment of the pelvic floor would also be beneficial following her whole-body assessment to address her cognitive and emotional beliefs related to the pelvic floor and her current presentation. The pelvic floor assessment would be done at a different session.
Ultimately, the goal is to integrate the findings of her pelvic floor assessment with those of the whole body (ISM assessment) in relationship to her meaningful tasks. Additionally, as past experience and beliefs also play a large role in what motor control strategy is being chosen and there is a threat perception with her job being on the line if her symptoms persist or worsen, it is important to address her beliefs (Hodges et al., 2013). All of this must be assessed over multiple sessions to address her cognitive beliefs and threat perception.
- Diane’s question:
When a patient has a cognitive belief that their SIJ is unstable, we use a form closure (passive integrity) test to validate or negate this belief. What test would do the same for her belief that her right hip was unstable and clarify if this ‘instability’ was due to a motor control/muscle deficit vs an articular injury?
- Kate’s response:
The passive integrity of the hip’s form closure could be assessed. As each joint has a closed-pack position where there is maximum congruence of the articular surfaces and tension in the major ligaments this is where the articular system can be assessed further.
The hip close pack position is in extension with abduction and internal rotation (Hewitt 2002). The hip can be taken into a closed packed position, often assessed in prone, taking the hip into end range extension and internal rotation and assess the hip’s ability to remain centred and apply an anterosuperior glide to the joint. In this position, with maximum congruency there should be no translation of the femoral head. This can also be combined with other compression tests at the hip to test the labrum through FABER/FADDIR scour test. These tests could help to validate or negate the articular injury.
Meaningful Task
Mrs. D’s meaningful task was a unilateral C-cut skating drill. See below for description and pictures which break the meaningful task down into three positions (How to Ice Skate Backward, n.d).
Picture 1: C-cut Drill
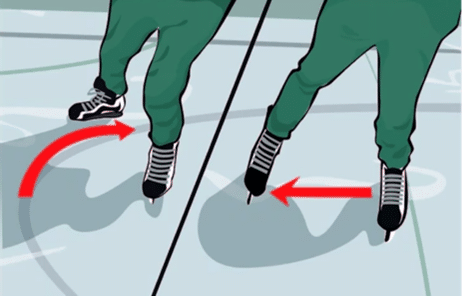
This picture demonstrates the arc of motion required for the right hip in a unilateral C-cut.
Picture 2: Position 1
This picture demonstrates position 1 of the task. The right hip is required to be in internal rotation and flexion.
Picture 3: Position 2
This picture demonstrates position 2 of the task. The right hip is required to move from internal rotation towards a neutral rotation position and into hip abduction.
Picture 4: Position 3
This picture demonstrates position 3 of the task. The right hip moves into external rotation and extension.
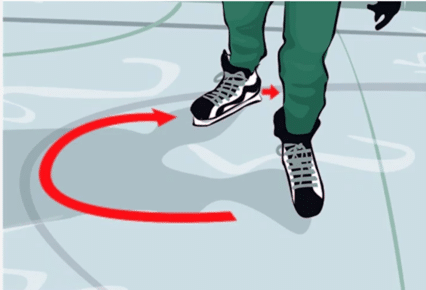
Picture 5: Position 2->3
This picture demonstrates the arc of motion between position 2 and 3 where the majority of Mrs. D’s meaningful complaints occur.
- Diane’s question:
Can you take the biomechanical requirements for this task higher up the kinetic chain and for each position describe the osteokinematic requirements for the pelvis, the thorax (lower and middle), the cervical and upper thorax and potentially the upper neck and cranium? This will allow us later to consider the impact of her pelvis, upper neck and cranial injuries on the whole-body performance of this task and not just the right hip.
- Kate’s response:
Position 1
Pelvis: L TPR IPT
Right Hip: Flexion and internal rotation.
Thorax (Lower): Left TPR, congruent with the pelvis.
Thorax (Middle/Upper): Left TPR, congruent with the lower thorax & pelvis.
Shoulder Girdles: Left TPR relative to the upper thorax. (The shoulder girdles are rotated further in the left transverse plane relative to the upper thorax, and both are left rotated relative to the pelvis).
Cervical & Cranial: Ascending right rotation to bring the head to neutral in the transverse plane as to place gaze forwards.
Ideally, the cervical segments (including the atlanto-axial joint) should de-rotate the LTPR of the pelvis, thorax such that the cranium is neutral and stacked on the atlas at the OA joint. Given the quantity of LTPR to unwind, it is not likely that many could achieve this unwinding without involvement of the AA joint.
Position 2
Pelvis: No transverse plane rotation.
Right Hip: Abduction with no rotation.
Thorax (Lower): No transverse plane rotation, congruent with the pelvis.
Thorax (middle/upper): Middle thorax left TPR relative to the lower thorax. Upper thorax left TPR congruent with the middle thorax.
Shoulder Girdles: Left TPR relative to the upper thorax. (The shoulder girdles are rotated further in the left transverse plane relative to the upper thorax, and both are left rotated relative to the pelvis).
Cervical & Cranium: Cervical segments transition into right rotation relative with minimal torsion of the cranium.
Position 3
Pelvis: Right TPR IPT
Right hip: End range extension and external rotation.
Thorax (lower): Right TPR relative to the coronal plane of the body. Left TPR relative to the pelvis.
Thorax (middle/upper): Left TPR relative to the lower thorax. The upper thorax is rotated further left in the transverse plane relative to the middle thorax.
Shoulders: Left TPR congruent to the upper thorax.
Cervical Spine: Lower cervical spine left TPR congruent to the upper thorax. Upper cervical spine right TPR relative to the lower cervical spine.
Cranial Region: No cranial torsion as the cervical spine should unwind lower rotations to bring the eyes forward.
Screening Tasks
- Standing start screen
- The right C-cut task was split into 3 screening tasks which are labeled below as Position 1, 2 and 3.
Functional Unit #1 (FU#1)
Start Screen: Standing
This is assessed first to determine the starting position (alignment) for each region before assessing their alignment/biomechanics into the C-Cut drill. It is important to assess the meaningful task in relationship to a screening task to be able to determine the relationship between where a body region starts and how it moves through the task. This is also how incongruences can be determined in relationship to both the start screen and the task.
- Diane’s comment and question:
Let’s break this down a bit. Sometimes a full meaningful task, such as the C-Cut drill, cannot be properly examined in its entirety so in ISM, we choose screening tasks that are relevant to that meaningful task – such as your choice of Position 1, 2 or 3. Then, we choose a start screen position (standing in this situation) and assess the performance of those body regions (or segments within a body region) which are starting incongruent to the requirements of the screening task (Position 1, 2, or 3 in this situation). In ISM, we use the term incongruent in two ways, what are they, and for your screening task chosen, which type of incongruence will be the most important going forward in your assessment?
- Kate’s response:
In ISM, incongruent is a way to understand the relationships between rotations within and between regions of the body. For example, if thoracic ring 4 is in a right transverse plane rotation and thoracic ring 5 is in a left transverse plane rotation they would be called incongruent as they are rotating in opposite directions of each other. A congruent finding would be those that rotate in the same direction. Incongruency can also be pertaining to the rotations of the regions of the body in relationship to the requirements of the task. For example, if the task requires the pelvis to move into a right transverse plane rotation and the pelvis moves into a left transverse plane rotation instead, this rotation is incongruent to the osteokinematics required for optimal performance of the task. This is the type of incongruency that will be most important going forwards in the assessment. This is because a task can often require that regions of the body rotate incongruent to each other in order to be congruent with the rotations required of the task. For example, if the task requires the pelvis to rotate in a right transverse plane and requires thoracic ring 5 to rotate left in the transverse plane, these findings would be considered congruent with the task, despite these two regions being incongruent to each other.
- Diane’s response:
Well, described Kate!
Standing start screen findings:
Pelvis:
Left transverse plane rotation (TPR) with a congruent left intra-pelvic torsion (IPT). This is congruent to the task requirements for position 1 of the screening task.
Hips:
Right hip anterior to the left hip. No anterior shear of the right femoral head relative to the right acetabulum. The right hip is congruent to the left TPR of the pelvis. In a left TPR IPT the right hip is expected to be anterior to the left. This is congruent to the task requirements for position 1 of the screening task.
Thorax:
4th thoracic ring translated left and rotated right in the transverse plane.
5th thoracic ring translated right and rotated left in the transverse plane.
8th thoracic ring translated right and rotated left in the transverse plane.
9th thoracic ring translated left and rotated right in the transverse plane.
Thoracic rings 4 and 9 are both in a right transverse plane rotation. They are congruent to each other, but incongruent to thoracic rings 5 and 8. Thoracic rings 4 and 9 are also incongruent to the left transverse plane rotation of the pelvis.
In position 1 of the task thoracic rings 4, 5, 8, 9 should all be in a left transverse plane rotation, and therefore thoracic rings 4 and 9 are the rings of interest as they are incongruent to the pelvis, other thoracic rings and are also incongruent to the requirements of position 1 of the screening task.
Lumbar spine:
Neutral lordosis observed. L4 and L5 were rotated left in the transverse plane. L4 and L5 are congruent to the pelvis in the starting screen.
Summary of incongruencies:
In the standing start screen, the pelvis, hips and thoracic rings 5 & 8 start congruent with the requirements of position 1 of the screening task. Thoracic rings 4 & 9 start incongruent to all the other regions and also incongruent to the requirements of position 1 of the screening task and their biomechanics during the first part of the screening task will be significant to note.
Screening task findings – C-cut drill position 1/2/3:
Pelvis:
- Left TPR with a congruent left IPT which is optimal for position 1 of the task.
- Left TPR and right SIJ unlocked at position 2 which is suboptimal for the task. The pelvis is expected to move towards a neutral rotation and maintain control with no SIJ unlocking.
- Left TPR and right SIJ unlocked. This is also suboptimal for the task as the pelvis should move into a right transverse plane rotation and a congruent IPT.
Right hip:
- Right hip is starting in a flexed and internally rotated position. In this position the right hip is anterior to the left which is congruent with the rotation of the pelvis and the task.
- The right hip is in an abducted and neutral rotation position. In this position the right hip is anterior to the left. This is incongruent to the task as the pelvis should be neutral with no rotation and therefore the right and left hip should both be aligned. The hip is following the pelvis which makes it incongruent to position 2.
- The right hip moves into external rotation and extension. During this movement the right hip remained anterior to the left and sheared anterior relative to the acetabulum. The right hip is also incongruent to the task between position 2 and 3 where it shears anterior relative to the acetabulum which indicates a loss of control. Additionally, as the pelvis should be moving into a right transverse plane rotation, the left hip should become anterior to the right to be congruent with the requirements of the task.
Thorax: 1/2/3:
Thoracic ring 4 moves more into left translation right rotation. Thoracic ring 5 moves further into right translation left rotation. Thoracic rings 8 and 9 remain the same. Thoracic rings 4, 5, 8, 9 should all be moving into further ascending left rotation as the skater moves through the arc of motion of position 1/2/3. As thoracic rings 4 and 9 both start in right rotation and remain right rotated through the task, they are incongruent to all 3 positions of the screening task. Interestingly these two rings are incongruent to the rest of functional unit 1 and are also incongruent to the requirements of the task, which highlights why they are the priority rings to be considering.
- Diane’s comment:
Yes! And that is why we focus on the body regions that in the start screen begin in a position incongruent to the requirements of the task!
Lumbar spine: L5 was L rotated following the pelvis, the change in rotation between the incongruent pelvis and low thorax occurred gradually in the high lumbar/TL junction.
Lumbar spine: 1/2/3:
L4 and L5 remain in a left TPR. After position 1 this becomes an incongruent finding in relationship to the task as L4 & L5 should follow the pelvis as it unwinds out of the L TPR and gradually moves into a R TPR.
Summary of Incongruencies:
The regional incongruencies will be noted if the findings are incongruent to the task.
The pelvis is incongruent to the task at position 2 and 3 because there is loss of control at the right SIJ and because the pelvis should be moving out of a left TPR/IPT into a right TPR with a congruent right IPT.
The right hip is also incongruent to the task at position 2 and 3 where it shears anterior relative to the acetabulum. Additionally, as the pelvis should be moving into a right transverse plane rotation, the left hip should become anterior to the right to be congruent with the requirements of the task.
Thoracic rings 4 and 9 are incongruent to the task in position 1, 2 and 3.
L4 & L5 are also incongruent to the task in position 2 and 3. The pelvis, hips, lumbar spine and thoracic rings 4 and 9 are incongruent to the requirements of the task.
Driver for functional unit 1
Primary Driver
Thorax (Priority rings: TR4 & 5; Secondary rings: TR8 & 9)
Clinical reasoning: Thoracic rings 4 and 5 were glued (incapable of independent motion), as were thoracic rings 8 and 9. Neither were unglued prior to completing the correction (next time I would unglue the rings prior to correcting them to be better able to determine the relationship between the thoracic rings and the other regions of the body). Thoracic rings 4 and 5 were chosen as the priority rings as they partially corrected thoracic rings 8 and 9, whereas correcting 8 and 9 had no impact on thoracic rings 4 and 5. Thoracic rings 4 and 5 correction also resulted in a partial correction of the pelvis by improving motor control since the right SIJ unlocked later towards position 3. Correcting TR4 and 5 partially corrected the right hip as it sheared anterior in the acetabulum later into the task (~ 90% of the movement). This correction also resulted in the best experience of the task, with a report of feeling less discomfort and smoother movement.
Secondary Drivers
Pelvis and right hip
Clinical reasoning: The pelvis is a secondary driver as it was only partially corrected by the primary driver because it remains in a left TPR and still loses control at the end of the task. A correction of the pelvis also fully corrected the position of the hip in position 2 and partially corrected the hip into position 3 as it sheared anterior later in the task. It also resulted in an improved experience of the task, but did not impact the thorax. The right hip is also deemed as a secondary driver, which I believe to be secondary in relation to the 3rd position of the task as the thorax and the pelvis both fully correct it until the very end range of the task where it then becomes a partial correction as the hip shears anterior. Correcting the hip did not improve any other region of the body and worsened experience.
- Diane’s comment:
Well-reasoned. What is the purpose in ISM of determining drivers that are primary vs secondary?
- Kate’s response:
It is important to determine if drivers are primary or secondary as this will determine their treatment priority. Drivers indicate the best place in the body to start treatment. A primary driver indicates that it is the priority region to begin treatment as it will improve or correct other regions of the body. If there was only a primary driver then this would be the only region that needed treatment. The secondary drivers are then treated after the primary driver has been addressed.
Functional Unit #2 (FU#2) Findings
This unit was chosen as part of the assessment for two reasons. Firstly, Mrs. D has indications from her story that there may be potential contributions from unit #2 as she has a prior neck injury and a recent concussion. Secondly, when head and neck rotation was screened with the FU#1 primary driver corrected, Mrs. D’s experience of right head and neck rotation worsened.
Start Screen : Standing
Cranial (Cranium, OA, AA):
Left intracranial torsion (ICT) with a congruent left rotated sphenoid. C1 in a left TPR.
Cervical spine:
C2 translated left, rotated right. C7 translated right, rotated left
- Diane’s question:
So, it appears that the atlas is following the cranium (LICT left rotated atlas) and C2 is incongruent in space to the atlas. Consider the OA, AA and C2-3 joints. Given the described osteokinematics, and knowing that pure transverse plane rotation doesn’t occur at either the OA or the C2-3 joint, hypothesize on the conjunct rotations that should have occurred at the OA, AA and C2-3 joints in this situation.
- Kate’s response:
At the OA joint, rotation occurs with conjunct contralateral side flexion. If the occiput is in left rotation relative to the atlas (OA joints) this would occur with conjunct right-side flexion of the occiput. C2-3 is rotated right relative to the cranium and atlas, which couples ipsilaterally with right side flexion. The AA joint will rotate with conjunct side flexion that can be ipsilateral or contralateral. As both the joints above and below (OA, C2-3) would have conjunct right side-flexion, I would hypothesize that the AA joint might move into a conjunct right-side flexion with its rotation.
- Diane’s comment:
What would be the benefit of MORE right sideflexion at the AA joint? I hypothesize that the occiput is left rotated/right sideflexed on the atlas, the C2-3 is right rotated/right sideflexed/left translated on C3 and the atlas is left rotated in space but right rotated relative to the occiput and left rotated relative to C2 (to unwind the conjunct rotations at the OA and C2-3 joints.) Furthermore, I hypothesize that the atlas is left sideflexed relative to the axis to compensate for the conjunct right sideflexion at the OA and right sideflexion at the C2-3. This is only true if the head is neutral in the transverse and coronal planes.
- Kate’s Response:
So, it would behave more of a sandwich like in the thoracic rings. I was just thinking that the side flexion above at the OA joint and below at C2/3 would create a net vector that would influence the AA joint. But it would make sense that it would try to unwind to bring the head into a more neutral position to unwind the rotations.
- Diane’s response:
IF the head appears to be stacked over the neck then the right sideflexion at the OA joints and C2-3 have to be compensated for somewhere and to me, it makes sense that the AA joint unwinds this.
Shoulder Girdles:
Shoulder girdles in a left TPR (congruent with the upper thorax). Both scapulae were resting in slight upward rotation and bilaterally, the head of humerus was centred in the glenoid.
Thorax (TR1 & 2):
Thoracic ring 1 was in a left transverse plane rotation. Thoracic ring 2 was translated right and rotated left in the transverse plane.
Summary of incongruencies:
C2 is in a right TPR which makes it incongruent to the cranium and C1 which are all left rotated. C7 is congruent to the cranium and C1, but incongruent to C2. The shoulder girdles, TR 1 and TR 2 are all in a left TPR which makes them also congruent to the cranium, C1 and C7, but incongruent to C2. Therefore, C2 is incongruent to all other findings in functional unit 2.
- Diane’s question:
Reflecting on the requirements of Position 1 of the C-Cut drill task, which region(s)/segments in FU#2 are incongruent to the requirements of the first part of this screening task. Hint: It isn’t C2.
- Kate’s response:
The cranium and C1 are incongruent to the requirements of Position 1 of the screening task. Although C2 is incongruent to other parts of functional Unit 2 it is congruent to the requirements of the task.
- Diane’s comment:
Exactly! Therefore, my focus when assessing the biomechanics of this unit in the screening task (position 1) will be everything starting incongruent to the requirements of the task, not C2.
Screening task findings – C-cut drill position 1/2/3
Cranial (Cranium, OA, AA):
1/2/3 the cranium remains in a left ICT, congruent left sphenoid rotation. C1 also remains in a left TPR.
Cervical Spine:
Positions 1/2/3 C2 remains in a right transverse plane rotation.
Position 1 C7 remains in a left transverse plane rotation.
Position 2-3 C7 worsens further into right translation and left rotation.
- Diane’s question:
Reflecting again on what you have written for the biomechanics of all 3 positions of this task with respect to the upper thorax, neck and cranium, the increasing of C7 is described as being a requirement of this part of the task; therefore, is it actually ‘worsening’ or doing what it should do? Which region is NOT doing what you described it should do?
- Kate’s response:
C7 is doing what it should do, and therefore its movement is not worsening. It is moving further into right translation and left rotation which is the required biomechanics of the task. The cranial region remains in the starting position, which is incongruent to the requirements of the task.
- Diane’s comment:
This is a key point in this complex case report. What happens in the task, and which segments are doing things incongruent to the requirements of the task, take priority over start screen incongruences when finding drivers for the task and NOT merely the start screen position.
Thorax: both TR1 and TR2 were right rotated.
Shoulder Girdle:
Position 1/2/3: Shoulders remain in a left TPR. The left glenohumeral joint moves into extension, abduction and horizontal abduction and the right moves into flexion and slight horizontal abduction. These positions are the required arm positions for the task. The scapula are both able to remain upward rotated and the head of the humerus centred in the glenoid.
2-3: the left clavicle compressed medially
Thorax (TR1 & 2):
1/2/3: thoracic ring 1 and 2 both increased into further left rotation in the transverse plane.
- Diane’s question:
Are TR1 & 2 moving optimally or suboptimally for the task as you described above? In ISM we use HODA-A (hands on data acquisition and analysis (Dr. Jo Abbott)) to find and analyze if those findings are optimal or not. Because something ‘rotates further’ how do we interpret this finding accurately?
- Kate’s response:
TR1 and TR2 are moving optimally for the task. They should both progress further into left rotation as the C-cut movement progresses through range.
HODA-A describes the mechanism when a practitioner of manual therapy actively touches a person to obtain information about their musculoskeletal system. We use sensory receptors to provide information to our nervous system to be interpreted. The finding moving further into left rotation can be interpreted in relationship to the finding of left rotation which I palpated in the standing start screen. In ISM we do a starting screen, in this case it is standing, in which baseline starting positions for each region is determined. This allows the movement of each region to be compared to the position it started in. If the starting position is not considered, I may have found that TR1 and 2 were left rotated during the task, but would not know if they began there or how their position changed through the movement of the task. As TR1 and 2 begin in left rotation in the standing screen, and I felt TR1 and 2 move into left rotation during the task, I can interpret this as moving further into left rotation as compared to their starting position.
Summary of incongruencies:
The incongruencies will be described if the findings are incongruent to the task.
The cranial region is incongruent to the task, as it should be facing forward with no rotation.
C2 is also incongruent to the task as it should be neutrally aligned under C1 with no rotation.
The left clavicle is incongruent to the task between position 2 and 3 as it should not compress medially during the task.
C7 and thoracic ring 1 and 2 are both congruent to each other and the task.
- Diane’s comment:
In your biomechanics of the task described above, you state for Position 2 – if the unwinding of the thorax rotation is not fully achieved by the lower cervical spine, the upper cervical spine should rotate further into right rotation to keep the eyes forward. C2 is doing just this – it is right rotating; however, is this right rotation relative to C3 or C1, and why does this matter when interpreting the data, you have found?
- Kate’s response:
C2 is rotating right relative to C1. C3 is also right rotating but is congruent with C2. This is important because C1 is incongruent to C2 and the requirements of the task. It is important as it determines if the driver is the cranial region and therefore the AA joint or if it is the cervical region at the C2-3 joint.
Driver for functional unit 2
Primary Driver
Cranial region
Clinical reasoning: It must be noted that initially, articular restrictions had to be addressed in the OA and AA joint in order to get a full cranial region correction, the details of these articular restrictions can be found in further assessment. A full cranial correction was completed by unwinding the left ICT and stacking the OA joint. I had to manually correct the AA joint at C2 by unwinding C2 to stack under C1. This correction of C2 was an indirect correction at the AA joint, and did not impact the C2-3 segment as C3 followed C2.
- Diane’s comment:
When you say ‘stacking the OA joint’ do you mean you aligned the corrected cranium to neutral over the atlas? And then to ‘manually correct the AA joint at C2’ – I’m not sure I know what an ‘indirect correction at the AA joint means’. At the end of the complete cranial region correction (after releasing articular vectors) was the goal to have the corrected cranium in neutral over the atlas and the atlas in neutral over C2? If so, when all this was corrected, was the head calibrated to a zero/zero axis i.e. stacked over the rest of the neck?
- Kate’s response:
By stacking the OA joint, I mean that I aligned the cranium neutral over the atlas first. Then I originally tried to stack C1 over C2, but it was quite challenging to get it to rotate back over C2, which I think was because there was an articular restriction. Because I had difficulty with the right rotation of C1, I left rotated C2 to try and bring it back under C1, which is why I was referring to it as an indirect technique. I got the wording because in the Orthopaedic courses we can do a direct mobilization technique on the vertebrae above or an indirect technique by mobilizing the lower vertebrae to influence the joint. In my mind I was thinking that rotating C1 right and rotating C2 left at the same time to stack them was the closest I was able to get to a full correction. Probably should have just realized that not being able to get a full correction of C1 and an articular end feel might mean that I should have moved onto passive mobility instead of trying to complicate the correction.
- Diane’s comment:
This makes sense and is very difficult! When I can’t get a complete correction without force, I often wonder if I have not corrected something else that this segment is in relationship with OR if there is an underlying articular system impairment as you realized later. It’s all part of the learning process!
A cranial region correction then resulted in full correction of the left clavicle, TR1 & 2 in their starting position, full correction of C7 and resulted in the best experience of the task. A correction at C2 fully corrected the clavicle, TR1 & 2 in their starting position and C7 in the starting position, but did not impact the OA joint or ICT and did not generate the same change in experience.
Relationship of Drivers from FU#1 and FU#2
Co-driver
Cranial Region (cranium, atlas) and Thorax (TR4 & 5)
Secondary driver
Pelvis and Right hip
Clinical reasoning: a primary driver will correct all other sites of impairments completely. A secondary driver will partially correct when the primary driver is corrected, but has no impact on the primary driver. There are two types of co-drivers. The first is with two primary drivers and that when either is corrected, they improve the other fully. The second type is when the drivers are corrected individually, they either worsen or don’t change the other driver, but when they are corrected together then the task and the experience are both positively changed. This case is the second type of co-driver which requires the primary driver from functional unit 1 and functional unit 2 to be corrected together. When thoracic rings 4 and 5 were corrected they negatively impacted functional unit 2 by worsening right head and neck rotation.
The functional unit 2 driver, cranial region, did not correct thoracic rings 4 or 5. When completing a co-correction of the thorax AND the cranial region this resulted in the best experience of the task. It also fully corrected the transverse plane rotation of the pelvis, where it then was free to move into a right transverse plane rotation into position 2 and 3, but again did not result in FULL control of the right SIJ at the very end of the task. It also resulted in the right hip being fully corrected until the very end range of the task where it still moved anterior relative to the left, but no longer sheared. Therefore, for position 1 and 2 there is co-driver of the thorax and the cranial region. Moving into position 3 there are then additional secondary drivers; the pelvis and right hip.
- Diane’s question:
It is interesting that the TPR of the pelvis fully corrected for positions 2 & 3 (RTPR) yet at the end of position 3 when the pelvis was in a RTPR, the right hip became incongruent to the left hip and didn’t shear relative to the right acetabulum. Any hypothesis as to why this sudden right hip/pelvis TPR incongruence?
- Kate’s response:
My hypothesis is that Mrs. D was working her gluteal and hip external rotators quite hard to achieve the required hip range of motion for the task. I visualized this similar to a butt grip strategy where the posterior musculature recruitment creates compression around the hip joint before full range of motion is achieved and this could potentially create an anterior net vector of force. Additionally, the arthrokinematics glide that would occur with extension in combination with external rotation would be an anteromedial glide. If there is reduced active or passive control in the right hip, the ability to withstand the anterior vector at end ranges of extension may not be enough to prevent the right hip from sitting anterior.
Functional Unit #3
This unit was chosen to be part of the assessment because Mrs. D’s history of a significant right ankle sprain. Additionally, she is wearing skates when completing the task on the ice which were described to be stiff and it was hypothesized that this could potentially impact the foot and any adaptation that may be occurring. Mrs. D also brought in her skates in the subsequent session which resulted in the same functional unit 1 and 2 driver findings.
Standing Start Screen Findings
Right Knee:
Screw home mechanism intact. Right knee stacked over foot
Hindfeet:
Left hindfoot stacked in standing. Right hindfoot positioned with the talus slightly anterior and more loading over the lateral edge of her foot.
- Diane’s question:
Was there any notable tilt in the coronal plane of the right talus? When the loading is more lateral over the foot, this can cause a variety of changes in position of the subtalar joint, what did you notice here? Anything notable in the mid or forefoot?
- Kate’s response:
There was no notable tilt in the coronal plane for the right talus, the right subtalar joint was supinated. From my perspective it seemed that the lateral loading was related to her centre of mass being off centre to her base of support with more weight into the right extremity. The mid and forefoot were noted to be folded position.
Upper extremities were not further assessed as they remain in optimal positioning throughout the task.
Screening task findings – C-cut drill position 1/2/3
Knee:
Left remains stacked in slight knee flexion. Right maintains in optimal positioning with proper biomechanics and control for all three positions of the task.
Hindfeet:
Left maintains optimal alignment and biomechanics; right talus remained anterior, laterally loading the foot and between position 2 and 3 the heel elevated, putting the talocrural joint into a relative plantar flexed position.
- Diane’s question:
Same questions as above – was there any tilt associated between the right talus and the mortice and where was the subtalar joint?
- Kate’s response:
There was no tilt of the talus that I picked up in the mortice. The subtalar joint was in supination through the arc of movement until she was no longer able to keep her foot on the ground and her heel lifted and the weight bearing transferred to the forefoot.
Summary of incongruencies:
The right hindfoot is incongruent to the task; the talus is anterior in the mortice and remains that way throughout the task; additionally, the talocrural joint moves into a plantar flexed position with the heel elevating when it should remain flat in the skate.
Driver for functional unit 3
There were no drivers for functional unit 3.
Clinical reasoning: Correcting the right hindfoot improved starting position of the foot, but it worsened the experience of the task. Interestingly, putting the foot into the skate also worsened the experience of the task.
Relationship of driver(s) in functional units #1, 2 and 3
Correcting the co-driver from functional unit 1 and 2 completely corrected the right hindfoot and the heel was able to remain in contact with the ground throughout the entire arc of movement.
Final drivers for all three positions of the C-cut drill task
Co-Drivers: Cranial Region & Thorax
Secondary: Pelvis and Right hip
Further Analysis of the Drivers
Once the driver(s) have been prioritized, further analysis of the driver(s) follows. Further analysis of a driver includes tests of active mobility and passive mobility. Active and passive listening can occur during the mobility tests which allows vectors of pull to be analysed and to determine the underlying system impairment (neural, articular, myofascial, or visceral). Further assessment also includes passive control tests to assess form closure and joint stability (if necessary) and active control tests which evaluate motor control strategy and force closure mechanisms.
Further assessment of the cranial region
Craniovertebral Region
Active mobility
Right head and neck right rotation was assessed because in the task the head should be facing forwards with no intracranial torsion, instead of in the left intracranial torsion. Right rotation of the head and neck was also noted to worsen when the thoracic rings 4 & 5 were corrected. Right rotation of the head and neck was limited early with the head moving off axis at the initiation of movement. Craniovertebral flexion was limited at the right OA joint which resulted in chin deviation to the left.
- Diane’s question:
In your FU#2 Start screen findings, you note that the cranium was in a LICT and C1 was left rotated. During craniovertebral flexion the chin deviated to the left and suggest this was due to a restriction of the right OA joint. However, the deviation of the chin to the left may have nothing to do with the OA joints. Describe the arthrokinematics of the OA joints if the LICT was associated with a neutral C1 (neutral in the transverse plane); which way would the chin deviate? Then describe the arthrokinematics of the OA joints if C1 was rotated left congruent with the ICT and explain why this relative position could NOT be the cause of the left deviation of the chin.
- Kate’s response:
The LICT relates to the position of the intra-cranial torsion and not the position of the OA joint. The OA joint arthrokinematics during flexion are a bilateral anterior roll with posterior glide. If C1 is neutral the arthrokinematics are the same – bilateral anterior roll with posterior glide which would not result in a deviation of the chin. With C1 in left rotation, which is impacting the AA joint, the OA arthrokinematics would also remain the same. The relative position of C1 on C2 would not impact the OA joint and therefore the relative position could not be the cause of left deviation of the chin. The chin deviation could potentially occur due to the right rotation of C2 and C3 which can be coupled with ipsilateral side flexion which could contribute to the chin deviation left.
*I am unsure about this question. I was wondering if there is an ICT, in the ISM Series it was noted that the occipital bone follows the posteriorly rotated temporal bone. Would this influence the OA joint?
- Diane’s response:
Absolutely!
- Diane’s response:
If the atlas was in neutral alignment (i.e. in the coronal body plane) and there was a starting position of a LICT, with NO OA joint restriction, the chin should deviate to the right during CV flexion (the left condyle would reach the end of the posterior glide before the right thus the chin deviation to the right) because the occiput is left rotated right sideflexed on the atlas. If C1 was rotated left in the transverse plane congruent with the ICT but less than the rotation of the occiput, as you mention above the OA joint would still be right sideflexed/left rotated relative to the atlas and the deviation of the chin on CV flexion would still be to the right. The only scenario by which the chin deviation could be to the left was IF the right OA joint was restricted. Therefore, neither the start position of the ICT (left), nor the atlas rotation, are responsible for the direction of deviation of the chin – the OA joint restriction is. Now then, you didn’t have to figure out all these arthrokinematics to know that in this assessment, the key findings was that with the cranial correction the neck didn’t automatically lengthen/unwind – this suggests, at minimum, that there were vectors between the cranium and the CV region.
When attempting to correct C2 in order to accurately assess the mobility at the AA joint, I was not able to correct it fully due to an articular restriction at the left AA joint. When AA joint mobility was assessed, there was little to no movement available into right or left rotation at the AA joint before side flexion of the neck occurred off axis.
- Diane’s question:
You note that C1 was left rotated and C2 right rotated, I assume this is ‘in space’. The AA joint may; therefore, be fully left rotated, which could explain the inability to feel any further left rotation. You also note that you couldn’t fully ‘correct C2’ i.e. bring it back to neutral from a right rotated position. If you are correct and the articular dysfunction was at the left AA joint, was the arthrokinematic restriction an anterior or posterior glide of the atlas on the axis and why? If the restriction was at the right AA joint, which direction of arthrokinematic glide of the atlas on axis would have been restricted. How did you differentiate which joint was restricted simply through a correction of C2?
- Kate’s response:
Yes, in space, placing the AA joint in full left rotation. If it was the left AA joint that had the restriction, the anterior glide of the left AA joint would be restricted. Because of the starting position of the joint, the atlas is starting in end range posterior glide on the left. If the right AA joint had the restriction, it would be the posterior glide of the right side of the atlas on the axis.
I should have worded this differently. Originally, I tried to correct C1 by right rotating in onto C2 to stack the AA joint. When I attempted this, I found it to be quite difficult which made me think it was an articular restriction and I should have probably just stopped there. Because in the orthopaedic levels I had in my head that we could do direct joint techniques on the vertebrae above and indirect on the joint below, I thought that trying to rotate C2 left in an attempt to ‘indirectly’ rotated C1 right was another way to try and complete this correction. So technically, I guess I determined that the AA joint was restricted when it was challenging to fully correct C1 and specifically when it was challenging to anteriorly glide the left side of the atlas on the axis. On reflection, I probably should have stopped here and assessed passive mobility to confirm my finding and mobilize the joint that was restricted to be able to complete a full cranial region correction.
- Diane’s comment:
Well-reasoned! If the starting position of any joint isn’t considered the results of mobility testing (either direct or indirect ala the orthopaedic courses you’ve taken) may be falsely interpreted.
Passive mobility
Passive mobility of this region was assessed and a full cranial region correction that included the OA and AA joints was not possible. The OA and AA joints were both being limited by an articular system impairment. This was first assessed through Passive Listening #1 (feeling for the first vector when passively moving a region) and there was no ‘rocking back’ motion of the atlas on the axis when the twist was taken out of the cranium. On osteokinematic testing there was reduced flexion at the right OA joint and right rotation at the AA joint.
- Diane’s question:
When testing mobility of the OA joint, in addition to correcting the ICT, it is important that the occiput be tested in the plane of the atlas. The atlas (C1) was rotated to the left and was unable to be corrected. Did you test the OA joint in the plane of the rotated C1 or with the head in neutral and the C1 position not considered? Why could the posterior glide of the right OA joint be ‘apparently restricted’ if the plane of the OA joints (atlas rotated left and unable to be corrected) is not considered?
- Kate’s response:
I tested the OA joint in the plane of the atlas by stacking the occiput onto C1 into left rotation. If the plane of the OA joint had not been considered it could result in incorrect findings, this is similar to the stability testing of the CV region where false positives could occur due to the starting position of the joints which can create relative slack in the ligaments, which resolves when the joint is tested in the correct position. If the plane of the OA joint had not been considered and the occiput was in neutral and C1 was left rotated, the right OA joint would have been starting in an end range posterior glide and when assessing the available joint glide, the end feel would be early. This early end feel would occur NOT because the joint glide was restricted, but rather because the joint was already starting at its end range of motion. This indicates the importance of considering the starting position of the joints prior to assessing their kinematics.
- Diane’s comment:
Yes!!!
Arthrokinematic mobility testing revealed a reduced posterior glide at the right OA joint and reduced anterior glide at the left AA joint.
On passive listening #2 for both the OA and AA joint the vector of restriction was determined to be articular. After addressing the articular restrictions, which was required to get a full cranial region correction, a second passive mobility assessment was done once the cranial region was determined to be one of the drivers. Additional, vectors were found at the anterior aspect of the right transverse process of the atlas creating a short anterior pull determined to likely be rectus capituus anterior and myofascial.
Active and passive control
Once C2 could be corrected fully, the active and passive control of the OA and AA joints could be assessed. Active and passive control were assessed due to history of priory injury and to determine any underlying instability after removing the articular restriction. There was no loss of active or passive control at the OA and AA joints.
Cranium
Active mobility
Active listening of the cranium (LICT) through head and neck rotation to the right, Mrs. D was not able to move into a RICT and the active restriction appeared to be an inability to fully anteriorly rotate the left temporal bone.
- Diane’s comment and question:
In general, when we are using active listening during head and neck to determine the first suboptimal region in FU#2, the ‘listening’ hand is on the top of the head. However, the mobility of the temporal bones is not palpable through this approach. When you were using active listening to the cranium during head & neck rotation to the right, where were your hands placed to pick up this limitation of anterior rotation of the left temporal bone.
- Kate’s response:
The base of the thumbs were places on the mastoid processes with the rest of the thumbs running along the occipitomastoid suture. The rest of the hand lays lightly onto the rest of the cranium.
- Diane’s response:
Perfectly clarified!
Passive Mobility
The LICT was corrected easily and when the correction was released, the first bone to move was the left temporal bone into a posterior rotation. The vector of pull was a short pull into the left base of the skull which was hypothesized to be the left sub-occipital muscles (specifically rectus capituus posterior minor, and major.
The second listening was a longer medium length pull down the back left side of the neck into the upper thorax, hypothesized to be splenius capituus and semispinalis capituus.
Further assessment of the thorax
Active mobility:
The thorax needs to be able to move into ascending left rotation during the task, to unwind the required right transverse plane rotation of the pelvis; therefore, left rotation was chosen as the relevant mobility test for the thorax. Thoracic rings 4 and 5 were glued, and the ring stack and breathe technique (RSAB) (LJ Lee) was used to restore independent movement between these two rings. Subsequently, thoracic ring 4 was the priority ring to assess as it remained positioned incongruent to the requirements of the task (rotated right). During left thoracic rotation, thoracic ring 4 rotated further to the right and translated further to the left. Correcting the 4th thoracic ring improved range of motion into left rotation. Thoracic ring 5 was also checked into right rotation and worsened through range.
- Diane’s question:
If TR4 was your priority ring, and you have released the two rings, why did TR5 worsen during right rotation?
- Kate’s response:
Ring stack and breathe helped to create independent motion between the two rings. TR5 was still left rotated after release with ring stack and breath, but I determined it not to be as important because it was congruent with the requirements of the task. There are potentially still vectors preventing it from moving into right rotation, but this should not have been assessed as it is not related to the left thorax rotation required for the task.
Passive Mobility:
Passive mobility was assessed including passive listening 1 and 2, which helped to determine that thoracic rings 4 and 5 were glued. The first vector felt was a strong short vector between thoracic rings 4 and 5 hypothesized to be the intercostal muscles. As mentioned above, RSAB was used to unglue the thoracic rings in order to further assess each ring individually for vectors. The second passive listening 1 and 2, for thoracic ring 4 led to a vector that pulled the ring left, anterior and superior which was determined to be from the left serratus anterior. An assessment of thoracic ring 5 led to the same vector of pull from the right serratus anterior. Release was completed on both serratus anterior muscle fascicles. Passive listening was completed after the release on thoracic ring 4 again which led to a third vector of pull on the right 4th rib into posterior rotation with a long pull down the back determined to be iliocostalis.
I did continue to assess the 5th thoracic ring, not determining it as the primary ring of importance and in this case may have been treating reactors as well now that I am reflecting. TR4 would have been the most important vectors to address to be able to obtain left rotation required for the meaningful task.
- Diane’s question:
Were you able to passively correct and facilitate full left rotation of TR4? This is the first part of determining passive mobility. The passive listening for vectors is the second part of passive mobility testing.
- Kate’s response:
Once the rings were unglued, I was able to get a full correction of TR4 through left rotation.
Active control:
Active control was not tested during the first session as the vectors influencing mobility of the thoracic rings still needed to be released. When assessed in future sessions, Mrs. D was able to maintain control in arm elevation into the three skating positions.
Passive control:
Passive control was not assessed in the first session due to the presence of vectors influencing mobility of the thoracic rings. I did not determine it to be necessary to assess in future sessions as there was no history of trauma to the thorax in her story and after releasing the vectors of restriction, she was able to maintain active control with arm elevation.
Hypothesis
Mrs. D is hypothesized to be experiencing right hip and pelvic girdle pain and weakness due to poor alignment, biomechanics and control in four regions of the body. In a complex task such as figure skating, the body must be free to create congruent and incongruent rotations between the pelvis, thorax, cervical spine and cranial region. This requires adequate active mobility and control to dissociate and create diverse movement patterns for skating drills without overloading an area.
Mrs. D’s first injury was an upper left cervical spine injury that occurred in university while bagging groceries, this area was never treated and left her with underlying head and neck rotation deficits and feelings of tension on the left side of her neck. Furthermore, she worked a sedentary desk job for many years, and computer work can often result in head forward posture that can impact craniovertebral flexion range. Lastly, one year prior to starting her work teaching skating she suffered another fall impacting her tailbone and resulted in a concussion. These multiple events, without treatment, likely impacted her AA joint’s ability to unwind the descending rotations from the left ICT and AA joint left rotation. The greater occipital nerve which is a branch of C2 and C3 spinal nerve dorsal rami, exits the intervertebral foramen between C1 and 2. As the left AA joint was held in end range left rotation this postural imbalance has the potential to reduce the foramen space and create compressive forces or traction on the nerve root. The greater occipital nerve supplies semispinalis capituus which was one of the muscular vectors that contributed to the myofascial pull on the left temporal bone into posterior rotation. The semispinalis capituus originates from the nuchal region with the suboccipital muscles, and extends inferiorly to attach to the transverse processes of T4. Mechanical trauma to a nerve through axial rotation and compression can contribute to an alteration in physiology (Foundations Health Education Manual, 2023). Torsion of 9 degrees of axial rotation can alter nerve conduction and function and increase the stretch of a nerve root (Foundations Health Education Manual, 2023). This can often manifest as short taught bands in muscles which can decrease range of motion and increase compression on the articular system. This shortening or taught bands in semispinalis capituus could potentially result in contralateral thoracic rotation when activated unilaterally, which has the potential to disrupt the 4th thoracic ring causing left translation and right rotation.
When Mrs. D performs a C-cut drill in figure skating, she needs to be able to move her middle and upper thorax into left rotation. During the screening task, TR4 moved incongruent to the required task biomechanics, which I hypothesized was due to the thorax compensating to the impairments in the cranial region. The thoracic rings are all in relationship to each other, and the descending thoracic ring rotations in TR5, 8 and 9 are potentially compensations as a result of TR4 right rotation. In the ISM assessment, correcting the functional unit 2 primary driver did not correct TR4 and 5 and it was hypothesized that the cranial impairment and thoracic compensation likely had been ongoing for many years which resulted in two sites of impairment requiring a co-correction. Additionally, because of the potential length of time for these compensations to occur, the pelvis and right hip had also developed impairments. The erector spinae get their segmental innervation from the dorsal rami of the thoracic spinal nerves and therefore the axial torsion and compression between TR4 & 5 and TR8 & 9 could result in neural traction and compression which can result in taught bands into the erector spinae. Additionally, the erector spinae can react to the thoracic ring rotations to act as a brake to prevent further rotations. The right iliocostalis is one of the vectors from the right rib of the 4th thoracic ring attaching caudally to the right innominate (PSIS region). This vector of force can contribute to anterior rotation of the right innominate relative to the sacrum potentially resulting in an unlocking R SIJ.
Mrs. D has a birth trauma from 13 years prior during a trial of labour followed by a cesarian section, both of which she did not receive any formal rehabilitation. Both of these macro traumas can result in an altered force closure mechanism at the pelvis due to the injury to the muscles and the inhibition of the deep core that can occur with an abdominal wall incision such as during a cesarian section (Saha etc al. 2021). With the altered deep system activation that can occur after a cesarian section, there is a potential that Mrs. D has reduced capacity in her deep system. This reduced capacity may impact her ability to manage descending vectors, such as the right iliocostalis, that has the potential to disrupt motor control and further impact her pelvic active control. Over time, the destabilized pelvis will use alternate strategies for control that often involve overactivation of the pelvic floor which can lead to stress urinary incontinence (SUI).
Additionally, incongruent rotation of thoracic rings 8 and 9 could potentially alter neural drive to the abdominal muscles (supplied by T7-12 spinal nerves (Lee, 2017)). This may make it more difficult to recruit transverse abdominis and therefore Mrs. D may recruit non-optimal strategies such as increased recruitment of external oblique. The external oblique has connections to the serratus anterior muscle through myofascial interdigitations and can further contribute to upper and lower ring rotations and translations. Over-activation of the external oblique also is noted to increase intra-abdominal pressure and may also be a contributing factor to her SUI.
After addressing Mrs. D’s co-drivers in the cranial region and thoracic spine, there was improvements in both pelvic active mobility and active control. Full SIJ control was not restored and attention to the pelvis and right hip would be required at future sessions. Assessment of these secondary drivers help to clarify the mechanism of this relationship.
Treatment
Release
Cranial Region
- OA: Articular mobilization right OA joint – Right posterior glide C1 on C2; Grade 4 sustained hold
- AA: Articular mobilization left AA joint – left indirect technique for C1 anterior glide via posterior glide C2; Grade 4 sustained hold.
- C1: Soft tissue release of right anterior vectors of rectus capituus anterior & neuromuscular vectors
- Cranium: soft tissue release of left sub-occipitals. Release with awareness of left splenius capituus and semispinalis capituus
- Home exercise program (HEP) was to continue self -release at the nuchal line and mastoid to address the suboccipitals and semispinalis/splenius capituus
Thorax Region
- Facilitate independent mobility of thoracic rings 4 & 5 using RSAB
- Soft tissue release and release with awareness for left and right serratus anterior vectors
- Release with awareness and dry needling for right iliocostalis – TR4 fascicle
- Home exercises of sumo stretch bilateral to address serratus anterior and lengthen through the right iliocostalis. Also, to provide the thorax with decompression
- Self RSAB was taught for thoracic ring 4
Align
Thorax region
- Cues given for skating to think of creating space between TR4 and TR5 when rotating left
Connect
Pelvis
- Tape was applied to the posterior pelvis using fixomull and leukotape. Applied transversely across the posterior pelvis with compression to provide increased force closure to help control the right SIJ that did not fully regain motor control after addressing the co-drivers. Additionally, this was done to provide more support to Mrs. D who had to continue to teach skating later that day and to determine if she could feel any changes or impact of more control in her meaningful task.
- We did not get into teaching connect cues for pelvic floor or multifidus until later in future follow up sessions.
Move
- Integrate the align cue to for TR4 & TR5 when skating and rotating left.
Followup treatment for the primary co-drivers
The first four sessions where focused on the co-drivers (cranial and thorax regions). Follow up sessions were completed weekly. Mrs. D reported to have liked the experience of wearing the tape on her pelvis at skating after the initial treatment session, which we continued to complete in each session. She also did not report any flare in symptoms, which had typically occurred when she received local release at the hip and pelvis in previous physiotherapy appointments.
In these subsequent sessions, the vectors for the cranial region and thoracic rings 4 and 5 required further release. As these improved, thoracic rings 8 and 9 did improve, specific vectors impeding their unwinding did show up and required treatment (e.g. external oblique).
Further analysis of secondary drivers
After 4 sessions focusing on the cranial and thorax regions, we were able to transition our focus to the secondary drivers, the pelvis and right hip. We did continue to monitor the cranial and thorax regions for any recurrent impairments which were treated as necessary.
Further Assessment of the Right Hip
Active mobility:
This was assessed during the screening task.
Passive mobility:
This was not assessed as she had previously seen other physiotherapists and reported working on mobility and found this had worsened her symptoms. This made me think that the issue was potentially related to control, and I did not end up assessing specific passive mobility.
Active control:
After addressing the cranial and thorax regions, there was an improvement in hip active control and she was able to maintain a centered position until the very end of the task.
Passive control:
This was not assessed.
Further Assessment of the Pelvis
Active mobility:
This was assessed during the screening task. After addressing the cranial and thorax regions, the pelvis was able to move into a right transverse plane rotation through the entire C-cut drill.
Active control:
This was assessed during the screening task. After addressing the cranial and thorax regions, although the pelvis was able to move into a right transverse plane rotation through the entire C-cut drill, she still lost control of the R SIJ between positions 2 and 3. The rest of the testing for active control is outlined in the motor control analysis below.
Passive mobility:
During passive mobility testing, the pelvis was placed in a neutral TPR IPT and an anteroposterior glide was applied in the plane of the joint. There was reduced excursion at the right sacroiliac joint at the superior pole. The vector causing the reduced motion was determined to be the right superficial fibres of multifidus (sMF).
Passive control:
This was tested because there was loss of SIJ control, that improved but did not fully resolve with the correction of the cranial and thorax regions into position 3. As Mrs. D has a history of a trial of labour and a fall onto her tailbone while skating, it was important to check that the passive system was intact. To assess this, Mrs. D was on her back with the SIJ placed in a close pack position, an anteroposterior glide was applied to the R SIJ and there was no movement palpated and therefore determined that there was no loss of passive control.
- Diane’s question:
What is the close-pack position of the SIJ? In which zone of motion should there be no motion palpable, if the passive integrity is intact, and why?
- Kate’s response:
The close-pack position of the SIJ is the sacrum nutated relative to the innominate bones. If the SIJ is in a close-pack position, there should be no palpable motion in the neutral or elastic zone. No translation is possible because this position will tighten the capsule and articular ligaments of the SIJ.
Motor control analysis (lower fibres of transversus abdominis (TrA), sacral fibres of multifidus and pelvic floor):
Treatment of the cranial region and the thorax did not restore complete control of the R SIJ through the entire screening task; therefore, a motor control assessment of the pelvis is required.
Low fibres of TrA
A synergistic response of TrA occurred bilaterally in response to a verbal cue to co-activate the deep system.
Sacral fibres of multifidus
Notable inhibition of the right sacral fibres of multifidus with an erector spinae strategy during a left and right active bent leg raise task. With verbal cues to co-activate the deep system (TrA, sacral fibres of multifidus and the pelvic floor) she was able to recruit the deep multifidus but did not have the capacity to maintain the recruitment during the active bent leg raise load transfer test. She could tolerate lower loads such as a bent knee fall out.
Pelvic floor muscles
A summary of the significant findings from the real time ultrasound and internal vaginal assessment of the pelvic floor muscles:
- Pelvic floor muscle recruitment: Grade 3/5 strength and 4 second endurance. Quality of contraction: more recruitment in posterior pelvic floor as compared to the anterior pelvic floor.
- Evidence of a stage 2 anterior vaginal wall prolapse.
- Diane’s question:
Was there any notable change in the behavior of the sacral fibres of multifidus or the pelvic floor with a co-correction of her primary drivers. This could help to explain how correcting these regions deferred the unlocking of the SIJ in her screening tasks
- Kate’s response:
On reflection, I should have co-corrected her primary drivers when assessing her pelvic floor and sacral fibres of multifidus. I just assessed the motor control separately after multiple sessions had been focused on treating the co-drivers. In the future it would be beneficial to also assess the relationship between the co-driver and motor control to further explain the relationship.
- Diane’s comment:
Reflection always helps us be better. This would have helped you explain how her remote impairments (cranial and thorax regions) were impacting the function of her pelvis and hip consolidating the principles of how you work (ISM) for her.
Followup treatment for the secondary drivers – pelvis and right hip
Release:
- Release right superficial fibres of multifidus
- No hip vectors were assessed for or released at this stage due to previous negative response to treatment
Connect:
- Stage 1 motor control training: Connect cues for the pelvic floor and right sacral fibres of multifidus were taught individually. These were taught in supine, which is where she found it easiest to recruit these deep muscles and because the plinth provided external feedback to know if she was arching her lumbar spine or over activating through her erector spinae. After a few weeks, she was able to combine her connect cues starting with her pelvic floor and leading into her sacral multifidus. This also resulted in synergistic activation of transversus abdominis. Mrs. D worked on stage 1 for 2 weeks.
- Stage 2 motor control training: In this stage, Mrs. D worked on her connect cues to maintain R SIJ control and began to add load through her legs. The exercises she was able to progress through over the next month were: bent knee fall out to work hip rotation, clamshell (eventually adding banded load), heel slides and side lying leg abduction with. After a month she was able to progress into vertical loads and started with standing leg abduction with neutral rotation for the hip.
- The goal for future sessions is to continue to progress stage 2 motor control to take the legs into multiple direction leg lifts under the load of a resistance band and then add external rotation through the hip without losing the centred position of the right hip. Additionally, training will progress to vertical loading. From here the treatment plan will progress into stage 3 working on greater complexity of movement that challenges the pelvis and hip moving through range while also adding complexity with head and thoracic rotation positions.
Conclusion
Mrs. D was able to regain alignment and biomechanics of her cranial region, thorax and pelvis during position 1 & 2 of the right C-cut drill. She was not able to regain full control of her right hip and pelvis at the end range of the C-cut drill and is still working on progressing from stage two to three for motor control. She needs more time to build increased capacity in these muscles to be able to manage the loading required for this task and other drills for her skating job. She has also reported a noticeable reduction in her stress incontinence when jumping on the ice, reduced mid-thoracic spine discomfort and finds head and neck rotation tasks easier in her day to day life.
References
- Hodges, P., Cholewicki, J., & Van Dieen, J. (2013). Spinal control: The rehabilitation of back pain – state of the art and science. Churchill Livingstone.
- How to Ice Skate Backward. (n.d). In WikiHow. Retried Feb 7, 2024 from https://www.wikihow.com/Ice-Skate-Backwards
- Foundations Health Education Course Manual, 2023
- Shah, S., Vaishali, K., Prasad, S. S., & Babu, A. S. (2021). Altered patterns of abdominal muscle activation during forced exhalation following elective laparotomy: An experimental research. Journal of Abdominal Surgery, 10(2), 45-56. https://doi.org/10.1234/jas.2023.4567
- Lee, D. (2011). The pelvic girdle. Churchill Livingstone.
- Lee, D. (2017). Diastasis Rectus Abdominis: A clinical guide for those who are split down the middle. Churchill Livingstone.
Skills Demonstration
Case Study Author
Clinical Mentorship in the Integrated Systems Model
Join Diane, and her team of highly skilled assistants, on this mentorship journey and immerse yourself in a series of education opportunities that will improve your clinical efficacy for treating the whole person using the updated Integrated Systems Model.
We will come together for 3 sessions of 4 (4.5) days over a period of 6-8 months with lots of practical/clinical time to focus on acquiring the skills and clinical reasoning to put the ISM model into practice. Hours of online lecture and reading material and 12 hours of in-person lecture are...
More Info




