Story
Ms. C is a 40 year old female referred for a scoliosis specific assessment at Diane Lee & Associates. Ms. C presented with persistent, irritable, lower back pain, as well as intermittent pain that shoots down to the left foot or into the right thigh. At the time of the assessment, there were no identifiable 24/7 behavioural patterns of symptoms; although her symptoms used to be significantly worse in the morning, and at night; now the back pain is constant. The first occurrence of pain happened more than 5 months before the initial assessment. The client described the onset of pain as sudden after waking up from sleep. No change reported since, and perhaps slightly worsening.
- Diane’s question:
I’m diving deeper into this pain behaviour to try to truly understand. When you say ‘no change reported’ are you referring to the intensity of pain, its constancy, or its location or all three?
- Judit’s response:
The constancy and location of pain hasn’t changed, but its intensity might have worsened.
Past treatment included chiropractic and massage therapy and neither provided relief. Her chiropractor suggested a 6mm heel lift for leg length discrepancy, which she has tried but did not feel a major difference in her status.
- Diane’s question:
The word ‘status’ can imply something different than pain. Does this mean that she felt no difference in her pain or any other symptom (below you report she also complains of feeling twisted in her pelvis, uneven in her leg length and loss of center when she sits).
- Judit’s response:
I believe that this client has accepted long ago that her legs are uneven, and that her center of mass is off; this newly developed, irritable, back pain is her main concern – the status was referring to this pain that limits her everyday activities. The other ‘complaints’ are secondary to her meaningful complaint, but the client believes there is a link.
Despite her pain, Ms. C continues to live a very active lifestyle. She is horseback riding four to five times per week for 45-60 minutes. Her daytime job is sedentary, working on the computer. Her past medical history was quite remarkable for previous injuries; she has been regularly horseback riding since the age of 11 and has taken multiple major falls; in which she reported she ‘always landed on the left side’. Ms. C also suffered from two concussions; once a fall from a horse, and another from crossfit where she landed on her cranium.
- Diane’s question:
Has Ms. C had any children, and if so, did she report any complications or non-resolving issues secondary to her pregnancy that we need to consider?
- Judit’s response:
Ms. C has 2 children, both were delivered via C-section 15+ years ago. She developed Diastasis Rectus Abdominis for which she received surgical intervention (recti plication and abdominoplasty) followed by Pelvic Health Physiotherapy and reported complete resolution of problems since 2018.
Meaningful Complaint
Ms. C complained of a primary area of pain localized in the left side of lower back, along the iliocostalis lumborum and thoracic longissimus muscles. Pain also presented along the left iliac crest towards the midline where these muscles insert to the ilium. She also reported intermittent pain that shoots down to her left foot or occasionally into her right lateral thigh. She reports her back pain as constant and further aggravated every day by sport activities or postures.
While horseback riding, she reports difficulty finding her center of mass and her left hip always externally rotates. Similar to standing, she feels like she is leaning to one side and never centered.
Sleeping is not providing rest, she reports often getting ‘locked’ into certain positions that wakes her up and feeling even more stiff in the spine and pelvis. The phenotype of pain is identified as neuro-nociceptive with components of local nociceptive pain following activities, and intermittent neuropathic pain.
- Diane’s question:
According to the International Association for the Study of Pain, pain can be classified into three phenotypes; nociceptive, neuropathic and nociplastic. Above you have classified Ms C’s pain as a blend of pain (neuro-nociceptive). What findings from the story support this classification?
- Judit’s response:
Ms C’s primary complaint is pain along the lumbar paravertebral muscles that is localized, ‘aching’ and occasionally sharp in nature, and is further exacerbated by movement, which are the characteristics of somatic nociceptive pain. Nociceptive pain is a normal response to noxious stimuli that is initiated by the activation of nociceptors (primary afferent neurons). Neuropathic pain, in contrast, results from pain signals transmitted by the nervous system. Unlike her nociceptive pain (aching), neuropathic pain comprises spontaneously occurring, electric, sharp and shooting sensation.
- Diane’s question:
At the beginning of this report you note “At the time of the assessment there were no identifiable 24/7 behavioural patterns of symptoms; although it used to be significantly worse in the morning, and night time; now the back pain is constant.” And then later you note “She considers her pain as constant, that is further aggravated by every day and sport activities or postures.” To me, these are two very different phenotypes of pain behaviour – why do I say this and why does this matter?
- Judit’s response:
Recently, the International Association for the Study of Pain (IASP) released clinical criteria and a grading system for nociplastic pain affecting the musculoskeletal system. These criteria replaced the 2014 clinical criteria for predominant central sensitization (CS) pain and accounted for clinicians’ need to identify (early) and correctly classify patients having chronic pain according to the pain phenotype. Still, clinicians and researchers can become confused by the multitude of terms and the variety of clinical criteria available. Therefore, this paper aims at (1) providing an overview of what preceded the IASP criteria for nociplastic pain (‘the past’); (2) explaining the new IASP criteria for nociplastic pain in comparison with the 2014 clinical criteria for predominant CS pain (‘the present’); and (3) highlighting key areas for future implementation and research work in this area (‘the future’). It is explained that the 2021 IASP clinical criteria for nociplastic pain are in line with the 2014 clinical criteria for predominant CS pain but are more robust, comprehensive, better developed and hold more potential. Therefore, the 2021 IASP clinical criteria for nociplastic pain are important steps towards precision pain medicine, yet studies examining the clinimetric and psychometric properties of the criteria are urgently needed.
- Diane’s comment:
Whenever pain progresses from intermittent to constant (absolutely no periods of complete relief), I believe that some processing error (whether it is called sensitization or nociplasticity) is present. The implications for clinical practice is that we cannot not expect (and neither should the client) that pain will be a valid indicator of progress when this feature of pain is present, as appears to be the case here. The response to ‘better, worse or no change’ requires attention to another sensory feature, other than pain; at least at the beginning.
Cognitive belief
Ms. C has been feeling that her center of mass has always been ‘off’ since juvenile / adolescent years; always felt crooked in her pelvis, one side of her pants felt shorter than the other; always stood funny, leaning to one side and hiking up hip to stand ‘stable’. She believes that a leg length discrepancy might play a role in her ‘unevenness’ but is unsure why her back hurts and if the two are related.
- Diane’s question:
Ms. C has been feeling that her center of mass has always been ‘off’ since juvenile / adolescent years; always felt crooked in her pelvis, one side of her pants felt shorter than the other; always stood funny, leaning to one side and hiking up hip to stand ‘stable’. She believes that a leg length discrepancy might play a role in her ‘unevenness’ but is unsure why her back hurts and if the two are related.
- Judit’s response:
She did not wear the heel lift consistently and did not give it enough time. She was simply unsure if it was needed or not as it did not immediately resolve her symptoms. I approached her objective assessment with even more curiosity since it is important for this patient to have more clarity over limb length.
- Diane’s comment:
Ah, here it is. If she only pays attention to pain, and desires immediate resolution with a small intervention, then this phenotype (blended nociceptive/neuropathic/nociplastic) will not inform her nervous system of any benefit. Perhaps if she was able to note a change in alignment, or centeredness and had understood more about pain neuroscience she would have given the heel lift more time.
Emotional and medical considerations
‘Nobody ever listened to me when I was little, and things hurt a LOT. My parents took me to doctors but I was always dismissed without a diagnosis, so I got used to it.’ Ever since this painful episode started, she feels exhausted and cannot rest well. Ms. C opened up about being diagnosed with anxiety, bipolar 2, depression, and ADHD. She started taking prescription medication but recently tried to avoid medication due to their negative side effects. She also suffers from migraine headaches since elementary school and reports trying ‘every’ medication. She currently receives Botox injections every 3 months to the muscles of her neck and cranium and this seems to help.
- Diane’s question:
This may come up later in this report if you need to get into functional unit #2; do you know specifically which muscles receive Botox for her headaches?
- Judit’s response:
I did not ask her about which muscles she receives Botox. I found it interesting though: ever since you asked this question, I have been asking ALL of my patients and the answer most of the time is ‘all over the place’, or ‘always different’ or ‘the ones that the Dr feels tight that day’. I think not all practitioners have a direct assessment/treatment protocol and are going with the patient’s symptoms that day.
Meaningful tasks
Based on the subjective assessment, the meaningful tasks chosen were:
- Primary: being able to stand straighter
- Secondary: being able to sit straighter in general (future progression: on the horse)
Structural and Apparent Spinal Asymmetries
The term posture refers to the position of the body in space; and has the purpose of maintaining the body in balance, during dynamic movements and stasis. Several factors contribute to the posture, including neurophysiological, biomechanical and psycho-emotional. Posture is automatic and unconscious, it represents the body’s reaction to the force of gravity; and as any position that maintains balance with maximum stability, minimal energy consumption and minimal stress on the anatomical structures (F. Carini, M. Mazzola, C. Fici, et al 2017).
A good body posture is considered:
(1) ergonomically advantageous while standing,
(2) mechanically effective while moving, and
(3) supportive for the normal function of internal organs.
Poor posture on the other hand is an imprecise term commonly used in clinical practice to describe a relationship between various body parts which may be considered as faulty and which could stretch the spectrum from the non-perfect to pathological posture. It is postulated that poor posture can produce an increased strain on the supporting structures and less-efficient balance of the body over its base of support (Kendall et al. 2005).
Spinal alignment refers to the physiological curvatures that balance the spine in the coronal, sagittal and transverse planes. These physiological curvatures will be discussed during the physical assessment below.
From a clinical point of view, spinal asymmetries, or misalignment, are categorized as either functional or structural. For the context of this report, the word ‘apparent’ will be used instead of ‘functional’ since a minor misalignment can still be highly dysfunctional for an individual’s meaningful task.
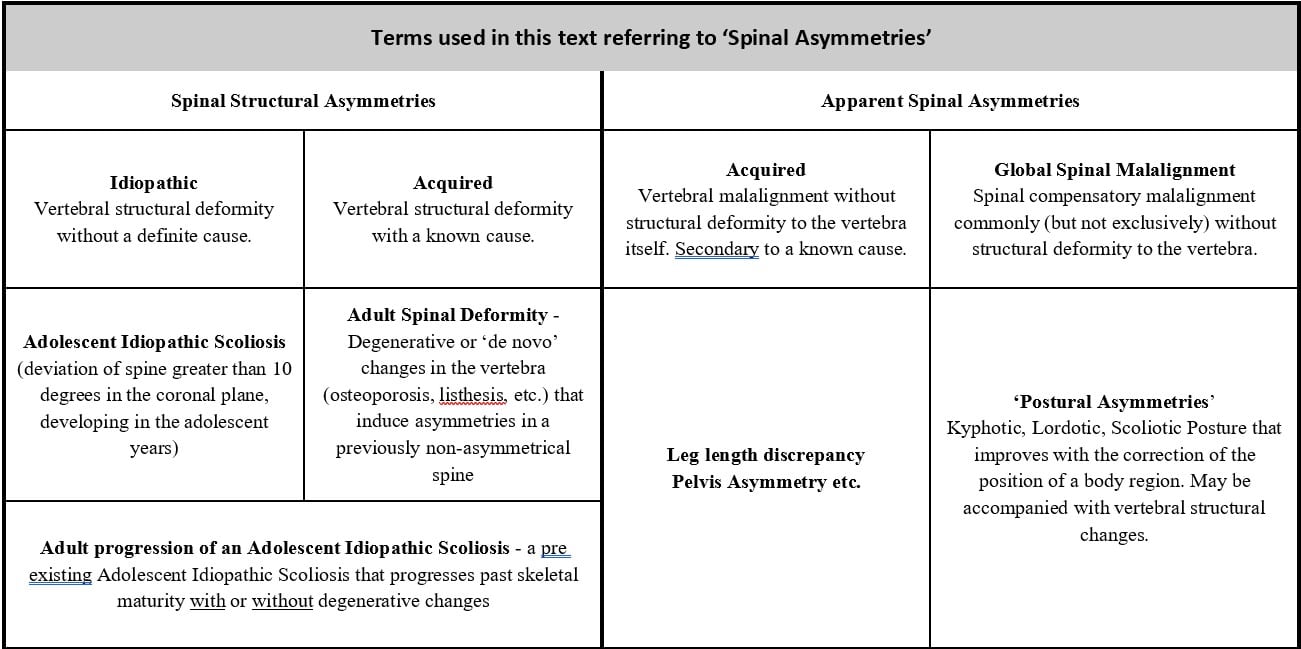
Table of Spinal Asymmetry terms used in this paper.
- Diane’s comment:
I love how you have simplified the complex categorizations for spinal deformities – this is very clear Judit!
Major apparent spinal asymmetries are not always associated with structural vertebral pathologies, but rather with over or under activation of muscles, restricted or unstable articular components, and/or adverse tension in the neural and dural structures. Treatment of these impairments resolves the spinal misalignment almost completely.
Unlike apparent spinal asymmetries, structural pathologies are mostly due to changes in the vertebra itself. The cause of these changes can be idiopathic, congenital, or acquired malformations (scoliosis, kyphosis, osteomyelitis, osteoporosis, spondylolisthesis). They can also develop secondary to structural changes of the pelvis or lower extremities that impact spinal alignment for prolonged periods of time, especially during the time of skeletal immaturity. These conditions might stand alone as specific clinical entities and require specific diagnosis and management, such as correcting the limb length discrepancy, instead of treating the spinal asymmetry.
How does the Integrated Systems Model help to differentiate apparent from structural spinal asymmetries? Structural spinal asymmetries present with more severe clinical problems and are less responsive to the manual corrections used in ISM. Furthermore, structural spinal asymmetries present with particular patterns in the sagittal, coronal and/or transverse plane unlike the asymmetries which are apparent and due to non-structural causes.
- Diane’s question:
In ISM we teach that non-responsiveness to manual corrections could be due to adverse neural/dural tension (something you mention above under ‘apparent’ spinal asymmetries). When there is marked adverse neural/dural tension, all corrections seem to make another body region worse. These individuals also can have ‘severe clinical problems’ and are exercise avoidant due to the lack of positive experience with any form of exercise. Can you expand a bit on how ‘severe clinical problems’ and non-responsiveness to manual corrections differentiates structural spinal asymmetries from apparent ones given what I have just mentioned about dural/neural adverse tension? What else is different?
- Judit’s response:
Structural spinal asymmetries and apparent asymmetries can both present with significant clinical challenges, but their underlying mechanisms and responses to interventions differ. While adverse neural or dural tension can complicate apparent asymmetries, it does not redefine them as structural. Instead, the differentiation hinges on the root cause of the asymmetry and its clinical presentation.
Non-responsiveness to Manual Corrections
Apparent asymmetries may appear unresponsive to manual corrections when neural/dural tension is marked. This resistance often stems from compensatory mechanisms or protective responses of the nervous system rather than a fixed structural pathology. Clinically, these individuals may exhibit widespread hyperalgesia, guarded movement patterns, and a lack of positive experiences with exercise, which contributes to kinesiophobia. However, with careful management, including strategies to address neural tension, these cases can show improvement over time.
In contrast, structural asymmetries are fundamentally tied to vertebral morphology (changes in bony alignment, relative anterior spinal overgrowth). Their non-responsiveness to manual corrections is due to the physical inability of the vertebral column to adapt to the corrections imposed, as the structural abnormality cannot be resolved through soft tissue or neural interventions alone.
In idiopathic structural scoliosis, vertebral pathology impacts multiple systems over time, including respiratory function (reduced lung capacity and altered blood gas values), musculoskeletal structure (asymmetric muscle tension and overloading), and neural elements (Anterior dural tethering can create adverse neural tension, contributing to pain or reduced range of motion). Manual corrections do not create physical changes in vertebral alignment but offer a counterbalance to habitual patterns, providing valuable feedback on the system’s adaptability and identifying potential pain-relieving postures. These manual corrections often have to be addressing 3 plains all at once in multiple body units – similar to co-drivers but with primary focus on the structure rather than the function.
Severity of Clinical Problems
Both structural and apparent asymmetries can present with severe clinical problems, but the nature of these problems often differs. Apparent asymmetries with adverse neural/dural tension manifest as multi-system dysfunctions, such as widespread pain, autonomic dysregulation, or heightened nervous system sensitivity, creating a barrier to functional improvement. If the apparent asymmetry persists for decades it has the potential to present as degenerative changes.
On the other hand, structural asymmetries can sooner lead to mechanical complications such as progressive deformity, joint degeneration, or localized pain syndromes directly related to the structural abnormality.
Movement and Postural Patterns
Structural asymmetries present with distinct and consistent patterns of deviation in the sagittal, coronal, and transverse planes, often visible on imaging and resistant to simple (non 3 dimensional) postural corrections. Apparent asymmetries, even with neural/dural tension, tend to be dynamic and modifiable to some degree, reflecting the compensatory or protective nature of the nervous and musculoskeletal systems.
Response to Exercise and Rehabilitation
While individuals with apparent asymmetries may initially avoid exercise due to a history of poor outcomes, tailored interventions addressing neural tension, graded activity, and movement education can lead to meaningful functional gains. Structural asymmetries, however, often require a more comprehensive approach that includes biomechanical adaptations, scoliosis-specific physiotherapy (e.g., Schroth or SEAS methods), and thoracolumbosacral orthoses (TLSO) to prevent curve progression and improve alignment. These conservative strategies can enhance postural control, reduce discomfort, and optimize function. In severe or progressive cases, additional measures such as surgical consultation may be considered, but conservative management remains foundational in most instances.
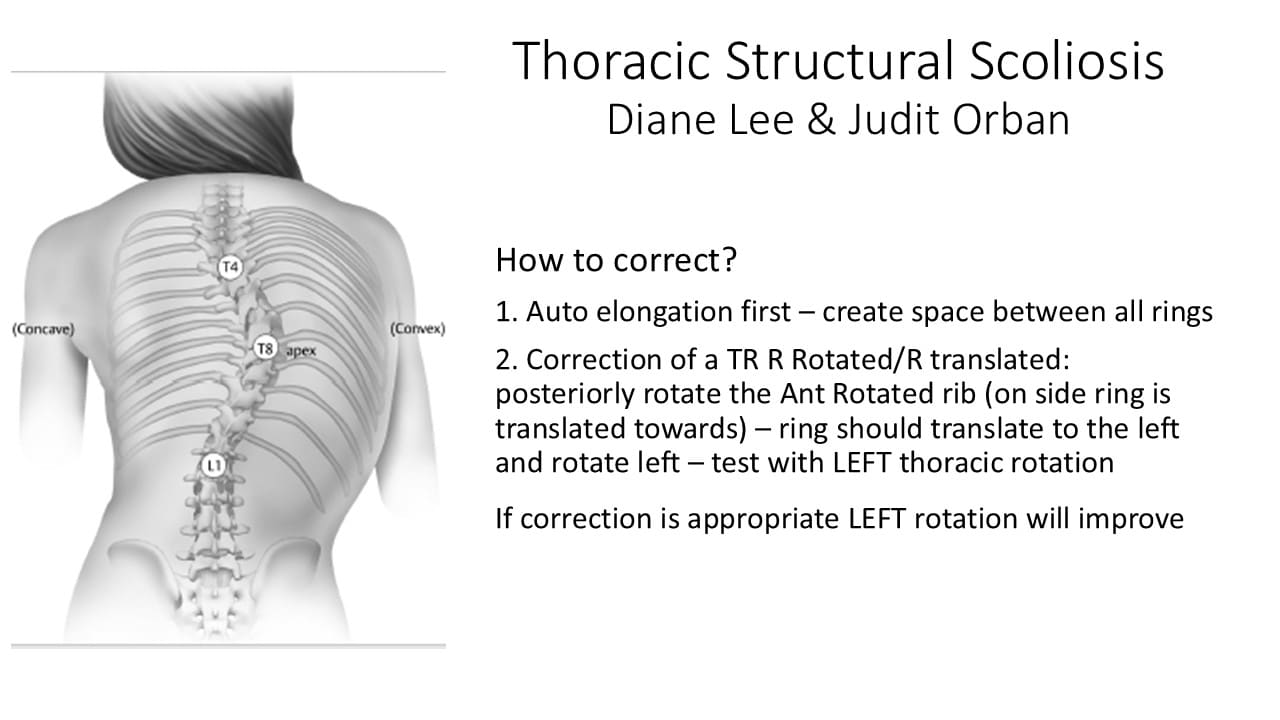
Scoliosis: idiopathic vs. degenerative
Scoliosis is a general term comprising a heterogeneous group of conditions consisting of changes in the shape and position of the spine, thorax and trunk (SOSORT – The International Society on Scoliosis Orthopaedic and Rehabilitation Treatment).
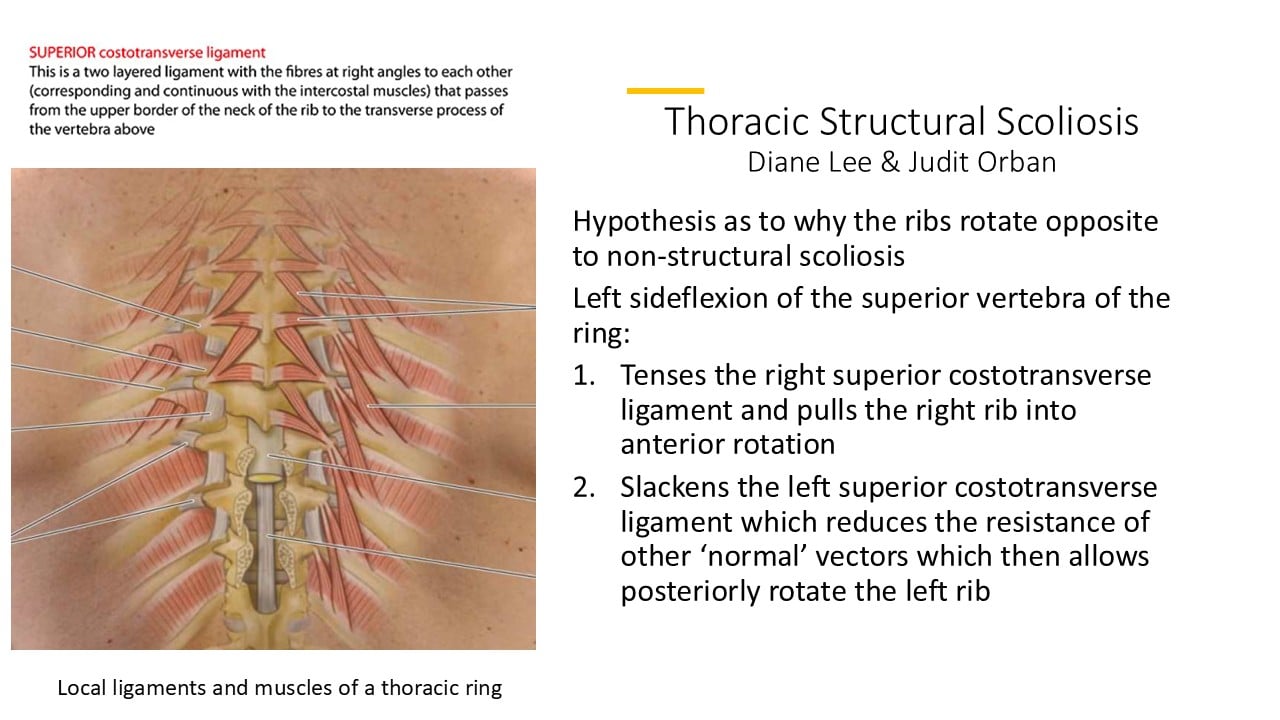
The term ‘idiopathic scoliosis’ was introduced by Kleinberg (1922) and it is applied to all patients in which it is not possible to find a specific disease causing the deformity. Idiopathic scoliosis can progress secondary to multiple factors during rapid periods of growth. According to the Scoliosis Research Society (SRS), a diagnosis of scoliosis is confirmed when the Cobb angle (Fig 1) is 10° or higher; and axial rotation is evident. However, idiopathic scoliosis can present with a Cobb angle under 10° with a potential for progression. Rotation can be delayed, and can significantly progress in adulthood.
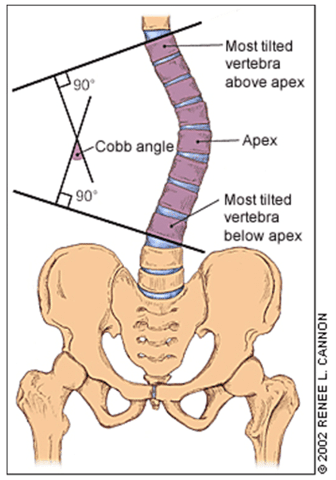
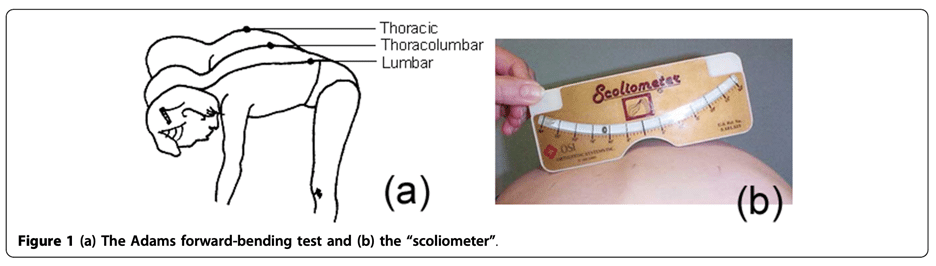
X-ray imaging is the gold standard for diagnosis of idiopathic scoliosis; however, children are not exposed to X-rays for screening purposes, because of the radiation risk. An alternate method for screening for idiopathic scoliosis is a clinical examination using a scoliometer to measure axial rotation in the forward bending position (standing or sitting). This is called the Adams test (Fig 2). When axial rotation is more than 5-7 degrees during the growing period, patients should obtain the gold standard diagnostic X-ray imaging in standing in both the anterior-posterior and sagittal views.
Adult spinal deformity and global spinal malalignment
Adult spinal deformity develops due to degenerative, or ‘de novo’, changes in the vertebra that induce asymmetries in a previously symmetrical spine. Lumbar and thoracolumbar scoliosis is a common feature of Adult Spinal Deformity (ASD), and current research reports the prevalence of ASD between 30-60%.
ASD can be accompanied by global spinal malalignment, back and leg pain, and decreased quality of life. It is not uncommon to develop ‘degenerative’ (or de novo, meaning ‘a new’) scoliosis in a previously completely straight spine due to spinal degenerative changes. These are typically recognized above the age of 60 in the older adult population, some research suggests the prevalence to be as high as 68%.
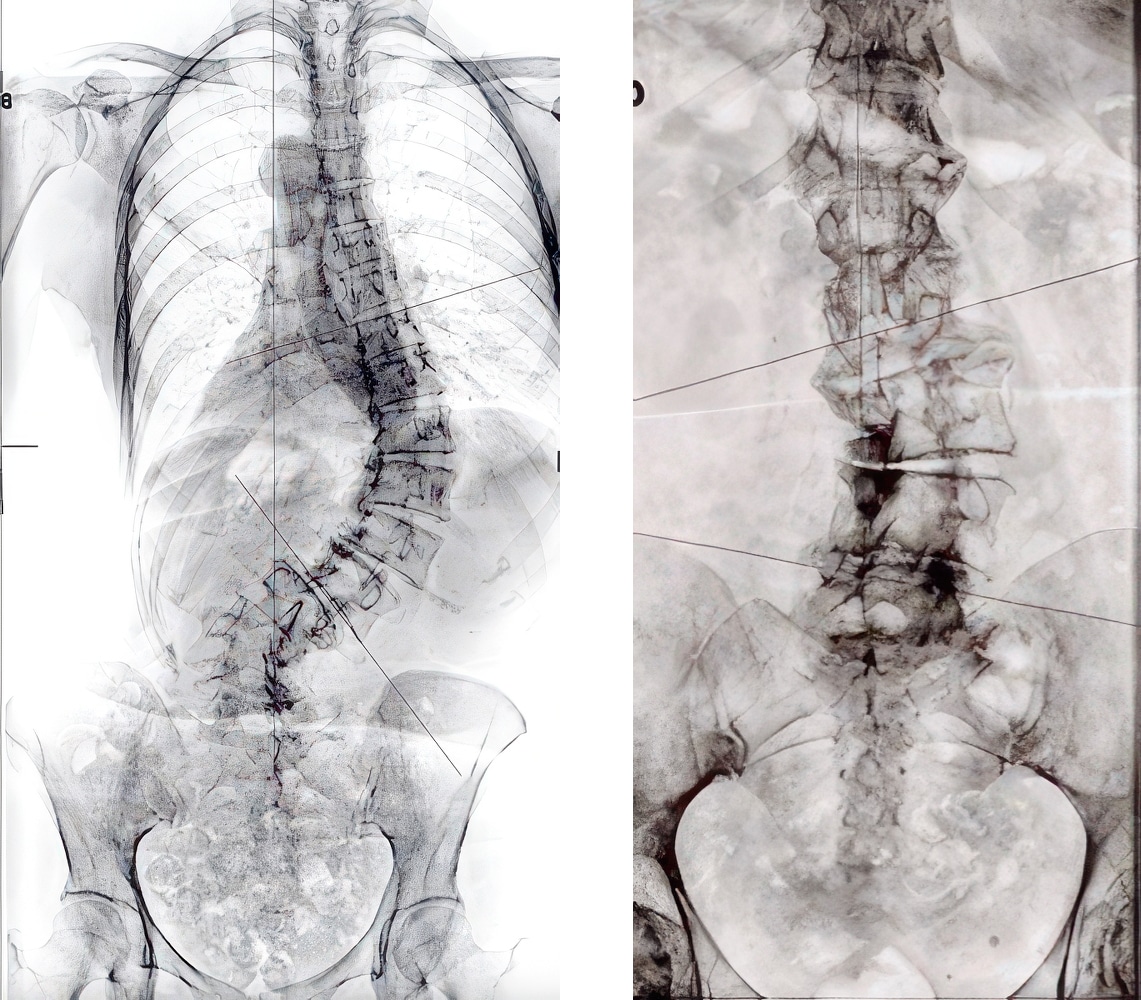
While the clinical presentation can be quite similar for two individuals with adult spinal deformity, their medical imaging shows many differences. Figure 3 shows an adult stage of idiopathic scoliosis on the left presenting with a ‘complete’ Thoracolumbar regional curvature; the right image shows an adult degenerative scoliosis with a lumbar segmental scoliosis and an incomplete curve.
According to the Scoliosis Research Society, we would call both of these curves Scoliosis even though the etiology, pathogenesis and pathomechanism are significantly different. Their clinical management is different as well.
The Objective ISM Examination in the Presence of a Structural or Apparent Spinal Asymmetry
In the Integrated Systems Model, the body is divided into three functional units to expedite the assessment. The driver(s) are found first in each functional unit and then the relationship, or priority, is determined between the drivers of the units. This process determines the relevance of any finding to the clinical picture (both the performance of the task and the patient’s experience is clinically relevant).
When spinal asymmetry is present, a full body assessment, whereby the body is divided based on each structural region that has formed based on the primary or secondary curves, is performed first to rule in/out a structural cause.
There are certain unilateral scoliosis patterns that help the clinician identify curve types. Idiopathic scoliosis has typical features that identify the curve pattern, as well as typical myofascial, neural, articular or visceral system impairments. Understanding which subjective, or objective, findings are the result of scoliosis can further help the clinician determine which findings are consistent or inconsistent with the scoliosis, and whether they are relevant, or irrelevant, to the meaningful complaint and meaningful task.
Patients can present with a very similar clinical appearance of their spine/posture whether they have structural or non-structural impairments. Clinically differentiating structural from non-structural asymmetry determines whether further medical imaging is necessary and guides management.
- Diane’s comment:
I have to interrupt this for a moment Judit because I know how very hard you have worked to bring clarity to this draft of your report. Our readers won’t have any idea how difficult it was to bring this clarity, for which I commend you – this is flowing beautifully!
We often say: just because you have disc herniation on your MRI, it doesn’t mean you must manage it, it is normal ‘wear and tear’. When a scoliosis is present (structural or non-structural), how do we know if it is ‘painful’ or ‘severe’ or ‘deformed’ enough to require treatment? When is a scoliosis specific exercise approach required? Clinically, in this author’s experience, there are no test-findings, or indicators, that suggest that an individual needs a uniquely tailored 12+ week long scoliosis specific exercise approach to manage their condition. Rather, further assessment is required to determine when, or if, the individual’s spinal asymmetry is relevant to their presenting complaint or a barrier to their functional goal (meaningful task).
Hodges et al (2016) notes:
‘… The ideal postural alignment is unlikely to be ideal for all individuals… It serves as a starting point for identification of features that can be evaluated for relevance to pain… If a feature of postural alignment is identified that deviates from ideal, it can be modified to assess the relationship to pain/muscle activation. If correction changes symptoms and/or reduces overactivity of muscles, then the feature is likely to be relevant to consider in planning of the [treatment program].’
This is applicable to all patients whether they have any diagnosis of spinal asymmetry, structural or non-structural.
According to Kim et al (2022) the spine and the body function within a cone of equilibrium with the focus of maintaining sagittal and coronal alignment with minimum energy expenditure. This happens with a harmonious relationship involving cervical lordosis, thoracic kyphosis, lumbar lordosis, and pelvic alignment. The purpose is to maintain a mechanical balance in the sagittal plane and coronal plane centered from the center of cranial mass, femoral heads, and lower extremities. It is also important to assess the impact of the transverse plane imbalance in both apparent and structural spinal asymmetries.
In Ms C’s subjective assessment the following findings suggested the need for a spinal asymmetry assessment:
- Her signs and symptoms were present since her juvenile or adolescent years,
- She reports feeling out of balance and states ‘her pants fit unevenly’,
- She reports noticing a rib hump,
- She reports difficulty with breathing.
This assessment will include analysis of her standing posture, a screening task for spinal asymmetry and a leg length discrepancy (LLD) assessment prior to a more regional ISM assessment.
Standing posture assessment
The quick observation of the standing posture is performed without LLD correction; the coronal, sagittal and transverse planes are analyzed.
Ms. C’s findings Fig. 5:
Coronal plane analysis
- Centre of Mass (COM) over the left foot
- Thorax lateral shift to the left over the pelvis
- Right foot lateral talar tilt
- Pelvic Obliquity: right iliac crest elevated relative to the left side
- Shoulder girdle asymmetry: right shoulder girdle depressed relative to the left side
Sagittal plane analysis
- Flattened lower Thoracic Kyphosis
- Hyperextended left knee
Transverse plane analysis
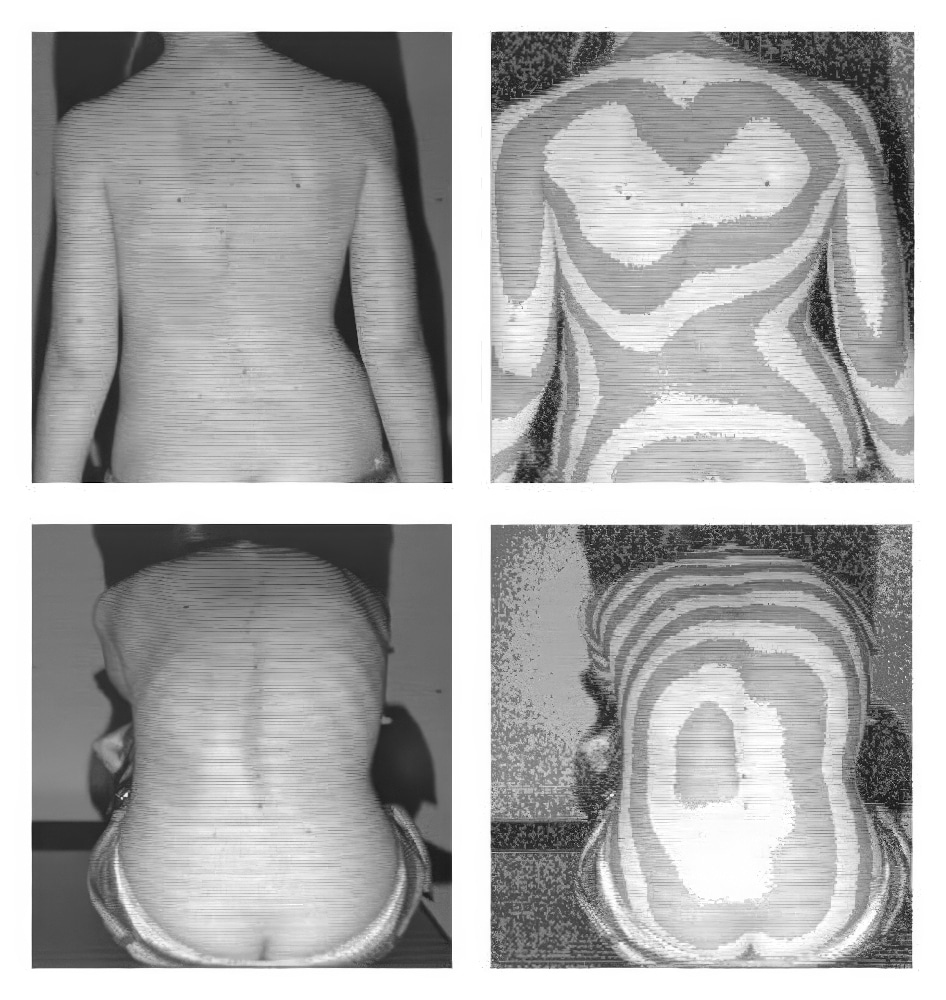
Observation of the transverse plane in standing is a key aspect of scoliosis screening, offering insights into the rotational biomechanics of the spinal axis. Visible features, such as spiral deviations observed with Moiré topography (Kotwicki et al 2007), guide further assessment:
- In the posterior view I observed minimal prominence of the Thorax on the right side and minimal to no flattening or a “sunken” appearance on the left side of the Thorax .
- Similarly, minimal asymmetry presented in scapular positioning, with the right scapula appearing minimally prominent compared to the left.
- Paraspinal musculature exhibits quite visible torsion, with hypertrophy and prominence on the left Lumbar region and a deep skin fold on the right Lumbar region.
- Pelvic asymmetry observed in the transverse plane: right transverse plane rotation.
Here is a picture from a research to show how Moire assessment shows transverse plane asymmetry:
Conclusion from the standing posture assessment
Analysis of Ms. C’s standing posture indicates that further screening is required for adult spinal asymmetry – a potential structural scoliosis.
Spinal asymmetry assessment
Ms C did not have previous X-ray imaging. It is fairly common in clinical practice that patients do not have medical imaging, or what they have is outdated, not meeting the standard criteria, or measured inaccurately. Measurements of coronal, sagittal and transverse plane imbalances were performed during a quick standing screen. The results were compared to normal physiological ranges to identify possible structural scoliosis.
Coronal plane analysis
Coronal plane imbalance is defined as a shift of the trunk in the coronal plane (Fig. 6). A neutral balance is identified if the midline of C7 (C7PL – C7 Plumb line) is no more than 20 mm laterally displaced in the coronal plane from the midline of the sacrum (central sacral vertical line (CSVL)).
A study by Fortin et al. in 2016 found an 85% prevalence of Coronal imbalance in Scoliosis, and a fair to moderate positive correlation between trunk imbalance and the Cobb angle.
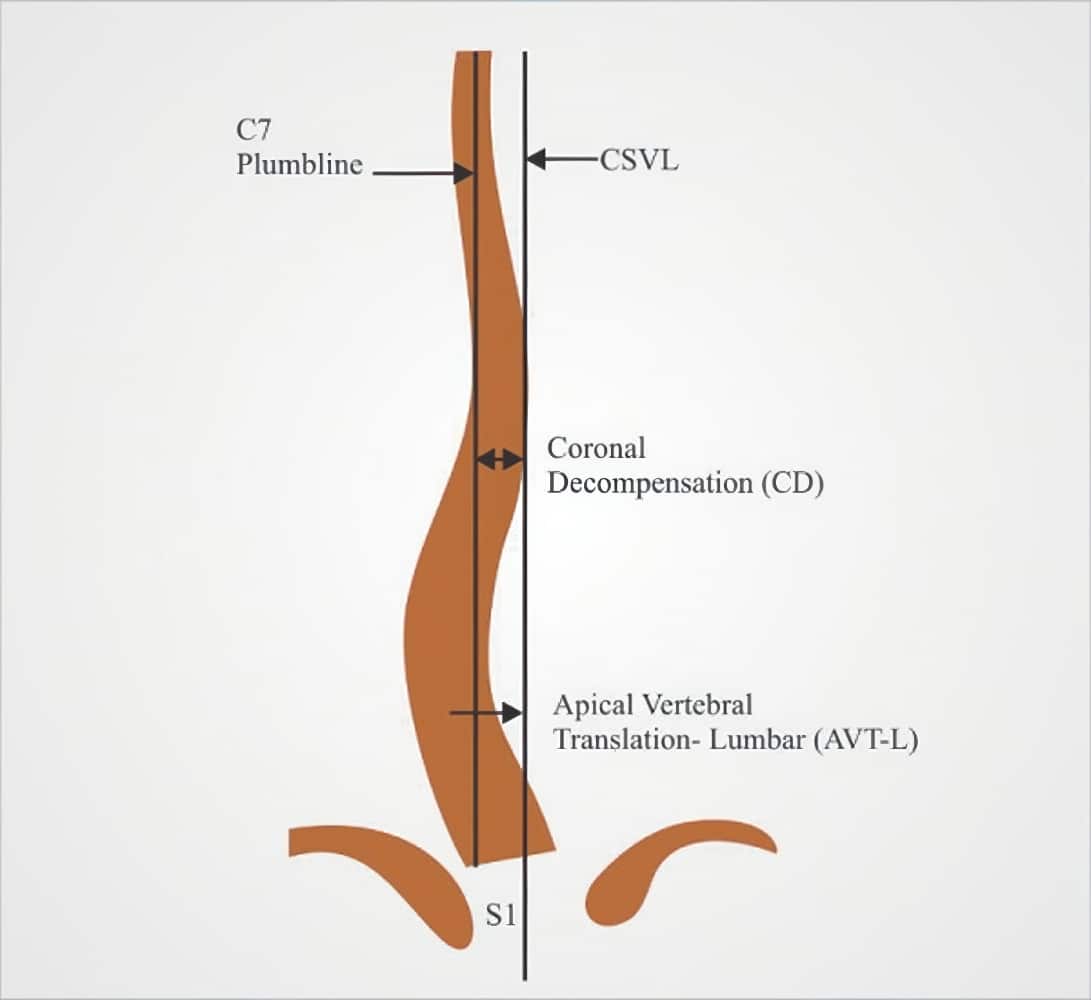
Ms. C’s coronal plane analysis revealed a left lateral displacement of C7 (C7PL) 25mm from the central sacral vertical line. This is an increase of 5 mm over the physiological range.
Sagittal plane analysis
Sagittal imbalance is another cornerstone in the diagnosis of adult degenerative scoliosis. This is measured globally on a full length, weight bearing, sagittal spine film with a plumb line dropped vertically from the center of the body of C7. The line should pass through the posterosuperior corner of the sacrum in ideally sagittal balanced individuals (Fig. 7).
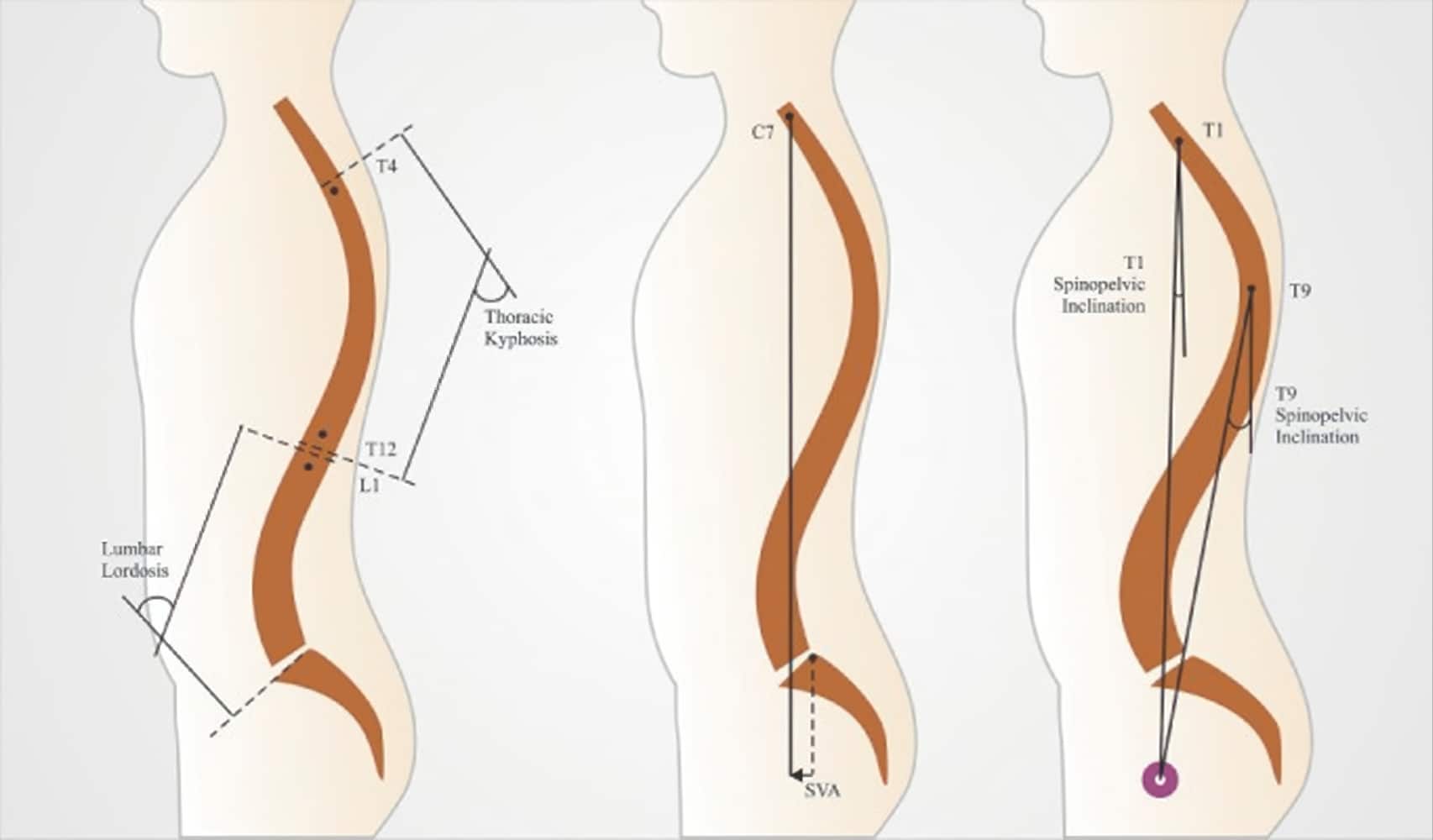
Sagittal Vertebral Axis (SVA) is the horizontal offset from a plumb line dropped from C7 to S1.
In a well aligned spine, the SVA plumb line falls behind or over the sacral endplate, normative range is between -60mm to +60mm. Since these measurements require medical imaging, it couldn’t be performed in Ms C’s case. A digital laser level can help get an approximate measurement where the clinician marks the approximate points where the SVA plumb line would fall, and was used to analyze Ms. C’s sagittal plane, and the line remained within the physiological range.
The sagittal spinal profile is often measured and calculated by the following values in Idiopathic Scoliosis measured on a plain radiograph. The most relevant (and applicable) sagittal parameters in outpatient clinical practice are lumbar lordosis, thoracic kyphosis; these can be measured with a digital inclinometer from the cranial and caudal vertebral bodies of each curve. Physiological Thoracic kyphosis is described as a Cobb angle between 20 – 40 degrees (some studies suggest 50 degrees) between T1-T12. Regarding the range of normality for the Lumbar Lordosis, the literature is extremely divergent, the most common values for a physiological lumbar lordosis range are found to vary from 26 degrees to 58 degrees Cobb-angle (Furlanetto et al. 2018).
Angles vary from one person to another, as each person’s lordosis is based on the relationship between their spine and their pelvis, a measurement called pelvic incidence. Lumbar lordosis should match the pelvic incidence +/- 10 degrees.
Ms. C’s measurements:
- Thoracic regional angle for kyphosis: T1+T12: 37 degrees – within physiological range
- Lumbar regional angles for lordosis: L1+S1: 35 degrees – within physiological range
Transverse plane analysis
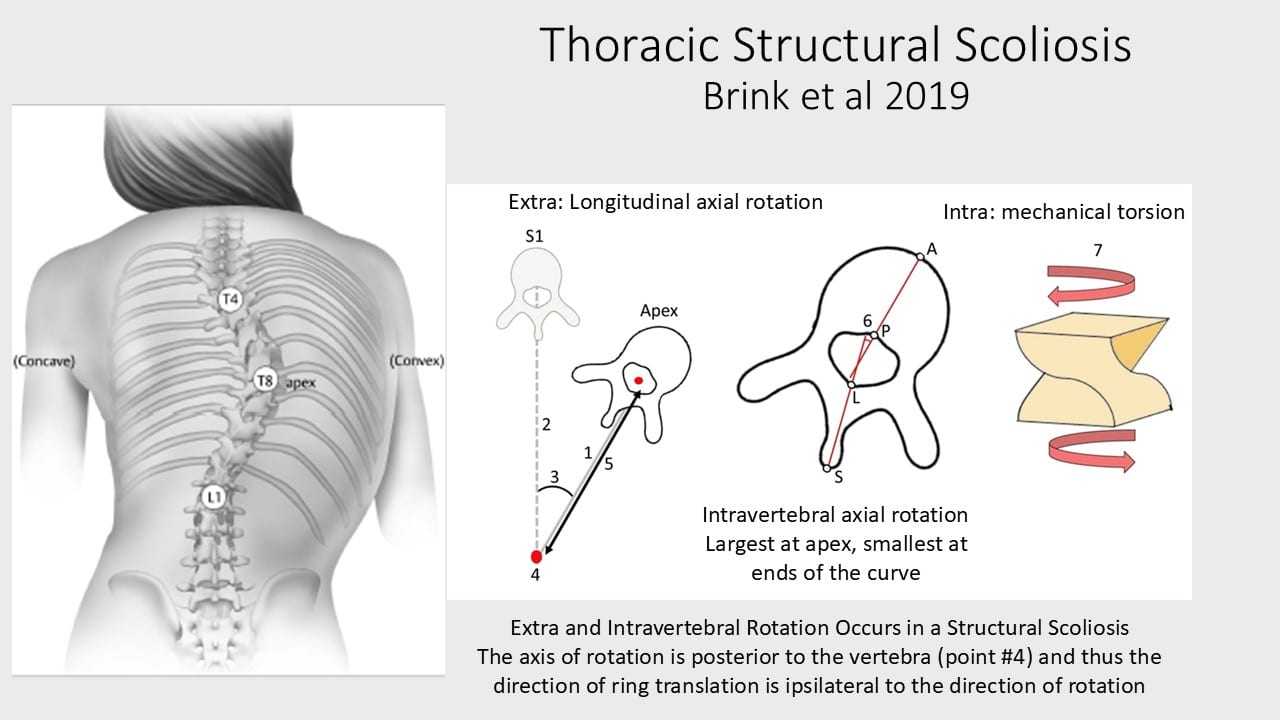
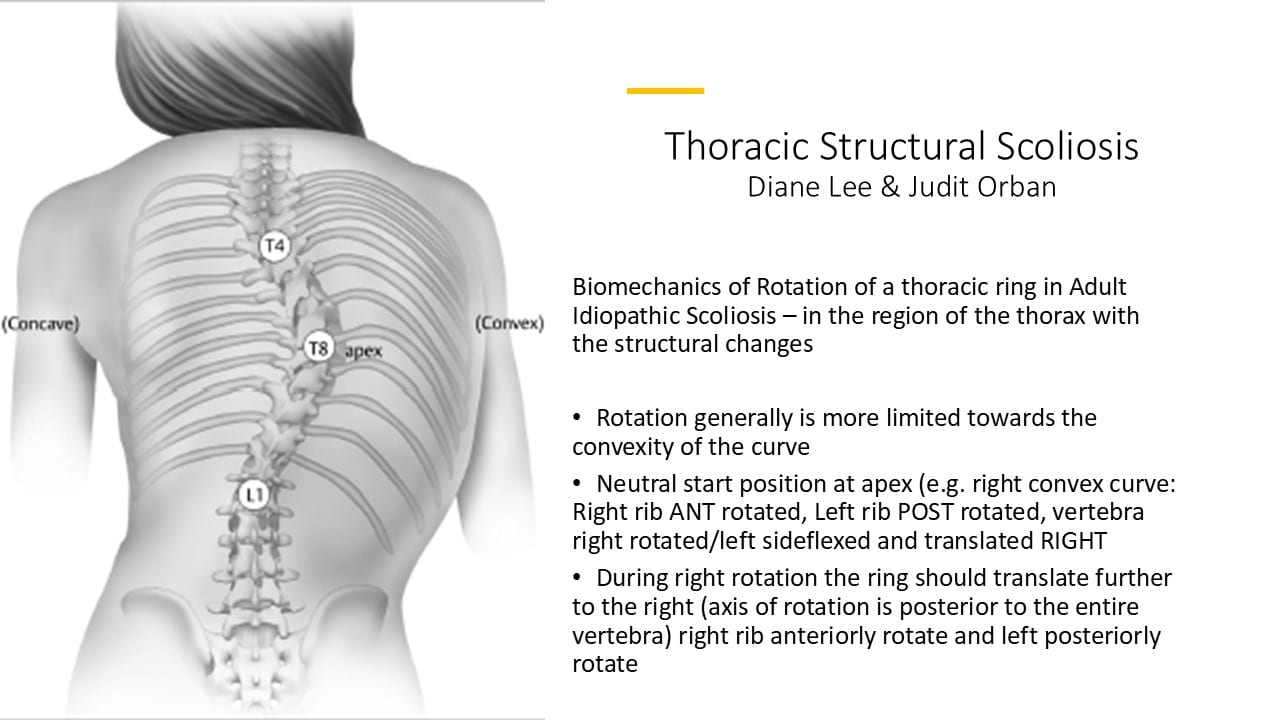
The non-scoliotic spine is only slightly rotated in the axial plane, is coronally aligned without a curvature, and shows mild kyphotic (thoracic and sacral regions) and lordotic (cervical and lumbar regions) curvatures. In structural (idiopathic) scoliosis, in addition to intra-vertebral torsion, each vertebra in the curve rotates, and translates, away from its midline position (the axis of this rotation is posterior to the spinous process of the vertebra) (Brink et al 2019).
While the radiographic measurement of the Cobb angle is considered the gold standard for scoliosis diagnosis, various trunk surface metrics can be used for objective assessment of any spinal deformity. Traditionally, scoliosis screening in an outpatient practice is performed using a scoliometer in the standing forward bending position (Adam’s Forward Bending Test). The scoliometer measures the Angle of Trunk Rotation (ATR) in the transverse plane.
Bunnell defined the following screening cut-off criteria:
- the trunk rotation is within normal limits: ATR from 0° to 3°,
- the trunk rotation is intermediate: ATR from 4° to 6°,
- the trunk rotation is relevant and it is highly probable for scoliosis: ATR ≥ 7°.
Scoliometer examination has shown good repeatability and reproducibility. For the cut-off value of the ATR equal to or greater than 7° the scoliometer examination is characterized by high sensitivity (83.3%) and high specificity (86.8%). Although the Bunnell criteria is designed for the skeletally immature spine, we can still use the measurements for screening the adult spine.
A standing scoliosis posture screen can help determine the presence or absence of any apparent or structural spinal asymmetry, but does not replace a thorough clinical examination. An ATR above 7 degrees can also be found in apparent spinal asymmetries. Further clinical tests are required to differentiate the two categories of scoliosis.
Ms. C’s findings using the Bunnell Scoliometer were as follows:
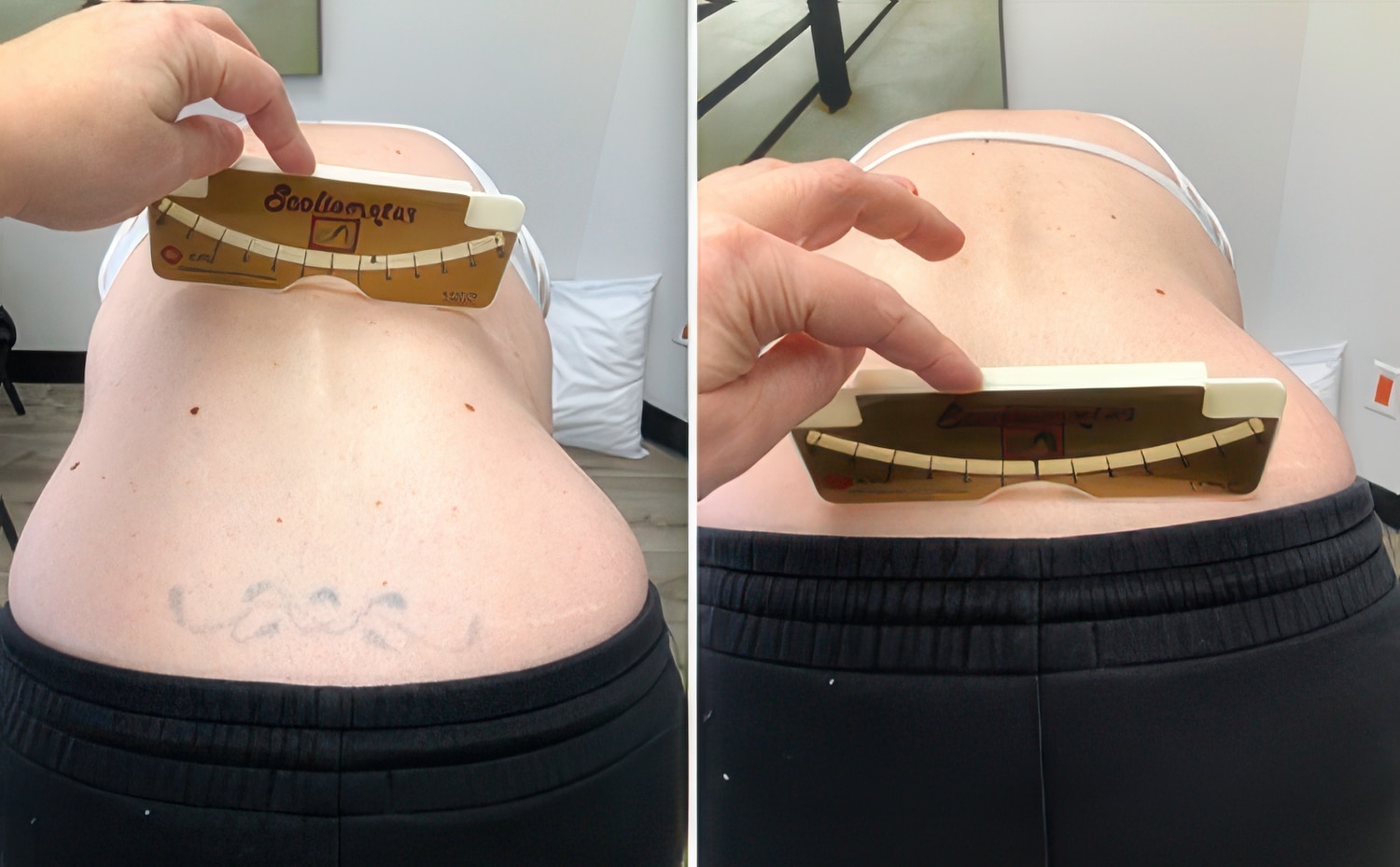
Standing forward bending (Fig. 8) – angle of trunk rotation measured at the apex of each regional curve
Thoracic spine: 0.5° to the right
Lumbar spine: 10° to the left
Pelvis: 5° to the right
Sitting forward bending (Fig. 9) – angle of trunk rotation measured at the apex of each regional curve
Thoracic spine: 0.5° to the right
Lumbar spine: 5° to the left
Pelvis: 9° to the right
Conclusion from the spinal asymmetry assessment
Although scoliosis screening is typically performed in the standing forward bending position, studies have shown that seated measurements provide the same clinical results. In Ms. C’s case there is a discrepancy between the standing and sitting angle of trunk rotation (ATR) measurements in the lumbar and pelvic regions and these findings are inconsistent with structural (idiopathic) scoliosis:
- The lumbar ATR improves in sitting. It would be expected to remain the same if a structural scoliosis was present.
- The pelvic ATR worsens in sitting. It would be expected to remain the same or improve due to the stable platform if a structural scoliosis was present.
These findings indicate the Ms. C has a non-structural spinal asymmetry. Furthermore, during the standing forward bending test further observation of the lumbar spine from the sagittal view revealed no signs of ‘flattening’, or extension, of the area of peak axial rotation in the lumbar spine, and this is another indication of an apparent spinal asymmetry.
Further screening is necessary to determine if ISM can determine whether suboptimal alignment, biomechanics, and/or control of the thoracolumbar spine and pelvis are responsible for the noted regional rotations and deviations in the transverse and coronal planes and/or whether a structural leg length discrepancy (LLD) plays role in this patient’s clinical findings. Factors from the story suggest further screening for a leg length discrepancy is warranted.
- Diane’s question:
I’m loving how all these assessment models are coming together here Judit! Since a leg length correction would also be considered a correction in ISM, why do you think it is necessary to separate a LLD model of assessment from simply correcting the leg length in an ISM approach to assessment?
- Judit’s response:
I consider structural, true leg length discrepancy as a ‘deformity’ and by adulthood patients have learned to live with compensatory mechanisms that are secondary to the LLD. Are we treating the deformity or the compensatory mechanism or both? Is this deformity related to the meaningful complaint or to the meaningful task? It needs to be assessed.
We can have completely different ISM assessment findings with and without leg length corrections, negative and positive impact on the meaningful complaint; and it can improve or worsen the meaningful task. Therefore, a separate model of assessment is required to collect more information.
Leg length discrepancy (LLD) assessment
The initial standing posture screen revealed visible pelvic obliquity (a strong indication of LLD) and measurements from the Adam’s Forward Bending Test were inconsistent with idiopathic structural scoliosis and certain subjective factors (ill-fitting pants, feeling lopsided since childhood) indicate that an assessment of the limb length was warranted. Approximately 90% of the population has a limb length discrepancy of less than 10 mm (1.0 cm). Current research supports that ‘discrepancies greater than 10 mm are clinically significant, and can alter biomechanics and result in functional limitations, such as gait, posture, and balance problems, as well as musculoskeletal disorders, such as lower back pain, scoliosis, and degenerative spinal changes’ (Applebaum et al. 2020).
In the following section, a series of combined limb length measurements and repeated scoliosis screening tasks were performed to verify if an uneven limb was playing a role in Ms. C’s spinal asymmetry, or if a combination of LLD and a compensatory, or apparent, scoliosis could be identified. There are multiple accurate, and reliable, clinical and imaging modalities for quantifying leg-length discrepancy (LLD).
Supine analysis of leg length
In a supine position, the distance between the anterior superior iliac spine (ASIS) and the medial malleoli is measured using a tape measure. In Ms. C’s case, approximately 10 mm discrepancy was measured, with the left leg being shorter than the right. Femoral bone length was also compared in supine position with the hips and knees at 90 degrees of flexion. The left knee appeared to be lower than the right knee.
These findings are congruent with the direction of her pelvic obliquity: right iliac crest higher than the left.
Standing analysis of leg length
In the standing position, there were multiple coronal plane imbalances that previously indicated a potential leg length discrepancy. Therefore, a quick screening approach was used where a 9 mm heel lift was placed under the left lower limb and the following changes were observed in the standing posture screen. (The reason for using a 9 mm and not a 10 mm heel lift: the standard heel lifts at our clinic are 6 mm and 9 mm, provided by the Pedorthist).
- Improved C7PL to CSVL: close to 0 cm (25mm deviation of C7 without leg length correction)
- Improved Pelvic Obliquity: level of the iliac crests close to even
- Improved alignment of right foot: no more lateral talar tilt
- Improved alignment of the lumbar spine in the coronal plane
- Worsened thorax alignment in the transverse plane: the whole thorax is slightly left rotated
Repeated spinal asymmetry assessment with LLD correction
Adams standing forward bending test with 9 mm heel lift under the left leg
Angle of trunk rotation measured at the apex of each regional curve (Fig. 10)
Thoracic spine: 0.5° to the right – no change in ATR
Lumbar spine: changed from 10° to 7.5° to the left – minimal improvement in ATR with LLD correction
Pelvis: changed from 5° to the right to 0° – neutral ATR with LLD correction
- Diane’s question:
What is your interpretation of this lack of change in thoracic rotation?
- Judit’s response:
I suspect a possible strong articular vector was present and thus limited the physiological adaptability in the mid-thoracic region.
- Diane’s question:
The lumbar region ATR with the LLD corrected is still greater than the guidelines for diagnosis of a structural spinal asymmetry. What cluster of findings at this point rule in, or out, a diagnosis of structural spinal asymmetry in the lumbar region?
- Judit’s response:
The main thought from my clinical findings is that correcting the leg length has a positive impact on the pelvis and no worsening of the lumbar spine. In idiopathic structural scoliosis, correcting leg length unnecessarily may improve the pelvis but commonly worsens the key measurements in all 3 anatomical planes, especially the lumbar regional transverse plane rotation. Having a slight positive impact on the lumbar spine rules in LLD diagnosis.
It is also important to mention the client’s experience with the 9 mm LLD correction. She felt positive, more balanced, and not leaning to the left. However, after a short period of standing, Ms. C reported that her thorax (chest) suddenly felt tighter and in my observation her thorax started to translate to the right in the coronal plane.
- Diane’s question:
So, in conclusion, would you say her experience was positive or negative and what objective finding do you think is driving this experience response?
- Judit’s response:
Her initial reaction is positive for certain body regions, (ankle, hip, pelvis) and then the delayed response in the thorax is negative, which is also reflected by the objective findings as well (observed right translation of the thorax in the frontal plane). This might suggest that multiple regions are in relationship to each other, or are co-drivers.
- Diane’s comment:
Here is where I think ISM provides a biologically, plausible hypothesis for this finding and experience. I don’t think the LLD is the primary driver since this correction worsened the alignment of her thorax as well as her experience. I would suggest that there is likely a region in the thorax that is incapable of adapting to this correction, and the alignment of one or more thoracic rings worsened with this correction. While a LLD correction is required, her body is telling you to not do this first – there is something in the thorax that requires treatment before prescribing the heel lift.
Correcting the left leg length with an approximately 9 mm heel lift created the following changes in the observed sitting posture (Fig. 11):
- The coronal plane analysis revealed a sudden change in the previously left lateral displacement of C7 (C7PL) 25mm from the central sacral vertical line (CSVL); becoming
- right lateral displacement of C7PL 20 mm from the CSVL
- Diane’s comment:
this is a reflection of the increased lateral translation of the thorax to the right
- Improved Pelvic Obliquity: level of the iliac crests are even
- Diane’s comment:
this is a reflection that the cause of the pelvic obliquity in standing was coming from below and not above the pelvis.
Starting from a standing position with 9 mm heel lift under the left leg
Angle of trunk rotation measured at the apex of each regional curve (Fig. 12)
Thoracic spine: 0.5° to the right – no change in ATR
Lumbar spine: changed from 5° to 2° to the left – improvement in ATR with LLD correction
Pelvis: changed from 9° to 6° to the right – improvement in ATR with LLD correction

Conclusion from the leg length discrepancy assessment
For Ms. C, the 9 mm heel lift under the left leg corrected the pelvic inclination, and improved the lumbar spine transverse plane rotation. This phenomena suggests that the noted spinal asymmetry might be apparent and not structural. Her leg length discrepancy assessment suggests she has a shorter left leg of approximately 10 mm. This LLD has likely been present since her juvenile or adolescent years, as suggested by her story. Ms. C’s LLD has potentially led to long-term compensatory mechanisms impacting her posture and multiple regions of her body..
I suspect an acquired or secondary Scoliosis due a prolonged period of asymmetrical alignment from having leg length discrepancy. The apparent spinal curve had most likely developed during the rapid growth spurt of adolescence or even juvenile years. The angles of trunk rotation in the thoracic spine did not change between standing forward bending without or with the LLD corrected or sitting; however, the LLD correction resulted in a right translation of the entire thorax and the client’s experience although initially was positive, it then quickly changed to negative (tightening of her chest). This suggests that the thorax is not able to adapt to the LLD correction and that further assessment of the thorax is necessary.
- Diane’s comment:
ISM will also provide the order of these interventions, when to do what for the best client experience and outcome.
Continued Regional Assessment - The Integrated Systems Model
Task Analysis – Squat without LLD correction
Functional Unit #1 (FU#1): TR3 to hips
Standing Start Screen Findings – without LLD correction
Pelvis: Rotated to the right in the transverse plane (RTPR). The pelvis was also laterally tilted to the left; the right iliac crest was elevated relative to the left. With 50% of the body weight through either leg, the SIJs were controlled; therefore, in standing her pelvis presents with a congruent right intrapelvic torsion (IPT).
- Diane’s question:
Is there another test with movement that would confirm the position of the left and right innominates being congruent with the direction of the pelvis TPR?
- Judit’s response:
In a standing position the therapist stands behind the client and palpates the left and right innominates (finger tips palpating the anterior aspect of the innominates; palms are resting along the iliac crests and soft tissues on either side). In this resting position the innominates should not be rotated relative to one another, and the sacrum should not be rotated either.
In Ms C’s case, since the left hand is more forward relative to the right, it indicates that the pelvis is in a right transverse plane rotation. Applying a gentle corrective movement into the neutral position of the pelvis where there is no transverse plane rotation, followed by a slow release and listen, or feel, where the innominates reposition themselves, can help the therapist confirm that the left innominate is rotating anteriorly relative to the right innominate; and this rotation is congruent with the transverse plane rotation.
The sacrum is rotated to the right with both left and right sides of the sacrum nutating relative to the respective innominates.
- Diane’s comment:
Yes, using movement to feel where the innominate returns to after releasing the correction, the test finding either validates, or negates the positional hypothesis.
Hips: Left hip was anterior relative to the right hip, congruent to the positional finding of the pelvis (right TPR). The right hip was also slightly anterior relative to the right acetabulum.
- Diane’s question:
What is the significance of noting the position of the femoral head to its own acetabulum?
- Judit’s response:
In neutral standing, the femoral head should be centered in the acetabulum, with equal tension in the front and back of the hip. When the femoral head is anterior relative to its own acetabulum, it indicates muscular imbalances.
- Diane’s comment:
Not quite Judit. In order for the femoral head to translate further anterior to the acetabulum (shear) there has to be some articular laxity of the anterior capsule, ligaments and labrum.
- Judit’s response:
Understood. The anterior translation of the femoral head relative to the acetabulum indicates more than a simple positional or functional finding; it reflects an underlying joint dysfunction, likely involving laxity of the anterior capsule, ligaments, or labrum. This dysfunction predisposes the joint to increased mechanical stress, potentially accelerating degenerative changes over time.
Thorax: The entire thorax was rotated to the right.
- Diane’s question:
Which way was the thorax translated generally with this entire right rotation?
- Judit’s response:
Looking at the middle picture in Figure 13, the thorax appears to be generally translated left, consistent with multiple thoracic rings being rotated to the right in a non-structural scoliosis.

- Diane’s comment & question:
By definition a glued ring means that two adjacent thoracic rings are incapable of independent movement and that correction of one worsens the other. When you say ‘the 5th thoracic ring is ‘stuck, stiff and doesn’t move’ when you attempt to align, or correct, the 6th thoracic ring, did the alignment in space of the 5th thoracic ring worsen?
- Judit’s response:
Yes, attempting to correct the 6th thoracic ring did not improve, yet slightly worsened the 5th thoracic ring.
The alignment of the 5th thoracic ring was incongruent to the positional finding of the pelvis (right TPR).
Lumbar spine: The entire Lumbar spine is left rotated and left translated in standing.
Although it appears that this patient doesn’t have structural, idiopathic scoliosis; her lumbar region still appears to be translated to the left and rotated to the left.
- Diane’s question:
What do you understand to be the normal combined biomechanics of translation and rotation of a lumbar segment? I need to look up Bogduk’s work for this but I think when the sagittal part of the right Z joint impacts during left rotation, it creates an axis of rotation around the right facet which is now posterior to the IVD and the translation of the vertebral body should be to the left. I could be wrong though – I need to look it up!
- Judit’s response:
During axial rotation, the lumbar vertebrae exhibit coupled movements involving both rotation and lateral translation. When the spine rotates to the left, the right (contralateral) zygapophyseal (facet) joint experiences increased compressive forces, while the left (ipsilateral) facet joint undergoes distraction. This interaction creates an axis of rotation near the contralateral facet joint, leading to a leftward translation of the vertebral body. Bogduk 1986, Basques 2017.
Screening Task Findings – Squat task without LLD correction
Pelvis: Remained rotated to the right in the transverse plane (TPR) and right iliac crest remained elevated as well – slightly worsens during the task. Both sacroiliac joints lose control during the task: left side early, at the beginning of task.
Hips: The right femoral head (hip) was delayed in centering during the task, but was able to center later in the task. The left hip remained anterior relative to the right hip during the task – did not center – and additionally it abducts and further externally rotates.
- Diane’s comment:
So here is the finding that is consistent with her report of her hip being in external rotation when she sits on her horse. Do you think this could be related to the pelvic obliquity? I suppose we will find out when you correct the LLD!
- Judit’s response:
Yes, I believe that the laterally tilted pelvis, coupled with the left femoral head being externally rotated, is a compensation for the LLD.
- Diane’s comment:
The RTPR of her pelvis could result in more external rotation of the left hip, regardless of the lateral tilt, especially if the saddle forces her to sit in a more neutral position and not a RTPR.
- Judit’s comment:
thank you for clarifying this.
Thorax: The thoracic region appeared to improve in the squat, the general right transverse plane rotation of the entire thorax corrects. However, within this total right TPR of the thorax, the 5th thoracic ring further translated right/rotated left.
- Diane’s question:
You mention above that the 5th and 6th thoracic rings are partially glued. What happened to the 6th thoracic ring (TR6) in the task?
- Judit’s response:
The 6th thoracic ring slightly worsened by being further translated to the left, not as significant as the 5th
Lumbar spine: The Lumbar spine rotated and translated further to the left during the squat task.
- Diane’s question:
Can you tell me specifically what happened to L5 and not regionally to the lumbar spine. The pelvis remained in a RTPR and the left lateral tilt increased. What would the congruent response be for L5 to this keeping in mind not only the rotation of the left and right innominate bones, but also the position of the left and right sides of the sacrum when the SIJs unlock?
- Judit’s response:
he coupled motion of L5 on S1 is an ipsilateral rotation versus lateral flexion. In standing the sacrum is right rotated with the pelvis in right transverse plane rotation. L5 is left rotated, therefore it is in a right lateral flexion relative to S1. So there are regional differences during the squat task and the above statement is not true for the entire Lumbar region.
During the squat task the sacrum should remain in its nutated position, relative to the innominates. The two bones should move as a unit, but in Ms. C’s case both innominates rotate anteriorly, the left innominate early, at the beginning of the task. Since the pelvis remains in right transverse plane rotation, my explanation for this would be that the sacrum is rotating left during the squat task (this should have been assessed).
- Diane’s comment:
We can only hypothesize at this point, reflection is always fun in ISM certification! However, consider this. When the sacrum rotates to the right as part of the pelvic ring TPR, regardless of what the ipsilateral innominates are doing relative to the sacrum, its axis is oblique and a contralateral sideflexion occurs. So, in space, the sacrum in a RTPR and is RR/LSF. L5 should follow the rotation of the sacrum and RR/RSF at the zygapophyseal joints – this is a congruent pattern. The sacrum sideflexes left and glides superiorly up the right facet of L5, L5 RR/RSF and glides inferiorly down the right facet – there is no conflict, or incongruence here. However, Ms C’s pattern is NOT this! If her sacrum RR/LSF and her L5 LR/LSF, then the sideflexion is congruent but the rotation is not. This could potentially create a lot of torsion of the L5-S1 disc and compression of the right L5-S1 zygapophyseal joint.
- Judit’s response:
Thank you for clarifying this Diane! Love your thought pattern leading to the torsion of L5-S1 disc and compression of the right L5/S1 zygapophyseal joint.
Impact of Corrections – without LLD correction
Corrections were applied to understand the relationships between the impaired body regions, before checking the impact of LLD.
Impact of correcting the pelvis: No change in the hips and lumbar spine. The mid and upper thorax alignment worsened (translated laterally to the right and rotated left). The 5th and 6th Thoracic rings remain partially glued.
- Diane’s question:
So why didn’t this increase in the left rotation show up in the Adam’s forward bending test? Can you give me more information specifically about what happened to TR 5 & 6 in this task other than remaining partially glued. TR5 started in right translation/left rotation and this increased in the screening task. What did correcting the TPR of the pelvis and providing force closure to control the unlocking SIJs (and I would have corrected the pelvic obliquity as well as this would have been a more complete pelvic correction rather than correct the LLD independently) do to the alignment of TR5 and 6? Also, please let us know what her experience was with this correction since drivers are not only about biomechanical improvements but also improved client experience of the task. Also, what made you decide to start with a pelvic correction and not the thorax or hips?
- Judit’s response:
The Adam’s forward bending test shows the regional rotation due to structural, vertebral changes; it is not tested for individual segmental rotation related to non-structural vertebral changes. The scoliosis screening task is a forward bending task, and right now I am correcting the pelvis in standing, therefore it is a different task.
- Diane’s comment:
Perfect answer!! Strategies are task specific!
- Judit’s further response:
To provide more information on the 5th and 6th thoracic rings: the 5th thoracic ring started in right translation/left rotation and the lateral translation/rotation further increased relative to the upper and mid thoracic rings above and below. The 6th thoracic ring started in left translation/right rotation and remained incongruent relative to the upper and mid thoracic rings. It translated to the right as a ‘block’ with the upper and mid thoracic rings.
- Diane’s comment:
This is because TR6 is not capable of independent movement from TR5 (it is glued); therefore when TR5 translated further right, it took TR6 with it.
- Judit’s further response:
I decided to start with the pelvis due to the multiplanar and significant findings: I tried correcting the obliquity first but the client responded by lifting the left heel matching the new, level innominates. The pelvis was not capable of isolated correction of the obliquity from the lower extremity.
Client’s noted being ‘lopsided’ to the left without any additional discomfort.
Impact of correcting the hips: Correcting the left femoral head (centering it in the left acetabulum) provided no change in the Thoracic and Lumbar regions. The pelvis worsened with further right TPR. Client reported no specific change to her sensorial experience.
- Diane’s comment:
So even though the start screen findings suggest that the pelvis and hips are following one another, they are NOT. If they were, correcting one would change the other. Here, neither resulted in a positive response in the other. This suggests there are at least two drivers.
Impact of correcting the thorax: It was not possible to fully correct the thorax due to the partially glued thoracic rings 5 and 6. A co-correction of TR5 and TR6 resulted in full correction of TR6 and a partial correction of TR5. However, this co-correction resulted in minimal improvement in the transverse plane rotation of the pelvis; however, no improvement in control of either sacroiliac joints. No change was noted in the Lumbar region (L5) or the hips. The client noted worsening of her symptoms during the Thorax correction and no impact with the pelvis or hip corrections.
Impact of correcting the Lumbar spine: A scoliosis specific, active self correction was applied to correct the entire Lumbar spine, and the entire Lumbar region alignment improved by partially deflecting and derotating towards the center. L5 remained in the left rotated position. The mid and upper thorax alignment worsened (translated laterally to the right and rotated left). The 5th and 6th Thoracic rings remain partially glued. Client reported positive sensorial experience in the lower back (less painful).
- Diane’s question:
What do you mean by ‘deflecting’ – that’s a new word for me!
- Judit’s response:
In “scoliosis jargon” deflexion and derotation are used when a curve appears to ‘straighten’ in the coronal plane and then improve in the axial plane.
- Diane’s comment:
Ah – every approach has its own language.
Summary of FU#1 drivers
There are 4 regional drivers in FU#1 to pay attention to moving on: Pelvis (bilateral unlocking sacroiliac joints), Left Hip (failed to center), Thorax with priority rings TR5 and TR6 and Lumbar (L5 remained left rotated).
Note to reader: these corrections are without LLD correction, we would expect changes with LLD correction.
- Diane’s comment:
We can have all the expectations (or cognitive biases) we want as long as we remember to test them – this is ISM!
From the patient’s story a possible structural leg length discrepancy suggests further assessment of the lower extremity (FU#3) is warranted. However, given her history of multiple concussions and head trauma, a quick screen to confirm/negate whether an assessment of FU#2 was warranted first.
Functional Unit #2 (FU#2) – Quick Screen
A quick screen task of head and neck rotation bilaterally was performed to confirm that corrections of the drivers in FU#1 did not create any worsening of symptoms or performance of FU#2.
- Diane’s question:
Did you do this quick screen task in standing or in the squat position? It is best done in the screening task since vectors of restriction impacting head and neck function may only show up once in the task position.
- Judit’s response:
I did it in both the standing and squat screening task.
Client presents with effortless head and neck rotation when partially correcting the Thorax drivers (TR 5 & 6) and her experience is neutral. The same findings are reported in both standing and the squat task.
Functional Unit #3 – Lower Extremities
Standing Start Screen Findings – without LLD correction
Left lower limb: shorter than right
Right hindfoot: right lateral talar tilt
Knees: not assessed at this time
Screening Task Findings – Squat without LLD correction
Left lower limb: Left foot worsens: talus supinates during the squat task.
Right hindfoot: The right talus can’t pronate during squat, tilts laterally further and the calcaneus moves into valgus position (calcaneovalgus)
Right mid and forefoot: restricted in fanning during squat
Knee: not assessed at this time
- Diane’s question:
Optimally, the hindfoot should pronate when moving from the standing position to the squat. Neither hindfoot is doing this. Can you describe for me the optimal osteokinematics of the talus and calcaneus during pronation (ala ISM) and how your findings for each foot differ from these optimal biomechanics?
- Judit’s response:
In relaxed standing, the talus should rest on top of the calcaneus with the foot neither supinated nor pronated. During a squat, the talocrural joint should dorsiflex relative to the mortise; the hindfoot should pronate. As part of pronation, the calcaneus rotates in the transverse plane about an oblique axis such that the anterior part goes lateral and the posterior part goes posteromedial, relative to the talus. The talus plantarflexes and moves medially and inferiorly relative to the calcaneus (medially rotates).
In Ms C’s case, her right talus is already in a medially rotated position relative to the calcaneus. Relative to the mortice, the talus is laterally tilted. The talus is essentially locked in this position, the tilt prevents the tibia and fibula from advancing over the talus and the talus cannot medially rotate relative to the calcaneus because it is already there. The only motion available during the squat is more tilting of the entire hindfoot relative to the lower leg.
Her left talus and calcaneus starts in an optimal, stacked position, but during the squat task the calcaneus rotates in the transverse plane about an oblique axis such that the anterior part goes medial and the posterior part goes anterolateral relative to the talus. The talus dorsiflexes and move superior and lateral relative to the calcaneus (laterally rotates).
- Diane’s question:
Her pelvis is in a RTPR and remains there during the squat. What would the congruent pattern for both the left and right foot be and is Ms. C’s performance congruent or incongruent?
- Judit’s response:
If an individual’s pelvis is in RTPT, then both left and right foot go into dorsiflexion; pronation occurs in the left foot, but in order to accommodate the pelvis remaining in RTPT the right foot would supinate. Ms. C’s performance is incongruent to accommodate for the leg length discrepancy.
Impact of Corrections in FU#3
Right hindfoot:
Left leg length discrepancy – impact of a 9mm heel lift left: The left heel lift corrected the right hindfoot lateral talar tilt in standing. In the squat task this correction resulted in pronation of the right hindfoot and no calcaneovalgus. The right mid and forefoot pronation (fanning) also improved during the squat task. The client’s experience: The legs feel balanced for both the standing and squat task.
- Diane’s question:
With the leg length changed, was the left foot then able to also pronate as it should?
- Judit’s response:
Yes, the left foot was able to pronate during the squat task following the introduction of the 9mm heel lift to address the leg length discrepancy. However, the pronation was not optimally controlled by the intrinsic and extrinsic foot musculature. During descent into the squat, the left calcaneus demonstrated excessive eversion and abduction relative to the talus, suggesting a lack of coordinated eccentric control from the tibialis posterior, peroneus longus, and the intrinsic stabilizers of the medial longitudinal arch. Additionally, the talus exhibited excessive medial translation and plantarflexion without adequate containment within the mortise, indicating insufficient neuromuscular regulation of hindfoot motion.
To optimize talar positioning and enhance foot stability throughout the squat, I applied taping to reinforce medial arch support and facilitate a more optimal talonavicular alignment. This intervention aimed to externally constrain excessive motion, providing proprioceptive input to facilitate co-contraction of the intrinsic stabilizers while promoting a controlled pronation pattern. With this support, the left foot exhibited a more biomechanically efficient pronation response, allowing for improved force attenuation and weight distribution during the squat task.
Summary of FU#3 driver
The short left limb is the primary driver in FU#3.
Relationship between FU#1 and FU#3 drivers for Standing & Squat Tasks
In an ISM assessment, the next step is to prioritize the individual unit drivers; in this case the 4 drivers in
FU#1: Thorax (TR5 & 6), Lumbar (L5), Pelvis (bilateral SIJ control and RTPR), Left Hip and 1 driver in
FU#3: left limb (short 10mm).
Correcting the FU#3 driver (left lower extremity LLD) had the following impact in the drivers in FU#1:
Pelvis: The Pelvis obliquity (lateral tilt) resolved in standing when the FU#3 driver was corrected (left lower extremity LLD). The pelvis remained in a right transverse plane rotation/IPT.
- Diane’s question:
What happened to control in the squat task?
- Judit’s response:
I found this in my old notes from 2023: ‘…correcting the Thorax restored LSIJ control and the LLD + right foot correction restored R SIJ control for the squat task.’
So at this point both sacroiliac joints lose control during the task: left side early, at the beginning of task. Later resolved by correcting FU#1 and FU#3.
Left Hip: The left hip centered in the acetabulum in standing when the FU#3 driver was corrected; however, the left femoral head remained anterior relative to the right femoral head congruent with the RTPR of the pelvis. During the squat task with the LLD corrected, both femoral heads remained centered in the acetabulum with the left femoral head being less anterior to the right as the RTPR of the pelvis improved during the descent of the squat. When returning to, the pelvis rotated to the right and then the left hip moved anterior to the right.
Lumbar (L5): The lumbar spine minimally improved with correction of the FU#3 driver; less transverse plane rotation was observed in standing. During the squat task with the LLD corrected, the entire Lumbar spine was translated further to the left and rotated more to the left.
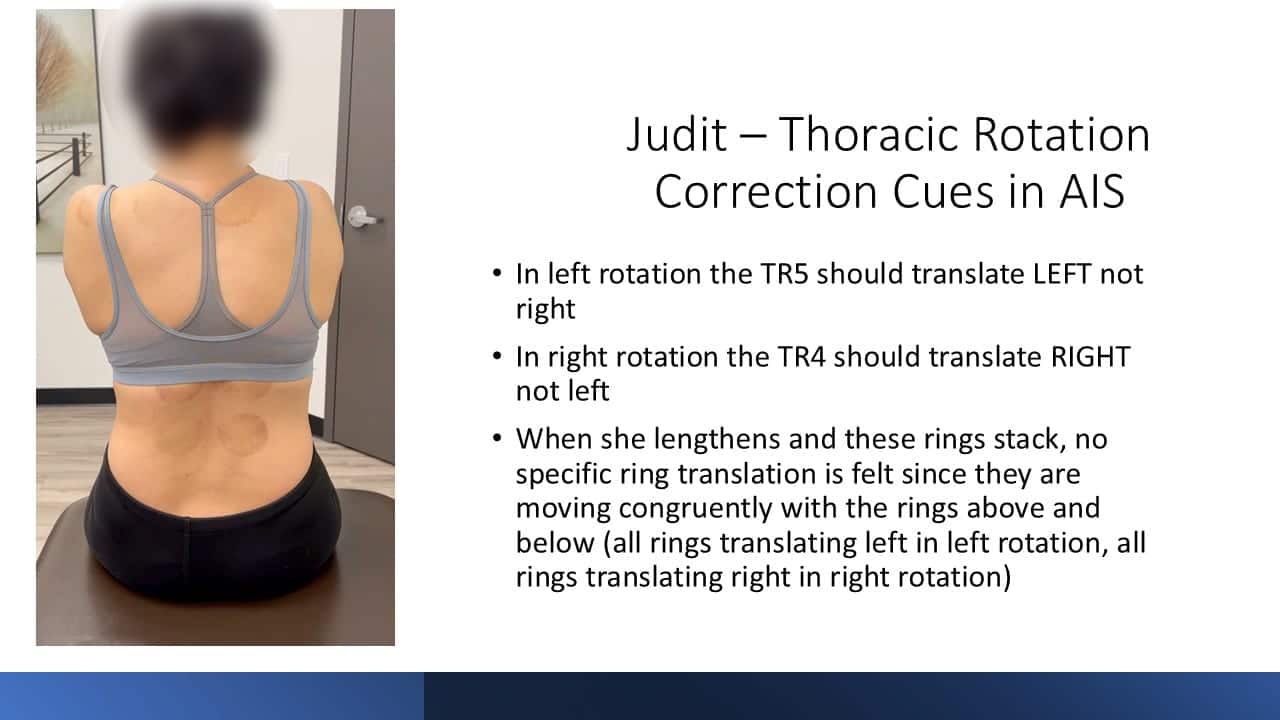
Thorax (TR5 & 6): During the squat task with the LLD corrected, the 5th and 6th Thoracic rings remain partially glued, the upper and middle thorax again translated further to the right as a ‘block’ and both thoracic rings became more difficult to correct. The 5th thoracic ring started in right translation/left rotation and the lateral translation increased relative to the upper and mid thoracic rings above and below. The 6th thoracic ring started in left translation/right rotation and remained incongruent relative to the upper and mid thoracic rings. It translated to the right as a ‘block’ with the upper and mid thoracic rings during the squat task with the LLD corrected.
No correction of any driver in FU#1 restored the LLD, or the driver of FU#3.
Final Drivers for the Standing and Squat Tasks
There are many body region impairments and relationships in this case to consider.
The primary impairment (driver) is the structural deformity (FU#3 LLD); since no body region correction within FU#1 impacted another site of impairment (there are 4 in this unit) without the LLD correction.
Determining the secondary driver(s) requires careful consideration of the relationships between the impairments (who corrected who) separately in each of the two tasks evaluated; standing and the squat task.
In the end, each driver in FU#1 only had a partial impact on the other sites of impairment except for the pelvis and left hip which resolved with a co-correction of the three drivers listed below. All three can be considered co-drivers (type 2) since the best performance of the task, and patient experience, was when all three were corrected to the best of the practitioner’s ability.
Driver #1 – Left leg length discrepancy
Driver #2 – Thorax – TR5 priority ring
Driver #3 – Lumbar Spine
When left foot was elevated with 9 mm heel lift and auto elongation applied to Lumbar spine via caudal hand press over the pelvis, an eccentric lengthening occurred in the left lumbar iliocostalis and longissimus musculature. As a result, TR6 self corrected; however, TR5 remained stiff and difficult to correct. This suggests an articular system impairment within the 5th thoracic ring. These co-corrections resolved the alignment and control of the pelvis and hip thus eliminating them from the final driver list.
The client’s experience with the three drivers corrected was positive. She felt centered, and reported a significantly improved sensation and a reduction in effort in her lower back in both standing and during the squat task.
Further Assessment of the Driver(s)
Driver #1 – Left leg length discrepancy
No further assessment was required. Treatment is to provide a 9mm lift to her left shoe, only when this correction is tolerable for the thorax.
Driver #2 – Thorax – TR5 priority ring (started in right translation/left rotation)
Active and passive mobility for right rotation to neutral was restricted with a short, hard, vector noted on release of the attempted correction. These findings suggest an articular system impairment and further assessment of the relevant arthrokinematics of the zygapophyseal and costotransverse joints revealed the following:
Based on the active mobility assessment, the T4/5 right zygapophyseal joint demonstrated a restriction into thoracic extension, while the right 5th costotransverse joint exhibited limited mobility during inhalation. These findings are consistent with an articular system impairment affecting segmental motion.
For treatment, I applied a sustained Grade IV inferior glide to the right T4/5 zygapophyseal joint to facilitate segmental extension. Additionally, a sustained Grade IV lateral glide was performed at the right 5th costotransverse joint, followed by an inferior glide combined with a posterior roll using a hold-relax technique synchronized with breathing. This approach aimed to enhance joint mobility and restore segmental compliance during respiration. To reinforce the correction and maintain optimal alignment, Leukotape was applied to sustain the achieved thoracic positioning.
Specific manual mobilization techniques restored the arthrokinematic mobility and full active and passive mobility of TR5.
Driver #3 – Lumbar Spine
Due to the presence of a persistent, asymmetrical myofascial pattern in the lumbar spine resembling a compensatory scoliosis-like presentation, a more scoliosis-specific assessment and treatment approach was warranted.
To evaluate segmental control and muscular recruitment, the patient was instructed to perform an autoelongation maneuver by applying a manual press into the iliac crest. This assessment revealed significant difficulty in achieving eccentric lengthening of the left lumbar paraspinal musculature, which exhibited characteristics of pseudo-hypertrophy and excessive activation, suggesting a maladaptive neuromuscular response.
As an initial intervention, I applied Heisse Rolle, a German myofascial release technique that utilizes heat-retaining compresses soaked in hot water. This method provided thermal and mechanical stimulation to facilitate superficial tissue relaxation, enhance local circulation, and prime the fascia for deeper manual interventions. I then performed a neuro-myofascial release approach incorporating release with awareness and muscle recoil, promoting neuromuscular recalibration and improved tissue compliance.
Throughout these interventions, the principles of Dermo-Neuro-Modulation (DNM) were applied to influence the superficial nerve-fascial interface, optimizing sensory-motor integration and reducing protective muscle guarding. To reinforce these effects and support postural awareness, kinesiology taping was applied to facilitate sustained neuromuscular adaptation.
During the follow-up session, the patient demonstrated a continued need for scoliosis-specific motor retraining to restore segmental alignment, improve myofascial extensibility, and enhance motor control. To address this, I introduced corrective exercises based on the Schroth Method, a physiotherapeutic approach specifically designed for scoliosis management, emphasizing three-dimensional postural correction, rotational breathing, and sensorimotor retraining.
Conclusion
It is not uncommon to see individuals with persistent pain present with what appears to be a structural, or apparent, scoliosis combined with a leg length discrepancy (LLD) and individual regions that are not following the typical pattern of either. This case report highlights the specific tests that allow a practitioner to:
- differentiate when a noted curve in the spine is apparent vs structural
- differentiate when a leg length discrepancy is apparent vs structural
- layer on an ISM assessment in an individual with both conditions (spinal curve and LLD) to prioritize the best place in the body to intervene for the best possible outcome.
Complex clients require this depth of assessment and clinical reasoning.
These findings emphasize the necessity of a whole-body approach to assessment and intervention. Clinicians must move beyond rigid methodological frameworks to truly see and listen to the individual in front of them. Rather than being constrained by diagnostic labels, we must utilize them as one piece of a larger puzzle—guiding, but not dictating, our clinical reasoning. A deep understanding of biomechanics, neurophysiology, and lived experience allows us to prioritize interventions that restore functional integration and optimize movement efficiency in complex cases.
Skills Demonstration
Case Study Author
Clinical Mentorship in the Integrated Systems Model
Join Diane, and her team of highly skilled assistants, on this mentorship journey and immerse yourself in a series of education opportunities that will improve your clinical efficacy for treating the whole person using the updated Integrated Systems Model.
We will come together for 3 sessions of 4 (4.5) days over a period of 6-8 months with lots of practical/clinical time to focus on acquiring the skills and clinical reasoning to put the ISM model into practice. Hours of online lecture and reading material and 12 hours of in-person lecture are...
More Info