Story
Anthony is a 34 year-old male who was self-referred to Physical Therapy. Anthony was initially seen on August 21, 2019.
Anthony is a 34 year-old Physical Therapist that comes in with long-standing lower back pain, that initially occurred when he was 10-years old due to a fall onto his back off the monkey bars. At the time, Anthony had excruciating pain and had significant limitations with mobility. He was able to minimize his symptoms after several sessions with a Chiropractor. Throughout his lifetime, Anthony’s lower back pain would come and go. In 2015, Anthony had a severe exacerbation of his pain after an intense gym workout. This resulted in the inability to walk or perform other functional activities over the next few days. He received Physical Therapy to help alleviate his pain until he was able to return to function. Since this point in time, Anthony’s pain would return intermittently with an increase in severity depending on activity level. Anthony has not had any formal interventions since 2015 for his symptoms and has attempted to self-manage his symptoms.
Diane’s question:
Given the evidence published in the mid-1990’s by Dr. Julie Hides pertaining to LBP and the deep muscles of the trunk, which muscle in particular are you interested in assessing given this classic story.
Emil's response:
Given Anthony’s history and based on the work of Dr. Hides, a practitioner should be most concerned with the lumbar multifidi as it has been shown that these muscles tend to be inhibited with the onset of acute lower back pain. However, what made this research monumental, it showed that as acute lower back pain diminishes, the lumbar multifidus activation does not return automatically. An inhibited lumbar multifidus is one possible explanation for Anthony’s reoccurrence of lower back pain. In Anthony’s case, he does not remember, as he was only ten, if he received specific lumbar multifidi training. Thus, assessing the multifidi’s function may be warranted in the examination.
Anthony described his pain to be sharp and to the left lower back. He reported that the pain radiated down to his left buttock region. Just recently, he noted that the pain began to radiate down his right buttock region as well. On occasion, he would feel a cramp-like feeling to his left lateral calf and lateral hamstring. He also cited weakness and poor ability to recruit his left gluteus maximus. Anthony referenced difficulty with pushing off his left ankle when walking faster.
Anthony’s pain was provoked with prolonged positioning, especially if it was in a poor posture. It has affected his ability to work out in the gym, especially performing squats. The pain has affected his ability to perform certain duties as a Physical Therapist. In particular, he has difficulty with performing manual therapy techniques in the bent forward position and demonstrating hip hinging, squats, and anterior pelvic tilts.
Diane’s question:
Above you note that Anthony’s pain was provoked by ‘poor posture’. Many would suggest that this statement reflects a bias, or judgement, on your part since recently, more and more literature suggests that there is ‘no such thing as poor posture’ and that how you sit, stand and move is not related to pain (Slater et al 2019, Lewis et al 2020). How does this evidence resonate with your clinical experience? As an educator of physical therapy students, how do you translate this evidence into their clinical practice?
Emil's response:
It is quite difficult to find someone who does not have poor posture. In sixteen years of being an educator and teaching students about “normal” posture, every single student was found to have poor posture. Similar to the research showing that many individuals have a lumbar herniated disc, but have no pain, I believe posture falls in this same cognitive bias. Many individuals have poor posture but no pain, and thus cannot always be the contributing factor to dysfunction. There are numerous variables to consider why this is the case, such as time spent in poor posture, tissue resiliency, self-awareness, etc. I find it more helpful to correct associated poor posture and see if that influences a patient’s symptoms and presentation. To further analyze the influence of time, I will apply a vertical compression load to the spine and see if that may mimick the patient’s symptoms as well.
An MRI performed on 6/29/19 revealed the following:
- Left subarticular disc protrusion at L5/S1.
- Impingement upon the left S1 nerve root with mild stenosis of the medial left neural foramen.
- This is chronic with associated vertebral spondylosis.
- Mild facet hypertrophy L3,4 and L4-L5
Diane’s question:
The evidence suggests that 70% of the time medical imaging has no relevance to the clinical picture. Given the story above and the imaging results – how significant do you think they are to the current clinical picture and why?
Emil's response:
Numerous studies have shown a weak correlation of lower back symptoms and findings of dysfunction on radiological imaging. In Anthony’s case, he reported radiating symptoms and weakness of his gluteus maximus and calves. These findings are suggestive of some type of pathology to the L5/S1 nerve roots. The MRI provides a plausible explanation for these symptoms with its findings of an impingement upon the left S1 nerve root with mild stenosis of the medial left neural foramen. However, this serves to be one possible pathoanatomical explanation for his symptoms. Anthony may have other areas of compression causing these symptoms as well. From a pathomechanics perspective, an MRI does not assess neurodynamics, in particular, the dura’s ability elongate and slide within its tissue interface. A dura system that may not be able to elongate may find ways to shorten the musculoskeletal system and thus can explain why a particular joint may give up its functional stability in order to not aggravate a shortened dura/neural system. A key component in educating the patient is not to fixate on the findings of the MRI but look at the dynamic movement findings shown during the examination.
Past Medical History
Anthony has a past medical history of bilateral shoulder impingement that has responded well to Physical Therapy. He also noted intermittent cervical pain but never has received formal treatment for this complaint.
Meaningful Complaint
Anthony’s meaningful complaint was his inability to perform the duties needed to provide optimal Physical Therapy. The inability to perform his duties stems from his lower back pain when he demonstrates an exercise, performs manual therapy techniques, and transfers a patient. In order to gauge his progress, Anthony will use the intensity and frequency of his low back pain when at work.
Cognitive Beliefs
Anthony believes his symptoms are occurring due to a decline in activity and decreased local core muscle recruitment. He believes that there is still a nerve compression that his producing his symptoms and leg weakness.
Diane’s question:
What does he mean by ‘local core muscle recruitment’? Are there any specific tests you would add to his assessment to address these beliefs, in other words to validate or negate them and thus educate further?
Emil's response:
Anthony believed that his inability to recruit the local core muscles of his lower back had led to his poor control of his lower back, which thus led to nerve compression. In order to validate or negate his cognitive beliefs, real-time ultrasound can be utilized to demonstrate the initiation and bulking of the multifidi muscles in the affected area, in comparison to non-affected areas.
Diane’s response:
And if the practitioner did not have access to real-time ultrasound imaging, a specific assessment of the deep muscles responsible for segmental control would be warranted EVEN IF your ISM assessment found a distal driver (something far away from the lumbar spine) that when aligned and controlled, restored control of the low back). This would be treating his cognitive belief (psychological component of the bio-psycho-social approach) and not providing any necessary biomechanical information for planning treatment.
Meaningful Tasks
After a discussion of what he would hope to achieve from Physical Therapy, Anthony expressed an interest in improving the ability to perform pain-free squats. He felt this would help him as a Physical Therapist and get him back to working out.
To squat pain-free, the following screen tasks were chosen, as these components make up the requirements needed to perform a squat:
- Standing postural screen
- Squat
- Trunk extension
Screening Tasks
Screen # 1: Standing Postural Screen
To get a baseline on where his body initially starts a functional activity, a standing postural screen was chosen. One of the key goals was to determine the starting position of the body from which a comparison could be made during subsequent screening tasks.
At the time of the examination, no pain was noted with static standing.
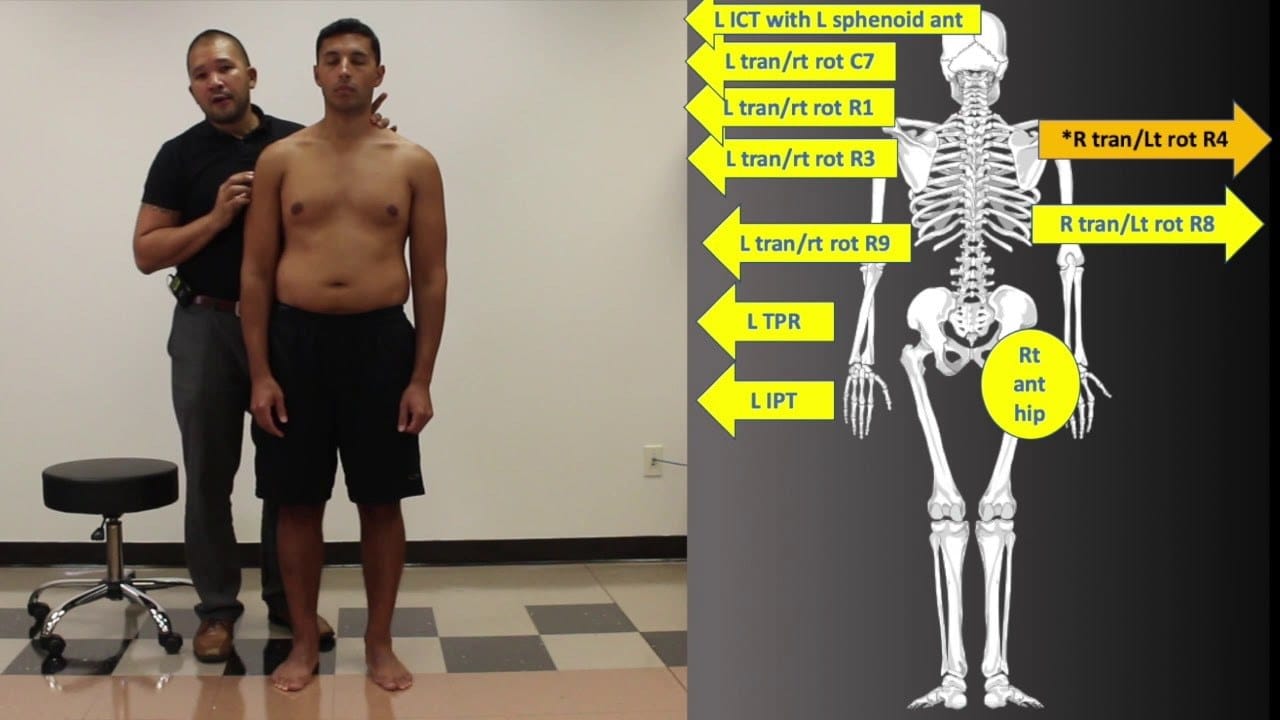
Functional Unit #1 (FU#1 – 3rd thoracic ring to the hips)
Pelvis: The pelvis was in a left transverse plane rotation (TPR), associated with a congruent left intra-pelvic torsion (IPT). The sacrum was left rotated and physiologically following the pelvis. The sacrum was also able to maintain its stability with left and right weight shifting.
Diane's question:
In an intra-pelvic torsion that is congruent with a left transverse plane rotation of the pelvis, as you note the sacrum should be left rotated ‘in space’. Where should the left and right innominates be relative to one another and where would the left and right innominate be relative to the sacrum?
Emil's response:
In a left intra-pelvic torsion, the left innominate rotates posteriorly, and the right innominate rotates anteriorly relative to each other. These combined motions would direct the sacrum to rotate to the left, and be termed a ‘Physiological rotated sacrum.’ However, in the case where the sacrum was rotated to the right, this would be termed an “Unphysiological rotated sacrum.’ An unphysiological rotated sacrum is suggestive of an SI joint that has unlocked because in order for the sacrum to rotate opposite of the innominate would require poor ligamentous/musculature support.
Diane's further question:
You are correct; however, what I am looking for here is less about direction of rotation of the sacrum and more about nutation or counternutation of the sacrum relative to the left and right innominate in:
- A LTPR/left intrapelvic torsion vs
- A LTPR with for example and associated ‘unlocked’ right SIJ
This is always a difficult concept for students new to ISM to understand and while the focus is still on relative osteokinematics between the innominate and sacrum, in ISM we don’t use positional testing of the sacrum to differentiate the two clinical scenarios since these tests are so unreliable. With respect to nutation/counternutation can you describe the relative position of the left and right side of the sacrum to the left innominate and right innominate respectively in a LTPR/LIPT vs a LTPR/right unlocked SIJ in the standing position?
Emil's response:
In the case where a patient presents with the a LTPR/LIPT, the left sacrum would be counternutated, and the right sacrum would be nutated. Whereas, with a LTPR/ right unlocked SIJ, the left sacrum would be nutated, and the right sacrum would be counternutated.
Diane's response:
If the left side of the sacrum was counternutated relative to the left innominate this would be an unlocked left SIJ. In an IPT, BOTH sides of the sacrum are nutated relative to their respective innominate even though the left side of the sacrum is more counternutated in space i.e. relative to the right side of the sacrum, it is still nutated relative to the innominate. This is the key difference between and IPT and an unlocked SIJ. So, in a LTPR/LIPT both the left and right sides of the sacrum are nutated relative to their respective innominate even though the sacrum is rotated to the left in space. In a LTPR/right unlocked SIJ, the right side of the sacrum is counternutated relative to the right innominate.
Diane's question:
You note that the sacrum was able to maintain its stability, and I would suggest that it is the sacroiliac joint the maintains stability, or control, as opposed to the sacrum. We test this by unloading and then then loading the SIJ in a weight shift task. What is the sub-optimal osteokinematic biomechanics to note between the innominate and the sacrum that would suggest that they SIJ is not controlled or ‘stable’ in a weight shift task?
Emil's response:
Yes, you made an excellent point, that merely saying “sacrum” alone, does not describe the relationship of the sacrum to the other structures for which its interfaces with. The sacroiliac’s open pack position is counternutation. Therefore, a practitioner should not witness counternutation of the SI joint in an activity where stability is needed, such as a weight shift task.
Hip: The right hip was found to be more anterior than the left, which is congruent to the findings of a left TPR.
Diane's question:
Was the right femoral head anteriorly translated relative to the right acetabulum in addition to being anterior to the left femoral head? Arthrokinematically, what would the difference mean for the right hip joint between the two clinical findings?
Emil's response:
If a practitioner’s observes that a femoral head is more anterior to another one, they must ask themselves, is the femoral head merely following what pelvis is doing, or is there an unstable hip joint, in which the femoral head is indeed translated within the hip joint. In this particular case, the right femoral head was more anterior than the left. Since there was a TPR left, this causes the right femoral head to be more anterior than the left, since the femoral head is merely following the lead of the femoral head. If the right femoral head was more anterior relative to its acetabulum, and there was a TPR left, this would be suggestive of an unstable right hip joint.
Thorax:
- The lower and mid thorax were rotated right. In particular, the 9th thoracic ring was noted to be left translated/right rotated, while the 8th thoracic ring was noted to be translated right/rotated left. Correction of the 8th and 9th thoracic ring was met with little resistance and both thoracic rings were able to move independently from one another.
Diane's question:
You note that the lower region of the thorax (thoracic rings 7-10) was rotated right and two thoracic rings within this region were translated/rotated. Given the net rotation of the lower thorax, which thoracic ring is of more interest – 8 or 9 and why?
Emil's response:
Since the overall rotation is to the right, one must ask themselves, what is causing this phenomenon to occur? In this particular case, the thorax region was rotated to the right. Therefore, a practitioner would be more interested in looking for the thoracic ring that is translated left/rotated right, in this instance the 9th thoracic ring.
- The 3rd thoracic ring was noted to be left translated/right rotated.
- The 4th thoracic ring was noted to be right translated/left rotated.
Diane's question:
Above you note that the mid thorax was rotated right. Given the positional findings of thoracic rings 3 and 4, which thoracic ring are you more interested in 3 or 4?
Emil's response:
Since the mid-thorax was rotated to the right, a practitioner would look for a thoracic ring that may be causing this rotation. Therefore, in this particular case, a practitioner would be interested in looking at the 3rd thoracic ring since it was translated to the left/rotated right.
Diane's question:
Where are the regions/segments of incongruence in functional unit #1?
Emil's response:
In this patient’s case, there were a number of incongruencies, such as:
- Pelvis: TPR L with the mid-thorax which was rotated to the right
- Mid-thorax right rotation with the 8th thoracic ring was noted to be translated right/rotated left
- Mid-thorax right rotation with the 3rd thoracic ring was noted to be translated left/rotated right
Functional Unit #2 (FU#2 2nd thoracic ring to the cranium)
- Upper thorax: TR2 was right rotated/left translated
- Cervical: C7 was translated left/rotated right
- Cranial: Left intracranial torsion with incongruent right rotated sphenoid.
Functional Unit #3 (FU#3)
Knee: The left knee demonstrated altered biomechanics with external rotation (ER) occurring with the descent phase of a mini squat and internal rotation when returning to the extended knee position. This is called a reverse screw-home mechanism.
Foot/ankle: Presented with bilateral medial tilted talus and internally rotated midfoot.
Diane's question:
Can you define a medial tilt of the talus please. Was the calcaneus also medially tilted, i.e. congruent with the talus, or was the subtalar joint able to adapt to the tilt with (depending on your definition of a medial talar tilt) pronation or supination?
Emil's response:
Medial tilt describes the talus position in relation to the tibia and fibula. A medial tilt occurs when the proximal talus moves laterally, while the distal portion of the talus moves medially. In this patient’s case, his calcaneus was able to remain neutral and thus suggesting STJ compensatory pronation.
Diane's question:
To be clear, when the proximal talus moves lateral and distal talus moves medially does this compress the medial side of the talocrural joint? If so, then I can see how you are describing a medial talar tilt!
Emil's response:
Yes with a medial tilt, the medial side of the talocrural joint is more compressed versus the lateral side.
Summary of Standing Screen Congruencies and Incongruencies
Diane’s question:
In a screening task, the summary of findings is less about drivers and more about congruency patterns. List the body regions that are congruent and those that are incongruent for all units. This informs what you will be watching for both to change in the movement task i.e. the squat as well as what is in compensation and what is driving patterns of motion.
Emil's response:
See chart below:
FU#1 FU#2 FU#3 Congruent with each other Pelvis: TPR L with the right hip and 8th thoracic ring congruent to the pelvis. - (Right hip anterior to left and 8th TR translated right/rotated left
- Mid-thorax right rotation with the 3rd thoracic ring was noted to be translated left/rotated right
Upper thorax: TR2 was right rotated/left translated Cervical: C7 was translated left/rotated right
Right STJ pronation of and IR of the midfoot Incongruent Pelvis: TPR L with the mid-thorax which was rotated to the right Mid-thorax right rotation with the 9th thoracic ring was noted to be translated right/rotated left
•Cranial: Left intracranial torsion with incongruent right rotated sphenoid. Right STJ pronation and ER of tibia Right STJ pronation and medial talar tilt
Screen # 2: Squat
A squat was chosen as that was the activity Anthony reported most difficulty with at the gym, and best represented the type of activity he needed to perform as a Physical Therapist. A squat is a unique activity that requires a combination of static stability of the trunk with concurrent dynamic stability/mobility of the hip, knee and foot/ankle. During squat, the entire spine should remain neutral, except for the later stages of a squat where the hip passes its end range of 120 degrees. At this point, there should be eccentrically controlled posteriorly pelvic tilt and lumbar flexion. The hips should flex bilaterally and the femoral heads should remain centered in the acetabulums throughout the range. The knees should also flex, with early internal rotation of the tibia and no excessive shearing between the tibia and femur. Bilaterally, superior tibia-fibular joints should glide posterolaterally. The talocrural joints should osteokinematically dorsiflex relative to the mortice associated with an arthrokinematic posterior glide of the talus in the mortice. The STJ should osteokinematically pronate eccentrically. Since the STJ is a bicondylar joint, the posterior joint is a convex on concave motion, and thus it should move posteromedially, while the anterior joint is a concave on convex motion and thus should move laterally.
The midfoot and transverse arches should be maintained initially, but eccentrically lowered into pronation as a person goes deeper into a squat. As pronation should occur, there should be a “fanning out” effect of the foot. Thus the medial structures, the navicular and medial and middle cuneiforms, first and second metatarsals should externally rotate about an axis of the 2nd ray, while the lateral structures, cuboid, and the fourth and fifth metatarsals internally rotate about this same axis. This results in fanning of the mid and forefoot in pronation.
Pain and difficulty performing a squat were noted.
FU#1 Findings
Pelvis: L TPR with congruent LIPT remained the same during a squat with no unlocking of the SIJs noted.
Hip: The right hip was found to be more anterior than the left, which is congruent to the findings of a left TPR. This finding remained the same during the squat.
Thorax:
- 9th thoracic ring left translated/right rotated and the 8th thoracic ring translated right/rotated left remained the same during the squat.
- The 3rd thoracic ring left translated/right rotated remained the same during the squat.
- The 4th thoracic ring translated even further into right translation/left rotation during the squat.
Drivers of FU#1
Correction of TR 4, fully corrected the dysfunctions in the thoracic region, but only partially corrected the pelvis and reduced the patient’s pain. Thus, the primary driver is the thorax (TR 4) with a secondary driver being the pelvis.
Diane's comment:
This conclusion would be validated, if correcting the pelvis did not improve TR 4 or any other thoracic rings.
FU#2 Findings
Upper thorax: No changed noted to TR2, which was noted to be left translated/right rotated.
Cervical: C7 was found to be left translated /right rotated and increased with the squat
Cranial: Left ICT and incongruent right rotated sphenoid remained the same.
Drivers of FU#2
C7 is the primary driver of functional unit #2 as it corrected all other dysfunctions found in functional unit #2 except for the sphenoid. Since the sphenoid didn’t correct with correction of C7, the cranium is either a secondary driver or there is a structural non-relevant asymmetry in the cranium.
Relationship between FU#1 and #2 Drivers (TR4 and C7)
Correction of C7 made TR 4 worse, and vice versa, however correction of both C7 and TR 4 most improved the pelvis alignment. Based on this presentation, C7 and TR 4 were co-drivers, at this point, for the squat task.
Diane's comment:
Given that the sphenoid didn’t correct with correction of C7 – you have a primary driver (C7) and possibly a secondary cranium (sphenoid) in functional unit 2. Therefore, you may actually have 3 drivers – cranium, neck and thorax for the squat task. Anything that remains uncorrected, still requires consideration going forward.
FU#3 Findings
Knee: The left knee demonstrated altered biomechanics with external rotation during the descent phase of a mini squat
Foot/ankle: Both feet presented with medial tilted talus and internally rotated midfoot.
Drivers for FU#3
No driver was found for FU#3, as correction of the feet or the left knee did not improve dysfunctions found in other areas of FU#3 or the meaningful task.
Diane's comment:
Both feet are in suboptimal alignment and the left knee is demonstrating sub-optimal biomechanics for this task, so even though correction the individual sites of impairment within FU#3 didn’t improve the other site within FU#3, they are still potential drivers for other units and need to be considered when the whole body is considered for this task.
Priority of all 3 unit drivers for the squat screening task
Diane's question:
What was the relationship between cranium (sphenoid in particular), neck (C7), thorax (TR4) and the feet (hindfoot medial tilt) – which driver has priority for first intervention in this treatment session?
Emil's response:
I did not analyze the impact of the drivers of functional unit #1 and 2, as did not see any correction in functional unit #3 affect the TPR of the pelvis. In hindsight, I see that how that was necessary in order to see the inter-relationship between all three units, as this could of have been done with having the patient correct functional unit #1 and 2, and I could have monitored functional unit #3.
Diane's comment:
Can you see how the flow for finding drivers for the whole body in a single task works now? Take a unit of the body with multiple impairments and find the driver or co-driver or primary/secondary driver within that unit. Then go to another unit and look for impairments and corrections, find drivers, then the 3rd unit. The play the unit drivers off one another to determine the final relationship between all 3 unit drivers and the task. This is the way I am teaching this now to expedite the assessment and avoid getting lost in the overwhelming amount of information that may not be relevant to the task being evaluated.
Overall driver for the squat screen
Diane's comment:
We are unable to determine the whole body driver for this task at this point since the impact of a cranial correction (sphenoid/ICT incongruency) was not noted on left knee and foot. The cranium correction did change the pelvis TPR/IPT so it is possible that the cranium is a player in this task. Based on Emil’s findings, his conclusion was that: Anthony had co-driver; the neck (C7) and the thorax (TR4). Correction of both drivers made each other worst; however, correcting both made the meaningful task the easiest to perform.
ISM certification is not about getting everything right – who does! It is about reflection, and learning more about our individual assessment biases, where we short cut, and how our habits may impact the assessment. Emil’s reflection decisions are helping him to grow as an ISM clinician.
Screen # 3: Trunk extension
Standing trunk extension was chosen as a task to screen because this motion narrows the intervertebral foramen bilaterally. The MRI indicated Anthony had a lateral recess stenosis, and thus, I wanted to ensure that he was able to withstand a maneuver that narrowed the affected lumbar segment. Also, it was noted that Anthony had more pain from returning to standing from trunk flexion, suggestive a poor tolerance towards extension. I also wanted to see his lumbar mechanics, to pick up additional drivers that may have not been found in the screens performed already, as in the other screens, the lumbar spine does not have to move from its neutral position.
Diane's comment:
Good clinical reasoning for choosing this task. It would also give you information about segmental control of his low back and an opportunity to address his cognitive belief that there is a local segmental control problem.
Standing trunk extension requires extension throughout the entire spine, arthrokinematically, a posterior translation and bilateral inferior glide is required at the Zygapophyseal joints (Z joints) in the lumbar spine. No rotation should occur in the lumbar spine.
Optimally, as extension occurs, the thoracic regions should posteriorly tilt. The thoracic vertebrae osteokinematically extend, arthrokinematically an inferior and slight posterior glide of inferior articular processes of the superior vertebrae occurs relative to the inferior vertebra at each segment. The thoracic rings should not rotate/translate. The ribs posteriorly rotate relative to their associated vertebrae and arthrokinematically, an inferior glide with a conjunct posterior roll of the ribs occurs at the costotransverse joints in the vertebrosternal and vertebromanubrial regions, and an inferior, anterior, lateral glide of the ribs occurs at the costotransverse joints in the vertebrochondral region.
The sacrum should remain nutated between the innominates as the pelvic ring posteriorly tilts, and the hips should extend bilaterally while the femoral heads remain centered in their respective acetabulum.
Pain and limited range of motion were noted with trunk extension.
Diane's question:
Where was the pain located and did it consistently occur when extension of the trunk reached a particular segment or region?
Emil's response:
The pain that Anthony experienced was consistent with the pain in which he cited during the subjective. The onset of pain was induced when the L4/5 region starting hinging.
FU#1 Findings
Pelvis: The pelvis maintained the left TPR/IPT and the SIJs retained control with trunk extension.
Diane’s addition and question:
Lumbar: This is where you would now add what the L5, L4 etc. did – there is no mention here of the lumbar segments yet your intention of doing this test was to evaluate the ability of the low back to accept load optimally – we need to know what the lumbar spine did in this task, if that was your intention of adding it to the assessment.
Emil's response:
As the patient extended, a notable “hinge point” was noted at L5/S1 with a noted decreased in posterior translation of the L5 vertebrae segment. As the patient moved further into extension, his pain increased, and his “hinge point” also increased. There was also a lack of upper lumbar movement into extension. These segments suggest a possible non-optimal mechanics to the lower lumbar spine, as the lumbar spine should move posteriorly. The limited upper lumbar motion may also result in requiring the lower lumbar segments to move in compensation.
Hip: The hips did not alter their position with standing trunk extension.
Thorax:
- 9th TR left translated/right rotated and the 8th TR translated right/rotated left remained in the same position during standing trunk extension.
- 3rd TR left translated/right rotated remained the same during standing trunk extension.
- 4th thoracic ring translated even further into right translation/left rotation.
Primary Driver of FU#1 was the thorax (4th thoracic ring).
Diane's question:
What happened to the ‘hinge point’ at L5-S1 with the TR4 correction? If the hinging still occurred in spite of the TR4 correction, you have a secondary lumbar driver. If it completely normalized i.e. the upper lumbar segments extended and the L5-S1 hinge disappeared, then you truly have a primary thorax (TR4) driver. Please add information here as to what the lumbar spine did with the TR 4 correction to justify your choice of a primary thorax driver (which suggests a normalized lumbar spine).
Emil's response:
The hinging seen at L5-S1 did partially correct with a correction of a TR4.
Diane's response:
Therefore, this is a primary thorax driver with a secondary lumbar driver since the lumbar spine biomechanics did not completely correct with correction of TR4 and further assessment at L5-S1 is warranted.
FU#2 Findings
Cervical: C7 was translated left/rotated right and increased with trunk extension.
Cranial: Left ICT and incongruent sphenoid right rotation remained the same.
Drivers for FU#2. Correcting the alignment of C7 improved standing trunk extension.
Diane's question:
Priority between FU#1 and FU#2 Drivers: Please make a statement about what the impact was on correction of C7 on TR4 and TR4 on C7 – i.e. time to play the drivers of the two units off one another.
Emil's response:
Correction of the primary driver of FU#1 and FU#2 made each other worse, and thus it appears that there is a possible codriver between C7 and TR4. A simultaneous correction of C7 and TR4 corrected the hinge point noted in the lumbar spine.
Diane's response:
Was the correction of L5-S1 complete? If so, then no further assessment of L5-S1 is indicated at this time and your drivers are the neck (C7) and thorax (TR4).
FU#3 Findings
Foot/ankle: Both feet presented with medial tilted talus and internally rotated midfoot and remain the same during trunk extension.
Drivers for FU#3
No driver was found for FU#3
Diane's comment:
If both feet performed sub-optimally during trunk extension, then they require consideration in relationship to the other functional units – the feet are the unit #3 drivers.
Priority of all 3 unit drivers for standing trunk extension screen: Neck (C7) and Thorax (TR4) were codrivers for this screening task.
A dual correction of C7 and TR4 did not alter the foot positioning, but it did fully correct the dysfunction noted in the lumbar spine. A foot correction did not alter the biomechanics of the back. In summary, C7 and TR4 are co drivers for standing trunk extension.
Screening Tasks Summary
In conclusion, Anthony did not have a single driver which helped the alignment, biomechanics, and control of other sites of impairment completely. Instead, Anthony had a consistent co-driver of the neck (C7) and the thorax( 4th thoracic ring). Correction of both drivers made each other worst; however, a co-correction of both optimally corrected alignment and biomechanics of the pelvis and the lumbar spine. This helps the clinician to prioritize which part of the body requires a further examination.
Drivers & Motor Control
An important decision a clinician must determine is whether to investigate the local core muscles, in particular the lumbar multifidi, in Anthony. It has been noted in the literature that lower back pain may inhibit the multifidus, and their optimal function may not have returned once the pain has been dissipated. However, one must determine the factors driving the lumbar spine to malalignment. A segment that is misaligned makes it difficult for the muscles that are attached to it, to contract correctly. Also, alignment leads to poor form closure and adds further to excessive motion. Therefore, careful observation is required of the impact of correcting drivers on lumbopelvic control. In particular, during a dynamic task, such as back extension, the lumbar spine must demonstrate dynamic control. As mentioned earlier, the lumbar segments must individually extend without any secondary rotation. This requires proper motor control to ensure motion is occurring in slow eccentric fashion at each segment. This occurs with the deep muscle system of the lumbar multifidi firing, with the superficial muscle system of the abdominals eccentrically lengthening in order to let this mechanics occur.
At the time of the examination, correction of C7 and T4 restored optimal alignment with no hinge to any segment in the lumbar region, thus from a motor control perspective, there was no need to assess the lumbar region further, nor was an assessment of multifidus required at this time.
In order to satisfy the patient’s cognitive belief that ‘there is decreased local core muscle recruitment’, dynamic segmental control tests were done. Resisted shoulder flexion was applied, and the ability of the lumbar spine to maintain control was noted. The patient was able to maintain lumbar neutral alignment with application of shoulder flexion resistance. This demonstrates that the multifidus is able to turn on automatically and thus does not require motor control retraining, and we can move on to strengthening and conditioning of the multifidus.
Diane’s comment:
Prior to treatment of the driver(s), usually a correction of the driver(s) is required for the recruitment strategy of the deep system of the lumbar spine to optimize. Here, you are saying that no correction of C7 and TR4 was necessary for optimal control of the lumbar spine. I would suggest; therefore, that he had a good strategy for arm elevation as opposed to backward bending. Perhaps the lack of control would have shown up if the resistance to loading had been done in more lumbar extension.
Emil's comment:
To justify why arm loading was chosen to assess dynamic control of the lumbar spine: It has been shown that a feed forward response of the deep muscular system in the trunk in anticipation of a load to the extremities. With resistance of shoulder flexion, the deep muscle stabilizers should initiate right away.
In summary, motor control training, despite the patient’s beliefs, was not a requirement for restoration of his ‘local core muscle recruitment’. This was shown by the ability of the lumbar spine to have proper neuro biomechanics when his drivers were corrected. Additional validation was done when the patient was able to maintain proper lumbar control during a resisted shoulder flexion test.
Diane’s comment:
Different task though, so the control he demonstrated without the drivers corrected in this task may merely mean that he had a better strategy for this type of loading.
Emil's response:
You are right, shoulder flexion was not associated with his meaningful task, and was merely assessing his ability to turn on the deep muscular system, but did not assess it during the meaningful task.
Further Assessment of the Drivers, including Vector Analysis
Further assessment is required for each region that was deemed to be a driver. The underlying impairment affecting the driver must be further assessed, as the impairment may be articular, neural, myofascial or visceral.
Active mobility tests carefully examine the ability of the driver to move correctly without compensation. Active listening may be utilized to feel the amplitude of range of motion that is ‘easy’, non-resistant and effortless. Active control tests assess the ability of the driver to remain in neutral when a force is applied. Passive control tests are indicated if there is a history of trauma to the driver. These tests examine the integrity of the passive structures (ligaments, capsule, discs, etc.) to resist shear, or other non-physiological motions, at a joint . Finally, passive mobility tests are utilized to assess available passive range of motion. Passive listening for the location, length and quality of restrictive vectors provides further information as to the underlying system impairment(s). If the movement is affected, a correction is attempted, and the Physical Therapist carefully feels for a vector that is limiting the ability to restore normal range of motion. Critical components for the physical therapist to be aware of is the angle of direction and when does the pull occur. A systematic approach of determining if a pull is more anterior, posterior or within the cavity, will give a PT a better picture which structure may be affected. The quicker onset of a pull suggests a more local vector versus pull that takes longer to occur.
Cervical Driver – Further Assessment of C7
Active mobility tests: Since C7 was left translated/right rotated, left rotation was assessed as a right rotated segment could alter a person’s ability to left rotate.
It was noted that left rotation was limited at C7-T1 and that left translation/right rotation of C7 increased during the left rotation task – this is incongruent biomechanics of C7 for this task. A dynamic active listening revealed a short anterior vector coming from the left anterior scalenes.
Diane’s question:
Below you beautifully describe a visceral vector that explains why you had to do a co-correction of C7 and TR4 to get the best result at L5-S1. Did the passive listening stop with the scalenes or go into the visceral thorax?
Emil's response:
At the time of the examination it stopped to the scalenes.
Active control tests: Resisted left shoulder flexion did not increase the left translation/right rotation of C7. This suggests there is enough motor control/strength capacity to maintain control at C7.
Diane’s comment:
Or it could also suggest that the restrictive vector is masking an underlying control impairment that may show up upon release. I find that active and passive control tests are not applicable in the presence of restrictive system impairments, but may be done at a later session.
Passive mobility tests: The dysfunctional C7, which was left translated/right rotated, was passively attempted into left rotation.
This was done with success; therefore, a capsular restriction was ruled out at this point. However, when trying to restore the segment into its neutral position, a short vector was initially felt from the left anterior scalene.
Passive control tests: This was not performed as there was no history of trauma to this region, nor was there a subjective complaint of pain, catching and/or clicking.
Thorax Driver – Further Assessment of the 4th Thoracic Ring
Active mobility tests: Right thoracic rotation was examined, as a right translated/left rotated TR4 dysfunction could limit right thoracic rotation if restricted. Limited motion was noted, and active listening suggested a vector from the right upper quadrant area of the abdomen.
Active control tests: Resisted shoulder flexion was utilized to evaluate TR4’s ability to resist the necessary force and to assess motor control. The patient here showed no dysfunction.
Diane’s comment:
same comment as above – suboptimal strategies that restrict thoracic ring mobility often mask, or hide, an active control problem and only manifest after restrictive vectors are released.
Passive control tests: This was not performed as there was no history of trauma to this region, nor was there a subjective complaint of pain, catching and/or clicking.
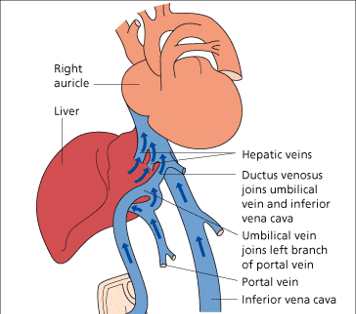
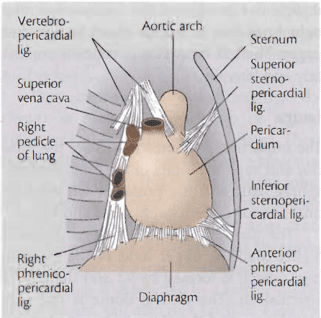
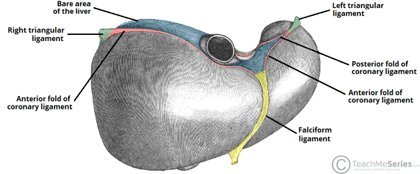
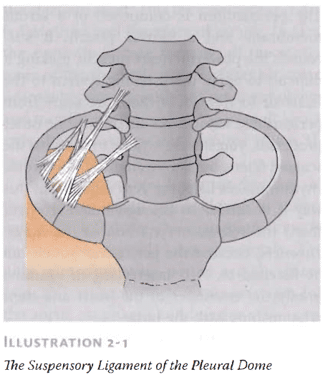
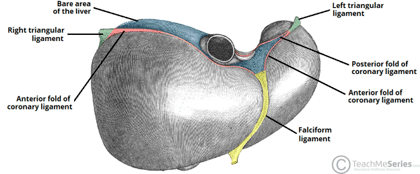
Passive mobility tests: Passive mobility of right rotation of TR 4 was limited and correction of TR4 right translation/left rotation revealed a strong vector of pull anteriorly in the right upper quadrant inside the abdomen. Follow up visceral assessment revealed a vector connecting the right 4th rib to the liver – see below for description of this anatomy.
Hypothesis
Anthony’s initial injury and trauma were to the lower back that received treatment to restore function. However, as time progressed, he responded less and less to interventions that were primarily focused on the lower back. Thus, the codriver found in the thorax (TR4) and neck (C7) may have never been addressed, which can explain the chronicity of his condition.
Diane’s question:
How would an initial low back injury cause a thoracic ring to rotate especially TR4 and C7 to compensate and rotate the other way? Think about motor control strategies that commonly change in deep and superficial muscles in a low back injury – what gets over-active – how far up do they go i.e. iliocostalis, EO? Etc.
Emil's response:
Whenever an individual has pain to a specific location, i.e. the lower back, the body can respond in a myriad of ways. It has been shown that the deep stabilizers are inhibited with pain, and thus leaves the body further vulnerable to shearing forces, and may be a new source of pain. Commonly, the body will limit movement, and thus limit pain by utilizing the long global muscles such as the external oblique and iliocostalis. These global muscles provide local stabilization to the lumbar spine, and thus will limit pain. However, as these muscles stabilize the local region, these same muscles will have a secondary effect on the bony structures in which they attached. For example, the external oblique, with its attachments to the ribs, may cause a thoracic ring dysfunction, due to its ability to induce rotation. The iliocostalis, which its attachment to the ribs as well, may cause a rib to posteriorly rotate, and thus cause thoracic ring rotation. As these muscles affect the thoracic ring, the cervical region will often have to compensate, and thus further add to the sequelae of events that originated in the lumbar spine.
Anthony also revealed in subsequent visits that he has a history of IBS. It is plausible that the combination of possible trauma to the abdomen and the compensations seen led to his chronic lower back pain.
Treatment Plan
The ultimate goal for Anthony was to be able to perform his functional tasks at work pain free and with optimal strategies for transferring loads that ensure efficient movement and control. The examination revealed Anthony’s barrier getting in the way of performing his functional task was due to the co drivers seen at TR4 and C7. Thus, the initial treatment concentrated primarily on releasing these drivers. Control training was not necessary as mechanics to the lumbar spine were restored with correction of this co-driver (C7 and TR4). Once the drivers were released, movement training with an emphasis on restoring optimal alignment, biomechanics and control during all tasks that pertain to his meaningful task of a squat and backward bending could begin.
R: Release system impairments of the co-drivers TR4 and C7. Left anterior scalenes (C7). TR4 required the release of the liver viscera to restore normal alignment of TR4.
In order to show the possible inter-play between the TR4 and the viscera, I have provided a chart below.
A: External focus cues on creating space by imagining there are strings at the cervical and thoracic region was imperative to maintain alignment of both C7 and TR4. Further cueing was necessary to make sure that the muscles weren’t bracing and creating a rigid response. Cues using the most minimal force were necessary while still being able to breathe.
C: This was not deemed to be necessary as correction of the neck (C7) and thorax (TR4) restored normal alignment and biomechanics at L5-S1 and alignment of the pelvis. Also, active control testing demonstrates sufficient strength/motor control for both C7 and TR4.
M: Movement training utilizing the principle of motor learning is necessary for his squat meaningful task. The squat should be progressed via adding more weight and to be able to perform jumping single leg squat. Under both conditions, monitoring of the codriver is imperative to ensure adequate control is being met, versus relying on symptoms alone. Continued emphasis on utilizing external cueing, knowledge of performance, variability of training, contextual interference, in multiple environments with added cognitive stressors will be utilized.
A positional release technique with release with awareness was used to release the left anterior scalenes. This was followed by releasing the vector connecting the liver with the TR4. Once these two system vectors (neural and visceral) were released, the patient was able to squat pain-free with subjective reports of greater ease. Therefore, the beginning of movement training was implemented, with the metaphor of creating space to the co-drivers for maintenance of alignment. Anthony was able to perform two bouts of 30 seconds of pain-free deep squats without any symptoms or worsening of his codrivers.
Followup treatment sessions
Anthony was seen for two follow up sessions after the initial evaluation. In the follow-up sessions the C7 was found to have a vector which responded to further release of the visceral vector noted on the first session.
Further assessment of combined movements of the trunk, such as those required for work as a physical therapist revealed altered biomechanics at L3-4. Further assessment of L3-4 revealed restricted extension, left side-flexion at L3-4 secondary to an inability of the left Z joint to glide inferiorly. Passive listening determined this impairment to be articular. This was treated with a grade 3-4 vector-specific mobilization.
At the last visit, Anthony reported no longer having radiating symptoms. He was able to walk and squat pain-free. He also reported being able to sit and stand pain-free as long he maintains a good posture. After the last visit, Anthony was able to perform a deep squat and left single leg squat with load without any pain with his co-drivers (C7 and TR4) maintaining a neutral position. He was given a long-term treatment plan with an emphasis on performing his home exercise practice daily, but mainly before he works out and before he treats. Anthony was told to return to running once he was able to perform a jumping singe leg squat without losing active control of his co-drivers. As he continues to decrease the irritability to the lumbopelvic region and continues to release his codrivers and maintain good alignment during his functional tasks, he will continue to minimize his pain, optimize his performance, and improve his overall function.
References
Barral, J.P., Mercier P (2005). Visceral Manipulation Revised Edition. Seattle, WA: Eastland Press.
Barral, J.P.(2007). Visceral Manipulation II Revised Edition. Seattle, WA: Eastland Press.
Skills Demonstration
Case Study Author
Clinical Mentorship in the Integrated Systems Model
Join Diane, and her team of highly skilled assistants, on this mentorship journey and immerse yourself in a series of education opportunities that will improve your clinical efficacy for treating the whole person using the updated Integrated Systems Model.
We will come together for 3 sessions of 4 (4.5) days over a period of 6-8 months with lots of practical/clinical time to focus on acquiring the skills and clinical reasoning to put the ISM model into practice. Hours of online lecture and reading material and 12 hours of in-person lecture are...
More Info