- Message from Diane:
Every once in a while, an ISM Series graduate qualifies for certification simply through the process of the dialogue between us that creates a beautiful ISM clinical reasoning form, without following this with a written case report. Dave’s journey to ISM certification was a tough one in that he had done the Series in 2009 and I was expecting him to be at the level of certification of 2023! He had a lot to catch up on and the 2 year process was way harder than writing a case report within two years of doing the ISM Series! His clinic in London, England, BodyMechanics, is now an affiliate of Diane Lee & Associates where Dave is now qualified to mentor others and join my assisting team. Well done Dave!
My Journey to Certification
I was a graduate of the Integrated Systems Model (ISM) series in 2009 when it was hosted in the UK. I had the privilege of assisting Diane with the running of the next 2 UK based series. The process of formulating a hypothesis from the findings of an assessment using the ISM has become part of the fabric of what I do every day. Having an assessment process that allows me to understand the relationship between different body region impairments has become second nature to my practice. With this in mind, the challenge of becoming certified as an ISM practitioner should have been a straight forward task.
Completing the Clinical Reasoning Form (CRF), and going through the process of certification with Diane, showed me how much the process has evolved since I completed and assisted 10 years ago. It has been invaluable to my ability to coach and mentor my team who have either completed the ISM series or are aspiring to do so.
When my assessment of a client was laid bare and my findings were questioned in order to look deeper at the relationships between impaired body regions, I found myself having a crisis of confidence. Pattern recognition was no longer good enough; clear reasoning needed to be shown and demonstrated and areas that I might skip in a clinical session were highlighted so that I could see the areas that needed to be sharpened in order to make my assessment and treatment better. This led to an emotional rollercoaster. Self-doubt crept in but the desire to improve my thinking, reasoning and ability to formulate and share information came to the fore.
Systematically looking through a functional unit of the body (i.e. 3rd thoracic ring to the hips is one functional unit, 2nd thoracic ring to the cranium another and the extremities a third) and deciding whether there was a need to further assess another functional unit was a new concept for me and demonstrates how the ISM assessment has evolved to become more focused and easier to use in a clinical setting. If a screening test is made 100% better with the input, or changes provided to a specific area of the functional unit with no detriment to other functional units (areas of the body) then that is the best place to start your treatment. In ISM this is called finding the driver. My journey from assessing the whole of the system and ‘playing areas off against each other’ has worked well for me over the last decade or so, but the challenge of breaking the assessment down in to a CRF and going through the process functional unit by functional unit made my head spin.
My client’s story was one of persistent back and leg pain with history of multiple inputs (physio, orthopedic review, chiropractor, sports massage) to no avail. The MRI was non remarkable and he was of the belief that nothing could change. In his assessment, we found that a positive change in his experience (decrease in pain) and performance in his screening task occurred when thoracic rings 4, 5 & 6 were aligned and controlled. The leg and foot improved position such that it was the same as the opposite side. Historically, given the limb’s poor position in the standing screen, I would still have investigated this further, but that is not the way of ISM functional unit assessments!
When the thorax was corrected (thoracic rings 4, 5, &6 aligned and controlled), the posture of the neck and head actually worsened, so even though his experience and performance of the screening task has improved, this finding now tells me that there is a relationship between the functional unit #1 driver and an impairment in functional unit #2. Through the ISM certification process I learned a new process to determine if a second unit required investigation and this has expedited all of my assessments. These quick unit tests are now a key part of my assessment.
My realization on reviewing my assessment of functional unit 2 was that I had not incorporated new learnings that had been introduced to the ISM Series since my completion. The integration of the cranium and the craniovertebral region with its relationship to the clavicles and the first thoracic ring was a missing piece of my puzzle, and I was brought up to speed through the short ISM for the Head, Neck and Upper Thorax course taught by Diane in Denmark.
The efficiency of a whole body/person ISM assessment is enhanced using the functional units and the structure of the new CRF. Expediting finding drivers faster is beneficial to all clinicians who might find that looking at the whole body is time consuming and difficult within the allotted time of an assessment. The ability to break the process down and then identify the relevant area faster is definitely a big take away for me, and my team, from doing this ISM certification and the short ISM course in Denmark.
The ISM certification process has highlighted where I have been ‘cutting corners’ in assessment and learning how ISM has evolved since 2009 has also been enlightening. My ability to coach and mentor my team has been enhanced and my confidence in my own ability to assess using ISM has been bolstered by going through the certification process.
Story
SC is a 24 year old gent who came in to clinic complaining of chronic R LBP and weakness of the leg. He has had previous investigations and treatments to no avail. Complains of leg being immobile and weak ‘due to an ongoing issue around the low back R hand side, pelvis and groin’. Discomfort started to travel up the back. Had steroid injection, nerve injection (this made things worse) MRI lumbar spine showed wear and tear disc L5/S1 but otherwise NAD. Prev physio, chiropractor, osteo, acupuncture – none made any lasting improvement. Has ‘a lot of pain and a lot of issue throughout every day’. Wakes with dull ache / throb, shooting pains during the day, ache and throb in general.
Changed from working as a plumber to a GP receptionist (part time) to help manage pain day to day – significant change in income.
Past Medical History
Fall on to R hip in teens. No #s, Assaulted when aged 18. No other ailments
Meaningful Complaint
Agg – extension in standing, erratic movements, standing R foot forward – feels body pain and decreased balance / weakness. Walking. All sporty movement.
Meaningful Task - Walking / R step forward
Screening Task - Left One Leg Stand
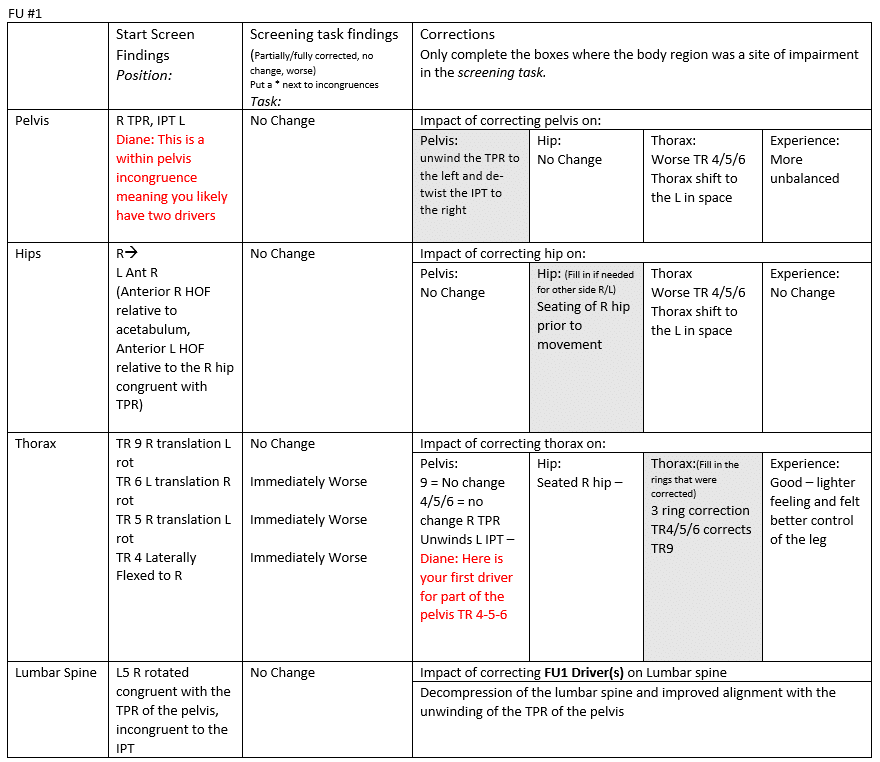
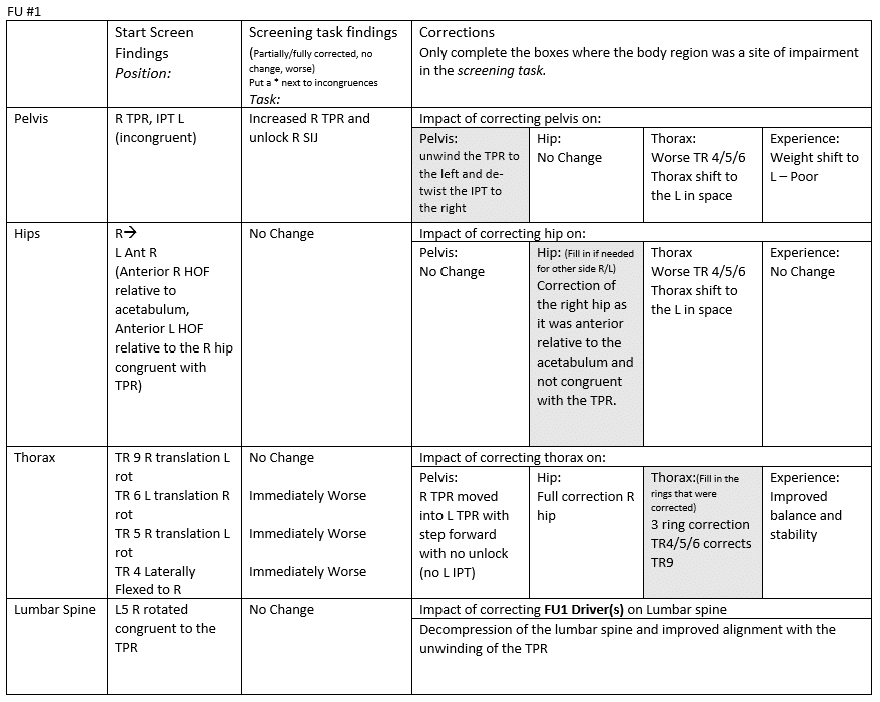
Functional Unit #1 (FU#1)
Start Screen: Standing
Driver for FU#1
The three TR4/5/6 ring correction unwound the IPT but did not affect the TPR of the pelvis. Right Hip seated.
Primary thorax driver (TR 4, 5, 6) – Whilst I didn’t do a rotation of the cervical spine and ascertain whether my correction of FU#1 had made a difference to the movement, I could see that there was still a translated upper cervical spine and the cranium had not corrected – this led me to assess FU#2.
- Diane’s comment:
Perfectly good reasoning – observation vs movement – doesn’t matter – you have a visual finding that prompts further unit assessment. You still have a secondary pelvis driver at the moment in that the TPR didn’t correct with any FU#1 correction although in the step forward task you note the correcting the 3 thoracic rings unwound the pelvic TPR?
Functional Unit #2 (FU#2)
Start Screen : Standing
Driver(s) for FU#2: Primary Cranial region (C0/1/2)
Correction of the thoracic rings 4/5/6 improved C0/1/2 but did not fully correct the complex or the cranial torsion, however, the experience of the task was that it was markedly decreased pain and the task felt better controlled. Correction of C0/1/2 did not improve the thoracic rings but it did have a positive effect on the experience of the task (but not to the same extent that FU#1 had).
- Diane’s question and summary of drivers:
Did correcting anything in FU#2 unwind the TPR of the pelvis?
So at this point your drivers still are:
Primary: Thorax: TR 4/5/6
Secondary: Cranial region: C0/1/2
Not sure if we have to consider the TPR of the pelvis?
FU #3 – Lower Extremity
Not assessed as corrected with FU#1 correction.
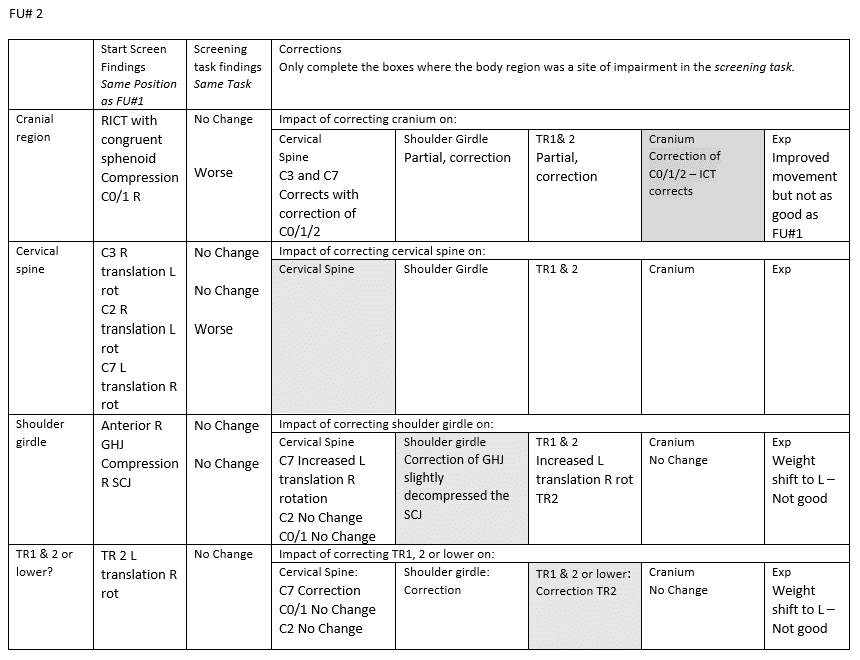
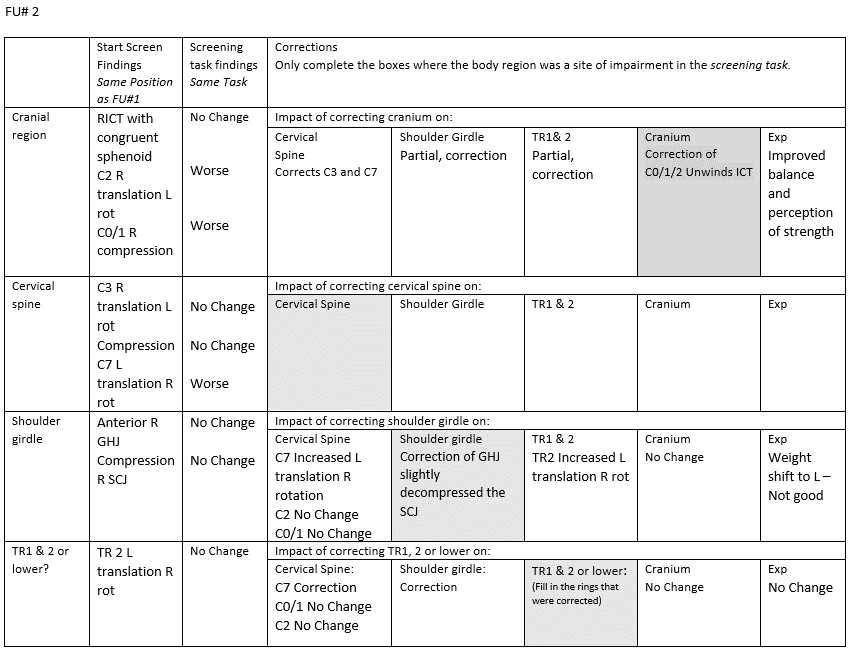
Screening Task - R step forward
Functional Unit #1 (FU#1)
Start Screen: Standing
Driver for FU#1
Primary thorax driver (TR 4, 5, 6) – Whilst I didn’t do a rotation of the cervical spine and ascertain whether my correction of FU#1 had made a difference to the movement, I could see that there was still a translated upper cervical spine and the cranium had not corrected – this led me to assess FU#2.
- Diane’s question:
So in this step forward task you do note that correcting the three rings of the thorax corrected the RTPR – did this not happen in the LOLS task too? If it did then you don’t have a pelvic driver – just a thoracic one.
Functional Unit #2 (FU#2)
Start Screen : Standing
Driver(s) for FU#2: Primary Cranial region (C0/1/2)
Relationship of driver(s) FU#1 & FU#2:
Correction of the thoracic rings 4/5/6 improved C0/1/2 but did not fully correct the complex or the cranial torsion, however, the experience of the task was that it was markedly decreased in pain and the task felt better controlled. Correction of C0/1/2 did have a positive effect on the experience of the task (but not to the same extent that FU#1 had).
When C0/1/2 correction was added to the TR4/5/6 complex, there was no pain at all in the task and the experience was such that the client could not believe that he was stepping and his body was not reacting in a negative way.
Final Drivers: Primary thorax, secondary cranial region
- Diane’s comment:
Awesome – I don’t think the pelvis is driver here at all – most likely unwound with the CV correction.
FU #3 – Lower Extremity
Not Assessed as corrected with FU#1.
Final Drivers
Primary: Thorax Region: TR4/5/6
Secondary: Cranial Region: C0/1/2
Further Analysis of the Drivers
(Active mobility, passive mobility (including vector analysis), active control, passive control).
Which assessment tools do you need? Which are irrelevant?
Primary Driver: Thorax: TR4-5-6
Active Mobility
I assessed thoracic rotation (given its role in walking). R rotation immediately increased the compression of ring 4 on 5 and subsequently the R translation of 5 on 6. Range was limited ( and felt awkward). L rotation, ring 6 increased in translation to the L half way through range.
When correcting the 3 rings, there was an internal vector not allowing the rings to decompress. It was a sensation of the rings being sucked inwards, particularly on the right side. By trigger point release of the diaphragm on the right side, in a forward flexed position, breathing improved and ring mobility improved to allow correction.
- Diane’s comment:
So by this description we can rule out an articular system restriction right? My first question is always “Can I correct these rings?’ You couldn’t not because of a hard stop endfeel, but rather this visceral pull didn’t allow enough space between the rings to move properly. The visceral listening took you into a visceral release which then allowed you to correct – this then ruled out any articular restriction.
As I continued to test, a lateral costal breath created the most tension on the rings when correcting them. In order to carry out a correction the 4th ring needed to be decompressed and this automatically started to unwind rings 5 and 6. Full correction was achieved with minimal force needed (the most force was needed to decompress ring 4 which had a short vector and also what felt like and internal vector). Given the ease with which the correction could be completed, I opted not to further assess the passive mobility of the rings as there was little evidence to point towards an articular element being involved.
- Diane’s comment:
perfect
To release these vectors, I used Breathe and Stack with a 3 ring correction in a neutral sitting position and in R thoracic rotation. At end of inspiration I also added a small fascial glide in to the short vectors (anterolateral intercostals) to encourage release of the compression of the 4th ring on the R side. On reassessment following release, full rotation was restored and breathing felt easier. On standing, the IPT, hip and foot corrected and the task was easier, but the TPR maintained.
- Diane’s comment:
aha – here it is – the thorax was not in relationship to the TPR of the pelvis!
There was no unlocking on LOLS or R step forwards. There was still no change to the upper cervical spine and correcting only the upper cervical spine now gave full relief of symptoms and ease of movement.
Once vectors were released, rotation was controlled but I did not test active control of the thorax with an upper limb challenge. As there was no history of trauma or notable step deformity I did not carry out passive control tests of the thorax.
Home Exercise for the thorax
Self correction taught – decompressing the 4th ring and supporting rings 5/6. Self breathe and stack were shown with rotation to be used as a check movement (ie is there any restriction to the movement) and as part of the homework (self correction, rotating to the point of restriction and breathing x 3). Once released and able to move freely into rotation, lying supine with knees flexed, self correct and knee rolling (3×10).
Secondary Driver: Cranial Region: C0/1/2
This is where I realise that while I tested the active mobility and passive mobility of the OA but not the AA joints, I was not as specific as I could have been (having reviewed the assessments on the ISM Flow).
Active Mobility – OA / AA joint restriction in to flexion R side (but I didn’t ascertain the timing to differentiate between the two). C2 not tested in to flex / ext.
Passive Mobility – OA joint restricted in to flexion R side. Occipital condyles glide anteriorly symmetrically but restricted R side in posterior glide with short vector tension. I did not test in to rotation. C2 correction possible with superior vector towards the cranium.
Active / passive control OA – Extension controlled in sitting (symmetrical) but flexion deviates to the right.
Short vectors (suboccipital space) were palpable on the R side. Trigger point release and mobilisation in to OA flexion created symmetry in testing movements and aligned C2. Vectors were vertical and rotational which suggests that there was tension restricting the AA joint as well as the OA joint.
Home exercise for the cranial region
Standing back to wall as if in a height competition with someone behind you, chin retraction and R rotation self mobilisation to maintain movement restored by passive mobilisation.
- Diane’s comment:
I can clearly see the principles of ISM through this complete two task clinical reflection form and the further assessment of each driver. Well done Dave!
Case Study Author
Clinical Mentorship in the Integrated Systems Model
Join Diane, and her team of highly skilled assistants, on this mentorship journey and immerse yourself in a series of education opportunities that will improve your clinical efficacy for treating the whole person using the updated Integrated Systems Model.
We will come together for 3 sessions of 4 (4.5) days over a period of 6-8 months with lots of practical/clinical time to focus on acquiring the skills and clinical reasoning to put the ISM model into practice. Hours of online lecture and reading material and 12 hours of in-person lecture are...
More Info