Story
Mr. B. first presented to clinic on January 9th, 2017 for his initial assessment and treatment. He is a resident of Chilliwack, BC and chose to connect with the clinic after searching online for men’s pelvic health treatment. The following is a summary of his story that was gathered during his assessment in clinic.
Mr. B. described a long standing tendency to grip and hold his abdominal muscles throughout the day which began as a strategy to reduce the appearance of a large “tummy”. He described being conscious of this appearance and the use of this gripping strategy for the past 12 years. Mr. B. is a busy father of two (a 2-year-old and a 14-year-old) and works as a registered massage therapist. Mr. B. re-counted a meaningful experience in his past that he feels contributed to his current experience of pelvic pain and dysfunction. Years ago Mr. B. remembers being very stressed balancing massage therapy school and family responsibilities while at the same time dealing with the unexpected death of a close friend. He remembers taking up pumpkin carving in his garage as a cathartic release of stress and anxiety. He noted that while sitting and carving pumpkins he would regularly feel the urge to urinate but would use his abdominal gripping strategy “sucking in his tummy” to reduce the urge to void for long periods of time. Overtime, he began to use this gripping strategy to avoid urination throughout the day. Over the following 2-3 years, Mr. B. experienced urinary symptoms including urinary urgency and frequency, nocturia, post-micturition dribble, penile irritation, penile spasms and pelvic girdle pain (PGP). Last year, after being unsatisfied practicing at a number of massage therapy clinics, Mr. B. took on the task of opening his own practice. He noted that this move increased his stress and anxiety and caused a gradual worsening of his urinary symptoms. In March of 2016, Mr. B. was involved in a motor-vehicle accident that resulted in the development of right arm and hand weakness and paraesthesia. He had x-rays and an MRI of his cervical spine to investigate potential injury to the neck secondary to his arm symptoms. The MRI identified a posterior disc protrusion that indented the anterior thecal sac and contacted the spinal cord at the level of C5/6. There was also a left posterolateral disc protrusion causing narrowing of the left intervertebral foramen at the level of C6/7. He sought out treatment for his injuries and has been seeing a physiotherapist, chiropractor and massage therapist in Chilliwack for his injuries stemming from the accident.
In Mid-November of 2016, his symptoms took a turn for the worse. He began coughing and sneezing due to a cold, this stress and strain caused him to experience diaphragm and abdominal spasms that extended from his navel to his pubic bone. Mr. B. also noticed that sitting at work and while pumpkin carving would aggravate his PGP. At the time of his first appointment Mr. B. had been making efforts to improve his overall health and wellbeing. He began a kettlebell exercise routine, and started seeing a clinical psychologist in addition to his physiotherapist, chiropractor and massage therapist. He noted that despite all of this, his urinary symptoms and PGP had not improved. At this point, he was not able to sleep through the night due to his nocturia causing him to wake every 1.5-2 hours to void. He also noticed that doing his own myofascial release of his external obliques offered some relief of his PGP, however he couldn’t achieve complete relief despite his efforts. His goals for physiotherapy were to improve his PGP, reduce his urinary symptoms and discover how his urinary function could be related to his history.
Meaningful Complaint
At his initial assessment, Mr. B. noted that he had bilateral PGP felt along his perineum that radiated into the testicles and penis. He also had urinary symptoms including low urine flow, post-micturition penile irritation, penile spasm, and urinary frequency/urgency and nocturia.
Diane’s question
Mr. B has been experiencing his perineal pain for ‘years’ and it is likely that there is some sensitization of the neural pathways. How will you structure your assessment to determine the role of peripheral mechanisms vs central mechanism in his pain experience?
Calvin’s response
A thorough understanding of the contributing factors to one’s pain experience cannot be assessed without considering the potential inputs affecting the pain neuromatrix. Melzack (1999) identifies these inputs as cognitive-evaluative, sensory-discriminative and affective-motivational. According to Moseley (2003), there are 2 mechanisms that contribute to the chronic pain experience via sensitization of the central nervous system, these include nociceptive (i.e. immune, hypothalamic-pituitary-adrenal system) and non-nociceptive (i.e. cognitive/emotional) inputs to the pain neuromatrix. Mr. B’s pain was complex with many potential contributing factors. The approach was to first hear the entire story and then ask questions to determine the nature of the pain experience. Subsequently, an ISM assessment was used to determine the behaviour of his pain in relation to areas of FLT. Finding these areas of FLT and determining drivers for them often involves changing sensory-discriminative and cognitive-evaluative inputs to the pain neuromatrix to produce changes in pain perception and movement.
From Mr. B’s story, there was a significant worsening of his pain over several years which was associated with anxiety, depression and stress from specific life events (i.e. the death of a friend, starting his own business) and dissatisfaction with his general health. Considering the chronic duration of his pain and the aggravation of pain from normally non-noxious stimuli (i.e. coughing and sneezing), there may be a component of central sensitization driven by a combination of cognitive-emotional and sensory-affective inputs to his neuromatrix of pain. The gradual worsening of his symptoms in response to anxiety and emotional stress may also lend to a central sensitization mechanism. Moseley (2003) proposed that changing the chronic pain experience requires assessment of the “painful/inappropriate motor strategy”. Moseley (2003) states that one potential mechanism that can modify an inappropriate motor strategy can involve changing posture and also changing physical demands (i.e. breaking up the task of interest). The ISM approach was used to correlate areas of FLT to Mr. B’s pain experience using screening tasks to see if these areas would change the sensation of pain and gripping (the threat response) in his pelvic floor. In this case, finding drivers was required to remove the sensory-affective inputs to the pain neuromatrix and cueing breathing and relaxation of the perineum and letting go of his abdominal wall gripping strategy was helpful in producing a change to the cognitive-emotional input (anxiety/fear/perceived threat) in the meaningful task.
Meaningful Tasks
Based on Mr. B.’s story, standing and sitting were identified as his meaningful tasks. Standing was chosen because it is a functional position for male urination and sitting was noted by Mr. B. as an aggravating posture for his pain.
Cognitive Belief
Mr. B. had a long history of urinary symptoms before he came in for treatment. As such, he had developed a cognitive belief that his pelvic floor was the culprit for his urinary symptoms and pelvic girdle pain. Before his initial assessment, he had done significant background research into the likely pelvic floor muscles that were causing his urinary symptoms. He began a stretching routine that he found on a pelvic floor physiotherapy website and did his own abdominal wall release work. This offered some relief but he was convinced that his pelvic floor muscles needed a specific and local release because he was still experiencing significant PGP and urinary symptoms.
Mr. B. also had an emotional component to his presentation that was centered around his abdominal wall gripping strategy. He was using this strategy to cope with anxiety, stress and frustration. He believed that these emotions were contributing to his pain and urinary symptoms.
Diane’s question
How will you structure your assessment to confirm/negate both the cognitive beliefs and the emotional component of his story and why is this an important thing to do for recovery?
Calvin’s response
It is important to clearly address Mr. B’s emotional and cognitive beliefs about his pelvic pain so that he is able to fully understand the relationship between his drivers and his experience of pain. Patient beliefs contribute to their narrative of the story of their pain experience. For Mr. B, his understanding of his pelvic floor pain from previous research was that his pelvic floor muscles were the cause of his symptoms. Given that his own understanding and the findings of his ISM assessment offered different explanations for his pain, a careful explanation of the relationship between his overactive pelvic floor and his cranial and thorax drivers was necessary. To corroborate the findings of the ISM assessment, Mr. B needed to feel a change in his pelvic floor with a specific pelvic floor assessment. This was done by identifying trigger points and then having Mr. B experience a release of these trigger points by correcting the drivers in his thorax and cranium. After experiencing this change in his body Mr. B was able to change his understanding of the underlying causes of his pelvic girdle pain.
Diane’s comment
Change the experience, change the belief!
Screening Tasks
Based on the meaningful tasks that were identified (standing and sitting), two screening tasks were chosen; the standing postural screen and the squat. The ISM approach was used to find the drivers that were responsible for producing non-optimal movement and neuromotor strategies for function. The screening tasks chosen were as follows:
Standing postural screen
The standing postural screen was important for Mr. B. as it was the body posture that he assumed while voiding urine. In 2007, Hodges P.W. et al. found that pelvic floor muscle activity was modulated by the abdominal wall muscles in quiet standing. They observed six female and one male subject’s pelvic floors in standing using surface EMG. They found that measures of intra-abdominal pressure recordings (using gastric pressure sensors and anal pressure balloons) were associated with changes in EMG recordings of the pelvic floor. Moreover, there were larger changes in the EMG recordings on expiration indicating that the action of the abdominal wall muscles impacts resting tone of the pelvic floor for the task of breathing while standing. From the findings of this study it is plausible that standing thorax and pelvic posture may impact the resting tone of the pelvic floor via the function of the abdominal wall muscles in breathing (particularly the external and internal obliques and diaphragm). If there is non-optimal alignment of the thorax or pelvis in standing there may be altered neuromuscular activation of the diaphragm and abdominal wall. This could result in changes in pelvic floor muscle tone in standing which may alter urinary function.
Diane’s question
Excellent hypothesis development here Calvin. What from the story so far (i.e. what specifically has he said about his urinary function) makes you suspect that there may be over-activation of the pelvic floor muscles in response to the abdominal ‘gripping’ habit he has developed?
Calvin's response
Micturition is a process that is controlled by both autonomic and somatic mechanisms (Fowler, 2008). The internal urethral sphincter and the detrusor muscle are under autonomic control. During the bladder’s filling phase, the parasympathetic innervation to the detrusor is inhibited, the muscle relaxes and there is closure of the internal sphincter. The striated urethral sphincter and bulbospongiosus are active under voluntary control and close the external sphincter. There can be increased pressure on the bladder when the abdominal wall is overactive due to increased intra-abdominal pressure. Persistent strain from gripping the abdominal wall may cause the feeling of urinary urgency which can trigger overactivity of the pelvic floor as a means to maintain continence.
There were no reported symptoms in standing when assessed. For optimal alignment in standing, there should be neutral rotation of the cranium, there should be no side-flexion or rotation of the neck when the gaze is straight ahead, there should be no rotation or side-flexion of the thorax, normal cervical and lumbar lordosis and thoracic kyphosis should be maintained. There should be no intra-pelvic torsion (IPT) or transverse plane rotation (TPR) of the pelvis, the sacrum should remain nutated relative to both innominates, and the femoral head should be centered in the acetabulum bilaterally.
On assessment of Mr. B.’s standing posture, the following was noted:
Functional Unit (FU) 1:
- Thorax: 9th thoracic ring (TR) translated left/rotated right
- Pelvis: transverse plane rotation (TPR) right, left SI joint unlocked
- Hips: Left femoral head forward compared to right
- Drivers for functional unit 1: Correction of the pelvis improved alignment of the left hip; however, no correction within the first functional unit improved alignment of the 9th thoracic ring or improved the patient’s experience in the task. Correction of the 9th thoracic ring did not improve the pelvis, nor hip. Based on these findings, the pelvis was considered the initial driver for the first FU; however, the 9th TR continued to be a level of ongoing interest.
Diane’s question
You note that the left SIJ was unlocked in standing, therefore this cannot be associated with an IPT but it can be associated with a TPR of the pelvis. Please explain the positional difference of all three bones of the pelvis between a right IPT and an unlocked left SIJ and why the two conditions cannot occur concurrently.
Calvin's response
Certain tasks require rotation of the pelvis as part of the optimal strategy for movement and sound load transfer. In these cases, normal movement of the pelvis may include the ability for the pelvis to move in a transverse plane rotation and an intra-pelvic torsion. These 2 motions most often occur congruently to the same side (i.e. a right TPR and right IPT). In a right IPT, the left innominate rotates anteriorly, the sacrum rotates to the right and the right innominate rotates posteriorly. The sacrum remains nutated relative to both innominates in this situation, that is, the left side of the sacrum is nutated relative to the left innominate and the right side of the sacrum is nutated relative to the right innominate. An IPT is a positional finding of the pelvis and is not in itself considered a problem. There is no loss of form or force closure of the pelvis in this situation. Conversely, when there is an unlocked left SI joint the sacrum is counternutated relative to the left innominate. This cannot occur when there is an IPT because an IPT requires the sacrum to be nutated relative to both innominates. There can be a TPR and an unlocked SI joint because the entire pelvic ring can be rotated to the left or right while one (or both) sides of the sacrum are relatively counternutated with respect to the ipsilateral innominate.
In the squat task, it is expected that the pelvis should undergo no TPR or IPT and that the sacrum should remain nutated bilaterally relative to the respective innominate as part of an optimal strategy for movement.
Functional Unit 2:
- Cranial: Intracranial torsion (ICT) right
- Cervical: C5 translated right/side-flexed-rotated left
- Drivers for functional unit 2: Correcting the cranium did not improve the alignment of C5. An articular system impairment prevented full correction of C5 and therefore the relationship between C5 alignment and the ICT could not be assessed. No driver was found within this functional unit. Ideally, C5 would have been mobilized first to determine its relationship to the cranium.
Relationship of Drivers between Functional Unit #1 (pelvis) and findings in Functional Unit #2: Correcting the pelvis did not improve C5 nor the cranium, nor as previously noted the 9th TR. Correcting the cranium partially corrected the TPR of the pelvis and resulted in improved control of the left SI joint (unlocked later in the task). The 9th thoracic ring did not change with the cranial correction and correcting the 9th thoracic ring did not improve C5 or the cranium. A co-correction of both the 9th TR and the cranium completely corrected both the alignment and control of the pelvis. However, because the articular system impairment at C5 was not mobilized, its relationship to the cranium and thorax was not determined.
Resultant drivers: Co-driver cranium and thorax (9th TR) and undetermined relationship to C5.
Diane’s question
Nice! What have you already determined about the underlying system impairment of the 9th thoracic ring and why?
Calvin's response
When considering the relationships between Mr. B’s areas of sub-optimal alignment, biomechanics and/or control, there was a clear connection between the cranium and the pelvis and the pelvis and the hip with the cranial correction partially improving the pelvis and thus hip. It is likely that there is a vector that connects these 3 areas. Correction of the cranium did not improve the 9th thoracic ring and the 9th thoracic ring correction did not have an impact on the pelvis, hip or cranium and was thus likely under the influence of a different vector. Mr. B was able to stack and align his 9th thoracic ring with a verbal cue which required influence of his motor cortex on the corticospinal tract to change the descending neural output to the muscles responsible for alignment of the 9th thoracic ring. As such, the vector was likely a neural system impairment affecting the 9th thoracic ring.
Diane’s question
Can you hypothesize on how a right ICT can unwind a right TPR of the pelvis – they are congruent and therefore not compensating directly for one another? What mechanism can you think of that would suggest a direct relationship here?
Calvin's response
The cranium is connected directly to the spinal cord via the attachment of the dura mater at the foramen magnum and through its extension to S2 via the arachnoid and pia mater to the conus medullaris and of the pia mater’s continuation as the filum terminale to the coccyx. If there is a twist in the system originating at either end of the dura mater there can be a congruent twist at the opposite end. Thus, taking the twist out of the cranium at one end takes tension away from the dura mater and removes the tension that was driving the twist in the pelvis.
Neuromotor patterns of the pelvic floor:
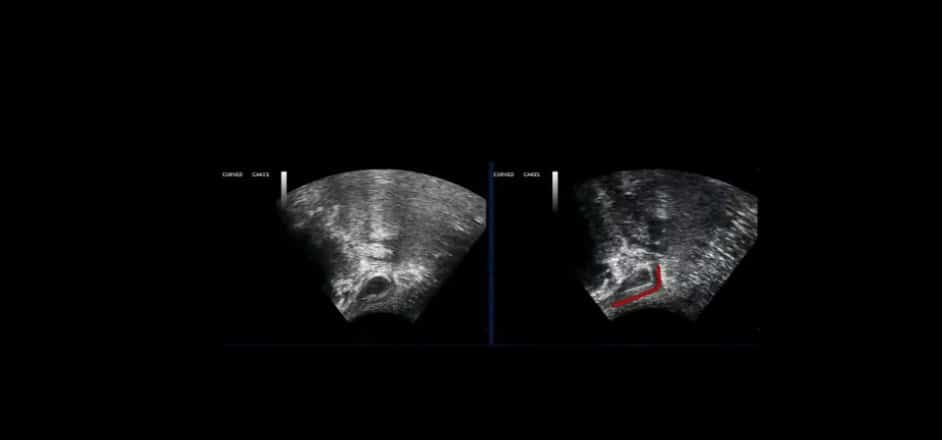
Symptoms of urinary frequency/urgency, post-micturition penile irritation and nocturia are sometimes related to the ability to the pelvic floor to close and open the urethra. Stafford et al. (2012) validated the use of transperineal ultrasound imaging as a measure to assess the ability of the bulbocavernosus and the striated urethral sphincter to maintain the continence mechanism. In order to determine the impact of whole body alignment on Mr. B.’s ability to recruit these muscles, ultrasound imaging was used to record activity of the bulbocavernosus and the striated urethral sphincter with and without the driver corrections that were found in standing. In supine lying, there were the same areas of sub-optimal alignment, biomechanics and control as in standing. Mr. B. was asked to perform a pelvic floor contraction, he noted the feeling of spasm and weakness which was reflected on ultrasound. The cranium was corrected and there was a significant improvement in the experience of perineal spasm and his ability to maintain the bulbocavernosus contraction was observed (Video of this provided – transperineal US of PF).
Diane’s question
Can you describe a biologically plausible mechanism that explains how ‘twists in the cranium’ can impact the recruitment strategy of the bulbospongiosus strategy and also define what you mean by ‘significant improvement.
Calvin’s response
The dura mater extends from the cranium to the distal end of the spinal cord and has attachment sites at both ends. Venous flow affects tension of the dura and this tension can affect distal extensions of the dura and its extensions to the peripheral nerves (as epineurium). The vasa vasorum are small arteries that provide blood to peripheral nerves and are sensitive to mechanical compression. Dural tension can cause tension or compression on the epineurium of peripheral nerves causing a change in function of the nerve as blood flow (and oxygen) from the vasa vasorum to the nerves are interrupted. An intracranial torsion can cause a change in tension along the dura and affect the exiting nerve roots (S2-4) that supply the pudendal nerve. This can impact the recruitment strategy of the bulbcavernosus by altering motor supply of the muscle from the pudendal nerve. The pudendal nerve’s sensory function would likely also be altered, and pain felt to the testicles, posterior scrotum, penis and anal canal are likely related to this change.
Diane’s question
Did the 9th thoracic ring correct fully in the supine position with the cranial correction? Can you describe an alternate mechanism that would suggest that the 9th thoracic ring (if it corrected) was more related to the change in bulbospongiosus as opposed to the cranium and how you would determine which was more important to address first?
Calvin’s response
When Mr. B was supine, the 9th thoracic ring was not fully corrected. Correction of both the cranium and 9th thoracic ring produced the best improvement to Mr. B’s ability to relax his pelvic floor and then activate and hold it without the experience of spasm. Mr. B was given stretch and release work for the external oblique and diaphragm and alignment cues for the cranium. However, even with the 9th thoracic ring improved, the cranial driver was still contributing to the experience of spasm and poor ability to maintain a pain free activation of the bulbocavernosus. In this case, it would be important to first address the cranial driver (the cranium) because the sub-optimal alignment/biomechanics at the 9th thoracic ring would likely always return as a non-optimal strategy to compensate for changes to the pelvic floor from the cranium.
The 9th thoracic ring could be related to the change in bulbocavernosus by its effect on intra-abdominal pressure (IAP). When there is overactivity of the abdominal wall (i.e. the external oblique) the pelvic floor can react by contracting. Correcting the9th thoracic ring could improve overactivity of the external oblique, reduce the IAP and improve the ability of bulbocavernosus to achieve a contraction without reactive spasm.
Diane’s response
Exactly what I was looking for!
Deep squat
The deep squat was used to assess early, middle and late stage strategies for moving into and out of a sitting posture.
During an optimal squat the thoracic rings should remain aligned and in neutral rotation, the lumbar spine should remain neutral with preservation of the lumbar lordosis, there should be no pelvic TPR or IPT and the sacrum should remain nutated relative to the innominates. The femoral head should seat (remain centered) in the socket of the acetabulum bilaterally, the neck may extend without side-flexion or rotation of the cervical vertebrae as the individual’s gaze may stay looking forward during the squat. The occiput may posteriorly rotate (anterior glide of the convex surface of the occiput) on the atlas bilaterally to maintain forward looking gaze, and there should be no intracranial torsion during the movement – the temporal bones, sphenoid and occiput should remain neutral.
During Mr. B.’s squat the following findings were noted:
Functional Unit 1:
- Thorax: 9th TR translated left/rotated right
- Pelvis: TPR R, L SIJ unlock
- Hips: L femoral head forward
- Driver for FU 1: There was no best correction of the squat in the first FU, and it was noted that no correction improved alignment, biomechanics or control (ABC) of the 9th TR. Correcting the pelvis improved alignment of the L femoral head. Based on these findings the pelvis was considered the driver for this functional unit; however, the 9th TR was noted as a site of interest as no correction improved its alignment.
Functional Unit 2:
- Cranium: ICT Right
- Cervical: C5 translated right/ side-flexed-rotated left
- Driver for FU 2: An articular system impairment prevented full correction of C5 and therefore the relationship between C5 alignment and the ICT could not be assessed. Correcting the cranium did not improve the alignment of C5 therefore no driver was found within this functional unit. To determine the relationship between the C5 and the cranium the articular vector affecting C5 would first have to be mobilized.
Relationship of Drivers between Functional Unit #1 and findings in Functional Unit #2:
Correcting the cranium improved the alignment of the pelvis and control (no L SI unlocking until later in the task), and the left hip also improved. The 9th thoracic ring still translated left/rotated right with the cranium corrected. A co-correction of the cranium and 9th thoracic ring was done to see if adding a 9th thoracic ring correction would improve late stage left SI joint control. With a correction of the cranium and alignment cues for the 9th thoracic ring, control of the left SI joint was restored in the late stage of the squat. Since a co-correction of the cranium and 9th thoracic ring was needed to produce the best improvement to alignment, biomechanics and control in the task, the cranium and thorax were considered to be co-drivers, however the influence of C5 remained not determined for this task.
Diane’s response and question
Excellent reasoning of the relationship between the two unit drivers.
I’m wondering about the relationship between this 9th thoracic ring and the abdominal wall – did you assess the EO IO TrA response via ultrasound with a cranial vs 9th thoracic ring correction? Considering the nerve supply to the abdominal wall, and the known response of the pelvic floor to increased IAP when the EO excessively activates – I’m curious if this was a player in this story?
Calvin's response
Considering that the 9th thoracic ring correction helped improve Mr. B’s ability to relax and connect to his pelvic floor, the abdominal wall was likely a player in his story. In the same way that Mr. B had multiple factors that played into his pain experience he also had multiple drivers and mechanisms that contributed to the function of his pelvic floor. Initially, a correction of both the cranium and the 9th thoracic ring was required to produce the best relaxation and activation of the bulbocavernosus on ultrasound. The 9th thoracic ring was likely driving the pelvic floor overactivity at rest and also the inability to maintain a contraction of the pelvic floor when cued. The cranium was likely also contributing to this altered motor control via its effect on the pudendal nerve. As treatment sessions progressed, Mr. B was able to change his 9th thoracic ring by improving his standing posture and bringing awareness to letting his gripping strategy go. The external and internal obliques are innervated by the intercostal nerve (T7-11) and the subcostal nerve (T12). The transversus abdominus is innervated by the intercostals nerves (T7-11), iliohypogastric and ilioinguinal nerves. Considering the common innervation of the abdominal wall and the known relationship between increased IAP and the pelvic floor it is possible that there was also altered recruitment patterns of the transversus abdominus and IO. This was not evaluated on ultrasound, however considering the loss of control of the left SI joint in the squat task it may be plausible to assume that there was a failure of the force closure mechanism of the pelvis and potentially altered activation of the TrA and IO. There are many factors that can contribute to the force closure mechanism of the pelvis. However, in Mr. B’s squat task, adding a co-correction of the 9th thoracic ring to the cranial correction was required to restore control to the left SI joint. Thus it may be that correcting its alignment changed the abdominal wall activation strategy that was a contributing factor in both force closure of the pelvis and reactivity of the pelvic floor.
Further assessment of the cranium to determine underlying system impairments
Further assessment of the cranium was done to determine the underlying system impairment for this driver using active and passive mobility tests with active and passive listening during both the correction and release of the correction.
- Positional findings for a right ICT: there was a right rotation of the occiput, the right temporal bone was posteriorly rotated, the left temporal bone was anteriorly rotated and the sphenoid was right rotated in the transverse plane.
- Active mobility was assessed by noting the ability of the right temporal bone to rotate anteriorly, left temporal bone to rotate posteriorly and the sphenoid to rotate to the left with left head and neck rotation (vice versa for the right). Part of the cranial region includes the occipito-atlanto (OA) joint. Cranio-cervical side-flexion can be assessed to note active mobility of side-flexion with the conjunct contralateral rotation.
- Passive mobility was assessed by noting the ability to de-rotate the occiput to neutral on C1 and then passively de-rotate the temporal bones. The sphenoid was observed (via position of the orbits) to follow the temporal bones back to neutral rotation. During this correction, passive listening was used to note any resistance to the correction.
- Passive Listening after release of the correction: Release of the R ICT correction, there was first an immediate rotation of the occiput to the right followed by the temporal bones, left anterior and right posterior. There was a long slow posterior vector felt down along the spine extending to the sacrum. This was felt to be a dural vector and a neural system impairment.
Diane's Question
Is the sphenoid rotation congruent, or incongruent to the ICT? Why is this important to know?
Calvin's response
The sphenoid rotation was congruent with the temporal bones and occiput in this case. This is important to know as an incongruent sphenoid rotation may indicate a vector within the cranium. When assessing for vectors within the cranium a cerebellar falx spring may be used to identify vectors affecting the congruent motion between the temporal bones and sphenoid. Tension in the cerebellar tentorium can restrict congruent motion between the temporal bones and sphenoid via its attachment to the petrous portion of the temporal bones and the clinoid process of the sphenoid. Alternatively, there can be a situation in which a vector arising external to the cranium causes an ICT of the occiput and temporal bones while an intra-cranial vector concurrently causes a rotation of the sphenoid in the opposite (incongruent) direction. In both scenarios, the therapist must use a combination of cranial listening techniques and clinical reasoning to determine the vector(s) causing the cranial torsion and the most appropriate treatment technique.
Diane's Question
At the moment, the dura is in the myofascial piece of the clinical puzzle, but I’m not sure it belongs there after the course we did with Christoff Sommer and the role the venous system plays in tension in the dural membranes in the cranium. I think the same can be true for the impact of the venous system on tension in the various dural layers in the spinal canal. Did you classify this as a neural system impairment for another reason? I’m still struggling to ‘fit’ the dura somewhere so your thoughts would be helpful.
Calvin's response
As highlighted by Christoff, the dural venous sinuses empty blood into the internal jugular vein. Adequate venous drainage is required to maintain pressure balance in the brain. As Christoff points out, an increase in arterial pressure may not impact tension in the dura of the brain because the venous system can adapt, however, poor venous drainage may cause an increase in CSF and increased intracranial pressure causing tension in the cranial dural membranes. The same can be true for the continuation of the dura mater into the spinal cord as CSF flows into the subarachnoid space. Changes in CSF pressure can impact the tension along the length of the dura to the conus medullaris, this dural tension can be carried through the extension of the pia mater as the filum terminale to the coccyx. The same can also be said for the extensions of the dura mater to the peripheral nerves. As the nerve root exits the spinal canal via the intervertebral foramen, the dura becomes continuous with the epineurium. This continuity of length allows tension in the dura to affect the nervous system to the extremities via the epineurium covering the peripheral nerves. According to (Barral, 2008), the vascular supply to the peripheral nerves is via the epineurium which carries veins and arteries (vasa vasorum). It is known in the literature that mechanical compression of the vasa vasorum can cause nerve ischemia and result in peripheral nerve symptoms (Griffin, 2001). This may explain the mechanism by which tension in the dura can affect distal regions of the nervous system as far as the peripheral nerves.
While the dura is histologically considered fibrous connective tissue, its greatest impact on function (optimal load transfer) is through its direct effect on peripheral nerves and the impact of the nervous system on whole body movement. Furthermore, considering the impact of the venous system on maintaining tension on the cranial tentorium and the role this plays in regulating tension of the dura mater, it may be appropriate to classify the dura as a nervous system vector.
Further assessment of the 9th thoracic ring:
- Positional findings for a left translated/right rotated 9th TR: anteriorly rotated left 9th rib and posterior/medial/superior (PMS) glide of the left costo-transverse joint (CTVJ), posteriorly rotated right 9th rib and anterior/lateral/inferior (ALI) glide of the right CTVJ, T8 is right rotated-sideflexed on T9.
- Active Mobility: using breathing to assess mobility of the costal joints, there was reduced ALI glide and posterior rotation of the right 9th rib, and on exhalation there was reduced PMS glide and anterior rotation of the left 9th rib. These asymmetries in active mobility were due to the left translated/right rotated position of the 9th TR. Seated segmental flexion, extension and side-flexion of the T8/9 spinal segments are determined by palpating and left and right transverse processes and noting symmetry of superior glide for flexion and inferior glide for extension. There should be ipsilateral inferior glide and contralateral superior glide for side-flexion. These spinal motions are available if there is no articular vector restricting active motion.
- Passive Mobility: the 9th TR was passively corrected by taking the left 9th rib into posterior rotation and the right 9th rib into anterior rotation. The quality and quantity of motion was noted as the left and right CTVJ’s were able to fully move back to a neutral position. Passive articular joint glides assessing PMS and ALI glides could have also been used to assess the passive mobility of each CTVJ and spinal facet joint at the T8/9 level; although if done when TR 9 was translated left/rotated right a false positive finding may be noted. Thus the importance of determining whether the TR9 could be corrected. When there is an articular system impairment, the alignment of the thoracic ring can not be completely corrected.
- Passive listening noted during release of a correction of TR 9: a drawing of the left 9th rib forward and into anterior rotation and then a short anterior and inward tip, this was felt to be a neural system impairment caused by overactivation of the left external oblique and left anterior portion of the diaphragm. Overactivation of primary muscles of respiration made sense with Mr. B.’s story that included a long history of breath holding and abdominal wall gripping.
Initial Session (RACM)
During the initial assessment, Mr. B. was educated about the connection between the cranium, thorax and pelvic floor. He was unable to move beyond his cognitive belief that his pelvic floor was the culprit because of his own research findings previous to his initial assessment. It was determined that his cognitive belief was a barrier to treatment during the first appointment. To remove this belief, a physical assessment of the external pelvic floor was conducted. Palpation of the first layer of the pelvic floor was done to locate trigger points and identify their referral points to the tip of the penis and testicles. Mr. B. was instructed to practice manually stacking his 9th thoracic ring while verbal cues to create space behind the skull and elongate the spine were used to correct the cranium. Mr. B. was then able to feel a “release” of tension in his pelvic floor and specifically helped to create a release of trigger points in the bulbocavernosus and transverse perineal muscles. Having Mr. B. feel a change in his pelvic floor tone by correcting his cranial and thorax drivers helped him change his cognitive beliefs about his pelvic floor.
Diane's question
So, here you’ve nicely answered some of my first questions! Why do you think that merely explaining ‘connections’ and ‘relationships’ didn’t ‘change his mind’ whereas changing the experience in his body did? Tell me a bit about your understanding of Melzack’s body neuromatrix that may help others reading this case report understand why ‘explaining’ things can have a different outcome than experiencing things change in our bodies.
Calvin's response
In 1965 Ronald Melzack and Patrick Wall published their joint paper describing the Gate Control Theory of Pain. This theory was novel for the time and became the basis for the understanding of pain in the 1970’s. It was the underlying mechanism for which electro-therapeutic agents such as TENS became important tools for therapists in the treatment of acute and chronic pain states (Melzack, 1999). Melzack’s Gate Control Theory introduced the novel concept that the brain could contribute to the pain experience contrary to the widely accepted Cartesian understanding of pain as being purely related to tissue injury and inflammation.
Melzack later developed the concept of a “Neuromatrix of Pain” which further defined the brain’s contribution to the pain experience. Under this new theory, Melzack introduced the concept of the Body-Self Neuromatrix in which the body (as we feel and experience it) is generated by a series of brain mechanisms that work together to generate a “neurosignature pattern of the whole body”. This neurosignature creates our sense of self and is affected by inputs from the body (i.e. peripheral nerve signals) but can be present in the absence of inputs (Melzack, 2001).
Inputs to the Body-Self Neuromatrix include:
- Cognitive-Evaluative inputs which include tonic input from the brain (including cultural learning and past experiences) and phasic input (anxiety, depression and expectation)
- Somatic input (visceral, somatic – trigger points, visual and vestibular inputs)
- Motivational-Affective inputs (limbic system, cytokine and immune system inputs etc.)
With this understanding in mind, it is clear the Mr. B’s experience of pain was likely multidimensional in nature. Thus, when addressing his pain experience, it was important to consider the multitude of inputs that were influencing his body-self neuromatrix. Merely explaining the origin of his pain would only address one of the potential multitude of inputs to the body-self neuromatrix and therefore fail to change his pain experience. In clinical practice it has been acknowledged that affecting the body-self also known as the “virtual body” may be accessed (though not exclusively) through the corresponding body tissues (Moseley, 2003). As such, the act of palpating the perineal trigger points while correcting his cranial and thoracic ring drivers changed his cognitive expectation and understanding about his pain as well as changing somatic sensory input. Cueing Mr. B to breath into his ribcage and relax his perineum further allowed him to access his cognitive-evaluative system to reduce the influence of anxiety and fear. Together, these changes produced a change in his pain experience by changing the inputs to his body-self neuromatrix.
During his second treatment session, Mr. B. was ready to further explore the connection between the cranium and thorax and his pelvic floor. During this session, the RACM treatment model was used:
R: Co-Driver: Cranium – unwind the cranial torsion with the patient in crook-lying and with the pelvis in neutral resting position and wait for a dural vector release, then take the pelvis into rotation by letting the knees drop to the left and wait at the point of further tension. Once a release is felt, take the knees further into the release until no resistance is felt to the cranial correction.
Co-Driver Thorax: Stretch with Awareness release of the overactive fascicle of the left external oblique to the left 9th rib of the 9th thoracic ring and a Release with Awareness of the anterior fibres of the diaphragm on the left.
A: Alignment cues were given for the cranium. Because the dural vector felt like a shortening from the occiput down to the sacrum, alignment cues were to elongate and create space behind the skull and take that length toward the ceiling feeling length all the way down to the tailbone. There was also a cue to breath laterally into his low ribs and allow space to arise between the intercostal spaces above and below the ninth thoracic ring. An alignment cue incorporating breath was especially important because Mr. B.’s story included a component of gripping and holding of his abdominal wall that was related to poor breathing patterns.
C: Correcting the 9th thoracic ring improved control of the left SI joint in the squat task so no specific connect cues were needed to control the pelvis.
Diane's question
Were you able to witness a change in his abdominal wall recruitment strategy on ultrasound with this cuing? If not, what do you suspect was present with the 9th thoracic ring shift and what may have changed that influenced his left SIJ control with the improved alignment?
Calvin's response
The abdominal wall recruitment strategy was not observed on ultrasound during the assessment before and after a thoracic ring correction. However, it is likely that with a left translated/right rotated 9th thoracic ring there was overactivation of the left external oblique and diaphragm muscles. This is likely correlated with his subjective description of abdominal wall gripping and poor breathing patterns. It is common to find that individuals with dominant abdominal oblique muscle neuromotor strategies may also have delayed transversus abdominus activation patterns (a non-optimal strategy for movement). Improving alignment of the 9th thoracic ring changed the neuromotor strategy of the external oblique and diaphragm muscles used in the squat task. This was reflected in improved control of the left SI joint as a more optimal strategy for movement was restored.
When the cranium was corrected Mr. B. was able to relax his pelvic floor, and connect to his striated urethral sphincter and bulbocalvernosus by thinking about “shortening the penis”. He was able to hold this activation strongly, without spasm and without reported fatigue once his pelvic floor was able to relax fully.
M: Using the above alignment cues in standing (while voiding urine) and in the squat/sitting task.
Follow-up treatment sessions
During the following treatment sessions, Mr. B. was able to let his overactive pelvic floor muscles relax by practicing his alignment cues in standing and supine while incorporating lateral costal and belly breathing. Once Mr. B. was able to keep the pelvic floor relaxed, he experienced improved ability to void his bladder without penile irritation, he was also able to return to sleeping through the night without having to wake to void urine. Mr. B. was instructed to practice keeping cranial and thorax alignment when sitting at home while carving pumpkins and while at work. Mr. B. has just had his 7th treatment session. At this time, he is still working on maintaining optimal sitting posture. He experiences occasional flares of his penile pain when he sits for prolonged periods of time. His thorax alignment is better in his standing and squatting task; however, he is consistently having to cue alignment of his cranium to improve his PGP symptoms and occasional flare-ups of penile irritation. He also mentioned that he was still struggling with aggravation of arm paraesthesia and muscle twitching after doing arm movements over his treatment table at work and when holding his cellphone.
On assessment, his arm was taken into median and radial nerve tension positions as well as his cellphone holding posture. These produced symptoms of muscle twitching that he described as fasciculations. His cranial right ICT and his left side-flexed/rotated C5 got worse with wrist extension. Mr. B.’s thorax was better aligned in standing and sitting. His C5 was difficult to correct potentially because of the cervical disc injury and made no change to the arm movement task. The cranial correction produced only a small change to the experience of paraesthesia and twitching into the arm and did not improve alignment of his C5. It is likely that a co-correction of the cranium and C5 would be needed to produce a full unwinding of the dural vector causing sub-optimal alignment of both the cranium and C5. In an ideal situation, 2 therapists would be present to co-correct the drivers and assess the response in the meaningful task. However in lieu of a second therapist, an alternate method was used to test the hypothesis that the dural tension between the cranium and C5 was causing nerve tension down the right arm. The cranium was corrected and it was taken into left rotation in line with C5. This was thought to unwind the dura mater between the occiput and the C6 nerve root (exiting through the intervertebral foramen at C5/6). Since this correction made the greatest change to the arm movement task, it is likely that there is a secondary driver (C5) and restoring proper alignment to both areas (cranium and C5) will be necessary to improve function in the right arm and prevent recurrence of the cranial torsion.
Diane's response
Very well explained. Could you correct C5 independent of the cranium? Given his history, what could the underlying system impairment be that would prevent correction for finding a driver?
Calvin's response
On assessment, it was difficult to correct the C5. Given the history of the MVA in 2016 and the posterior disc protrusion on MRI it is possible that there was an underlying articular system impairment preventing correction of the C5 vertebra, specifically a change in the orientation and tension of the annular fibres of the intervertebral disc between C5/6.
Next Steps
At the end of the last session, Mr. B. was left with a supine lying cranial alignment exercise to practice with arm movement into the positions of nerve tension that we explored during the session. He was able to find a reduction in symptoms using cues to create space behind the neck and reach the back of the head long. At his next session, we will explore control cues for C5 with integration of his cranial alignment cues for his right arm movement tasks.
Diane's response
What from your assessment of C5 so far led you to believe there was a control problem at C5 vs a mobility problem? There is no mention of what C5 did with the corrections in standing, and it didn’t change in the squat task. I can’t find any other segmental assessment of C5 to understand how you determine that control was an issue as opposed to mobility. How did you differentiate the two?
Calvin's response
As the role of C5 became more apparent in subsequent treatment sessions, a segmental assessment of C5 was done to determine whether there was a control or mobility issue affecting C5. This included assessment of the passive intervertebral movements of the C5/6. For left rotation, the U-joint between C5 and C6 must extend on the left and flex on the right, the left z-joint must glide in an inferior, medial and posterior (IMP) direction and the right z-joint must glide in a superior, anterior and lateral direction (SAL). It was found that there was less neutral zone felt in the left IMP and the right SAL. Considering the positional finding of the C5 vertebrae left side-flexed and rotated, it would be expected that there would be a change in the neutral zone felt in the left IMP and right SAL PIVM’s. In supine, the C5 was taken into a right rotation and side-flexion following the plane of the joints (C6 fixed and C5 moving) relative to its resting position to facilitate assessment in a neutral position, however, there was a very local and specific resistance to the correction in the supine position with the muscles of the neck relaxed. This resistance was felt to arrive early in the correction between the C5 and C6 vertebrae. It was felt to be the intervertebral disc at the C5/6 level, this was considered an articular system impairment because the intervertebral disc is considered to be an intrinsic component of the 3-joint complex of C5/6 motion segment. In this case, mobility of the C5/6 segment was restricted. Based on the motion segment assessment, Mr. B would actually require alignment cues for his C5 to promote improved postural alignment despite the change in tension of the annular fibres of the C5 disc. In future sessions, specific PIVM mobilizations could be used to improve the mobility of the 3-joint complex at the C5/6 segment.
Diane's response
Perfect!
As Mr. B.’s story continues to unfold there has been a continual change in his symptoms and areas of sub-optimal performance. Some areas have improved (his 9th thoracic ring, and pelvis and hip alignment and left SIJ control) and others have remained present (his cranium and C5). As the layers of dysfunction in his body change, different drivers arise and need to be addressed. As his sessions continue, the focus on improving alignment, biomechanics and control of the cranium and C5 will lead to integration into sitting and standing tasks to restore function and resolve his remaining persistent symptoms of PGP and penile irritation.
Skills Demonstration
Case Study Author
Clinical Mentorship in the Integrated Systems Model
Join Diane, and her team of highly skilled assistants, on this mentorship journey and immerse yourself in a series of education opportunities that will improve your clinical efficacy for treating the whole person using the updated Integrated Systems Model.
We will come together for 3 sessions of 4 (4.5) days over a period of 6-8 months with lots of practical/clinical time to focus on acquiring the skills and clinical reasoning to put the ISM model into practice. Hours of online lecture and reading material and 12 hours of in-person lecture are...
More Info