Story
Ms. C, a 67-year-old retiree, first presented to the clinic in early 2022. She is an equestrian who has competed internationally and has been training ever since she was a child. She competes specifically in dressage, a form of horseback riding that requires a harmonious demonstration of skills between the rider and the horse, while performing various gaits and movements (St George et al., 2022).
Ms. C has two meaningful complaints: left sided sacroiliac joint pain and difficulty sensing when her bladder requires emptying. She was advised by her medical team to attend physiotherapy as it will be beneficial. Her bowels are functional. She has regular bowel movements every day and only describes periods of constipation during travel.
Two years ago, Ms. C fell off her horse while riding and both her and the horse fell. The horse rolled over on top of her chest and upon trying to return to an upright position, the horse stepped on her lower neck and upper ribcage. As a result of this accident, Ms. C suffered the following injuries:
- Multiple rib fractures bilaterally (does not recall which ribs specifically)
- Compound fracture in left humerus
- Right punctured lung
- Bilateral collapsed lungs
- Bilateral clavicular fractures
Prior to the accident, Ms. C reports a normal voiding schedule and sensation for her bladder. As a result of her injuries, Ms. C began developing bladder infections due to the urine staying in her bladder for long periods of time. Recently, about six months ago, the bladder infection spread to her kidneys for a second time.
Diane’s question:
At this point, what are you thinking is the link, or mechanism, between an injury to the upper thorax and lungs and her bladder’s lack of sensation for the need to void?
Brittany’s response:
My initial thought was the impact to the fascial system of the thorax and large surface area that was affected from the trauma may be affecting the proper mobility of the tissues around the bladder, along with bladder motility. I also suspected that the trauma of the incident may have affected the communication between the brain and bladder, altering the reflex the bladder sends to the brain once its ready to be emptied.
Diane’s comment:
I also wondered about a change in homeostasis of pressure management since the thorax is a huge regulator of pressure both for the cranium, abdominal and pelvic canisters.
Ms. C is a very active individual and also enjoys cross country skiing in the winter months. She has sustained the following injuries in her past:
- Fractured left radius and ulna while skiing (Jan 28th 2022), and had a surgical repair (Feb 10th 2022)
- Torn left ACL and fractured tibial plateau (2018)
- Fractured left ankle (distal tibia) and tore all ligaments surrounding lateral malleolus from dismounting horse (2010)
Ms. C is healthy and does not have any other previous medical concerns. A bone density test was completed after the history of fractures, in which there were no concerns.
Diane’s questions:
Does Ms C have any children and has she had any abdominal surgeries in her medical history?
Brittany’s response:
Ms. C has not had any abdominal surgeries and does not have any children.
Meaningful Complaint
Ms. C reported two meaningful complaints at the time of assessment:
- Left sided sacroiliac joint pain – She states that the pain comes on after riding the horse and she does not experience any pain while sitting on the horse.
Diane’s question:
Has Ms. C noticed any pattern to the length of time she sits on her horse to the pain onset. In other words, is this a dosage problem such that if she limits the time on the horse the pain doesn’t arrive after, or does it always arrive regardless of length of time on the horse. Why is this information key for treatment planning?
Brittany’s response:
Ms. C has not noticed any pattern to the onset of pain. She gets pain after sitting on the horse, regardless of the length of time she has been sitting. This is important for treatment planning because it can help differentiate between neuropathic, nociceptive and nociplastic pain responses.
Diane’s question:
There are 3 phenotypes of pain. Can you name them, describe the symptom/behaviour qualities of each and then state which phenotype you consider Ms C’s pain to be and what features from her story support your choice.
Brittany’s response:
There are three different phenotypes of pain as follows:
- Nociceptive pain occurs when there is actual or threatened damage to a non-neural tissue such as bones, ligaments, muscles and tendons. This typically occurs from nociceptors activated in the peripheral tissues in response to a chemical, mechanical or thermal stimulus. An example of this would be when you touch the top of a hot stove and you get a burning sensation on your finger that makes you quickly withdraw your hand.
- Neuropathic pain occurs where there is an injury to the nervous system, or the neural structures within the body. It can feel like a sharp, shooting or burning pain along the distribution of the specific nerve. An example of this is when you compress a nerve in your arm while sleeping on it and you feel the numbness and tingling sensation along the length of that nerve.
- Nociplastic pain arises when the nervous system becomes sensitized. Nociceptors fire in the absence of an actual threat or injury to the tissue or nervous system. This type of pain does not typically change throughout the day in response to activities and rest and can remain constant. It is also characterized by a widespread pain and can have a strong association with factors such as levels of high stress, anxiety and negative emotions.
Ms. C’s pain falls into two categories: nociceptive and nociplastic. Her experience of getting pain after sitting on the horse is mechanical in nature, especially as it occurs every time and specifically with that task. However, as the pain has been ongoing for greater than three months, there is an element of central sensitization or upregulation of the tissues, which would fall under the category of nociplastic pain.
Diane’s comment:
While the formal classification of nociplastic pain would agree with your answer relating to the timeline of nociplasticity, I have seen patients in clinical practice who have had pain for longer than 3 months and their phenotype is totally nociceptive with no sensitization so I’m not sure they’ve nailed this classification yet!
Diane’s question:
What does the latent, or delayed, pain response suggest here?
Brittany’s response:
The latent pain response suggests that the pain may be attributed to a neuropathic pain mechanism. There is still a mechanical stressor of sitting on the horse, but it takes time for the pain to present itself, therefore involving the nervous system.
Diane’s question:
Hm… yes but it feels like you have merely described the response and not explained it. Why does it take time for the pain to present itself? What is happening physiologically in the body in that a delay is required for pain to occur?
Brittany’s response:
There are many factors at play when it comes to a patient’s experience of pain. According to Butler (2000), the mechanisms can be differentiated between peripherally mediated mechanisms (such as peripheral neuropathic pain and nociception) and centrally mediated pain (related to the central nervous system). The processing occurs within the central nervous system and the dorsal root ganglion (Lee, 2011).
In a study from Taylor & Corder (2014), it was found that tissue inflammation can lead to a latent pain response in the body, as it takes time for the inflammation to occur and build, requiring a delay in the occurrence of pain.
Diane’s comment:
Yes that is the answer I was looking for – inflammation!
- Decreased ability to sense when the bladder is full leading to chronic urinary tract infections (UTIs).
Cognitive and Emotional Beliefs
Ms. C was not sure what was causing her pain but believed it came from her accident and the physical injuries her body experienced. She believed that although she had worked with other therapists in her past, they were only treating symptoms and not getting to the root cause of her problem. She believed the left sided pelvic pain was most likely referred from somewhere else in her body, but was unsure from where.
Diane’s question:
Given that this pain pattern has been present for two years, there is likely an emotional dimension to her experience. Did you get a sense of any emotional considerations that would need to be addressed as part of treatment?
Brittany’s response:
When Ms. C was describing her story and I asked her what she thought was going on, she seemed to think it was very mechanical and was originating in another area of her body after her traumatic fall off the horse. I did not get a sense of any emotional considerations when discussing the story with her; however, a pain that has been present for longer than three months can include some central sensitization.
When assessing Ms. C, I made sure to educate her on what we were doing and describe the interaction of different body areas with one another and relate it back to the primary driver. I also discussed that the pain around her SIJ that she was experiencing, may not be the source of the pain and instead be the reactor tissue in the body.
Meaningful Tasks
Ms. C reported one meaningful task during the initial assessment:
- Sitting on horse (squat position with straight back, arms bent at side and looking straight ahead)
Screening Tasks
There is one screening task to assess for Ms. C:
- Squat task (to mimic sitting on the horse)
Standing Screen
A standing start screen was assessed first in order to determine the body’s starting position before moving into her main task of sitting on the horse. In clinical practice, it is expected to find incongruencies within the body. It is important to assess where the body is in the starting screen position in order to determine the relationship between the incongruencies in the body when we compare the start screen findings to the screening task.
Diane’s question:
You note that ‘it is expected to find incongruencies within the body’. Can you define what you mean by incongruencies in this statement?
Brittany’s response:
I feel that I misworded that sentence. In clinical practice, I often see a variety of presentations within the body. It is normal to find small differences between body areas. We live in our bodies and therefore our day-to-day activities influence the findings that I see in practice and we are never expecting perfect symmetry. What is most important is that we assess to see which findings are actually important and which are ones that we can leave and carry on. For example, if someone has a right pelvic rotation in the transverse plane, and we correct that and it improves other body areas and their task at hand, then we will go ahead and further assess the pelvis. We are also assessing to see which areas of the body may be incongruent to the demands of the task. If we correct the pelvis and it makes other findings worse, or has no effect at all on other body areas, then we will leave it and move on to another area of greater importance.
Diane’s further question:
Recently, the word ‘correction’, that we use all the time in ISM, has been challenged. Some state that we are judging a positional finding and that there is no evidence to suggest that any positional change is not always relevant. Above, you state “that we assess to see which findings are actually important and which are ones that we can leave and carry on. For example, if someone has a right pelvic rotation in the transverse plane, and we correct that and it improves other body areas and their task at hand, then we will go ahead and further assess the pelvis”. There is a big piece missing in this statement that we also do, so that we are not only biomechanically ‘judging’ a correction, or change’ – what is it and how does it inform whether we ‘can leave and carry on’?
Brittany’s response:
Good point! The part I left out here is the patient’s experience. When we are assessing a change or correction, a big piece of this is how it feels to the patient in their body and how it affects their task. When they give me the feedback that their task feels much easier and I get that “wow” from them, then I know that we are on the right spot and we can go further assess that area.
Diane’s comment:
Exactly, we let the patient’s nervous system be the judge of any change in biomechanics, alignment and/or control of any body region.
Functional Unit #1
Pelvis: right transverse plane rotation (TPR) with a congruent right intra-pelvic torsion (IPT)
Hips: Left hip anterior to right
Thorax: 3rd thoracic ring translated left and rotated right, 4th thoracic ring translated right and rotated left; 7th thoracic ring translated left and rotated right, 8th thoracic ring translated right and rotated left. These rings are not glued and can move independently of each other.
Lumbar spine: Neutral lordosis observed. L5 is right rotated.
Summary of congruencies & incongruencies in FU#1: The pelvis and hips are congruent with each other. Given the right TPR, the left hip is expected to be anterior to the right. TR3 is in a right rotation, which is congruent to the pelvis and TR4 is in a left rotation which is incongruent. Similarly, TR7 is right rotated which is congruent to the pelvis, and TR8 is left rotated which is incongruent.
Diane’s question:
TR3 is right rotated and TR4 is left rotated – is this congruent or incongruent?
TR7 is RR and TR8 is LR – same question? This sentence “The 3rd and 4th thoracic rings, along with the 7th and 8th thoracic rings are congruent with one another” suggests that all of these thoracic rings are rotating in the same direction, and they are not.
Brittany’s response:
The pelvis is in a right TPR and the 3rd thoracic ring is also right rotated, making the 3rd thoracic ring congruent to the pelvis. The 4th thoracic ring is left rotated, which is incongruent with the pelvis.
TR7 is also right rotated, which is congruent with the pelvis, and TR8 is left rotated and is incongruent with the pelvis. Therefore the 3rd and 4th thoracic rings, along with the 7th and 8th thoracic rings are not congruent with one another as they are not all rotating the same way.
Diane’s question:
In ISM there are two uses/definitions of the word congruent. What are they?
Brittany’s response:
The word congruent can be used as above where the 3rd and 7th thoracic rings are right rotated which is congruent with the right rotation of the pelvis in the transverse plane as they are all rotating in the same direction. A congruency can also be task specific, which may not require all areas to the rotate in the same direction, it entirely depends on the demands of the task.
Functional Unit #2
When Ms. C fell off of her horse, she hit her head and lost consciousness. She also experienced broken ribs and clavicles, so there has been significant impact and trauma to functional unit #2. For this reason, it is important to assess these areas.
Cranium: left intracranial torsion (ICT), congruent sphenoid
Diane’s question:
Which way is the sphenoid rotated if it is congruent with the LICT?
Brittany’s response:
The sphenoid should be in a left rotation if it is congruent with the L ICT.
Thorax: 2nd thoracic ring translated left and rotated right (congruent with the 3rd thoracic ring of FU#1)
Cervical spine: C2 translated right, rotated left; C6 translated right, rotated left
Shoulder girdle: left shoulder girdle downwardly rotated and anteriorly tipped, head of humerus centred bilaterally, right clavicle compressed medially
Summary of congruencies & incongruencies: C2 & C6 and the cranium are all congruent with one another, but are incongruent to the findings of the 2nd thoracic ring.
Incongruencies:
The findings of a walking cranium and TR2 infinity sign are incongruent with the other findings. In FU#2, C7 and C1 are incongruent with C2 to C6 and TR1
Functional Unit #3
I did not assess Functional Unit #3 as the feet are non weightbearing in the task and are instead resting in stirrups.
Diane’s comment:
I’m not convinced that the feet are not weightbearing in this task – I think the forefoot is and the forefoot may be influenced by the hindfoot which could have some residual impact from the left ankle fracture in 2010 or the tibial plateau fracture in 2018. Did the left foot or knee ever come into the clinical picture?
Brittany’s response:
If I were to redo the assessment, I would have further assessed her foot in the task. I originally thought that the feet were not a part of the clinical picture for this specific task; however, I realize and agree that the forefoot would be providing some force against the stirrup during some phases of her riding.
Diane’s comment:
Ah, the power of reflecting on our thinking!
Diane’s comment:
Brittany has chosen to list all the start screen findings for each unit before moving into the screening task. While this is not ‘wrong’ per se, it is much faster in clinical practice to find findings in one unit, then note what happens to the chosen sites of impairments in the screening task, then find a unit driver for that screening task. Following this, quick tests are used to determine IF you need to even go into other units. It is a faster way to conduct and ISM finding drivers assessment.
Squat task
A squat task was chosen as Ms. C experienced her left sided sacroiliac joint pain after riding her horse; however, the pain did not present itself until the end of her riding session.
In order to complete the assessment as accurately as possible, her back was kept upright and elbows at her side in a roughly 120-degree angle to mimic holding onto the back of the horse.
The following assessment findings were observed in her squat task.
Functional Unit #1
Pelvis: right transverse plane rotation (TPR) worsens with depth of squat and left SIJ unlocks early in the squat (within the first 25% of the range)
Hips: left hip translates anteriorly relative to the acetabulum and is anteriorly translated relative to the right hip.
Diane’s comment & question:
In the standing start screen, it was noted that the left hip was anterior to the right but there is no notation that it was anteriorly translated relative to the left acetabulum. This finding seems to have appeared in the squat task itself. What is the difference between the anteriorly translated left hip (to the acetabulum) vs anteriorly positioned left to right hip and what is the significance of the translation finding?
Brittany’s response:
A hip that is sitting well within the acetabulum can still be anterior to the other side. For example, in this scenario for a right transverse plane rotation, when assessed in standing, the left hip is sitting in the acetabulum but is anterior to that of the right hip. The left hip is congruent to the right TPR of the pelvis and incongruent to the task of standing. However, this changes in the squat task. The left hip is now anteriorly translated to the left acetabulum, which means it is incongruent to the right TPR of the pelvis and incongruent to the squat task being assessed. As the left femoral head translates anterior relative to its acetabulum in the squat, the left hip should be assessed to see if it is a driver.
Thorax: 3rd thoracic ring further translates left and rotates right, 4th thoracic ring further translates right and rotates left. The 7th and 8th thoracic rings remain the same as the screening task (7th thoracic ring translated left and rotated right, 8th thoracic ring translated right and rotated left).
Lumbar spine: the 5th lumbar vertebra remains in right rotation
Diane’s question:
Regarding the L5, is this rotation relative to the coronal plane of the body or to the rotation of the sacrum? For example, L5 can appear to be rotated to the right but if the sacrum is more rotated right than the L5, if only L5 position is assessed in space, it can be found to be right rotated in space and yet left rotated relative to the sacrum.
Brittany’s response:
The 5th lumbar vertebrae was assessed in relation to the sacrum not the coronal plane of the body.
Diane’s comment:
A much more clinically relevant finding.
Driver for Functional Unit #1: Pelvis
Clinical reasoning: Correcting the pelvis corrected the left hip, 3rd and 4th thoracic rings and 7th and 8th thoracic rings. The 3rd and 4th thoracic ring correction corrected the 7th and 8th thoracic rings and provided a partial improvement of the pelvis (the L SIJ still unlocked but not until deeper into the squat). Video #1 in the skills acquisition section demonstrates how SIJ control is assessed with a thoracic ring correction. There was no change in the hip with the thoracic correction. Correcting the hip had no effect on the pelvis or thorax.
Diane’s comment & question:
Recently, quick unit screening tests of non-assessed units have been introduced to expedite the assessment. Did you do a quick screen of FU#2 with the FU#1 driver corrected in squat task to see if you even needed to assess FU#2? What was your clinical reasoning for even needing to assess FU#2?
Brittany’s response:
In order to expedite the assessment, a quick screen of FU#2 was completed with the FU#1 driver. For Ms. C, once I found it was her pelvis in FU#1 that was the primary driver, I assessed her head and neck rotation without any corrections made. I then corrected her pelvis and reassessed her head and neck rotation. Correcting the pelvis worsened the head and neck rotation, which made me realize that I had to go and assess FU#2.
I was also interested in assessing FU#2 secondary to the story bringing her in. When she fell off of her horse, she hit her head and lost consciousness and had broken ribs and a broken clavicle, so there has been significant impact and trauma to FU#2.
Diane’s comment:
Both are very valid reasons for moving into FU#2.
Functional Unit #2
Cranium: left intracranial torsion (ICT) worsens.
Thorax: no change observed in 2nd thoracic ring from the standing start screen (2nd thoracic ring was translated left and rotated right).
Cervical spine: the 6th cervical vertebrae further translates to the right, rotates to the left. The 2nd cervical vertebrae remained in a right translation, left rotation as found in the standing screen. C2 further translates left and rotates right during the squat task. C2 is part of the AA joint which is very critical for maintaining alignment of the head.
Shoulder girdle: no change in the shoulder girdle from the standing postural screen (remains downwardly rotated and anteriorly tipped). Right clavicle remains medially compressed.
Diane’s question:
In this squat task you have asked her to keep her ‘back upright’ and I assume her neck and head aligned with her thorax? Is there any system impairment that comes to mind when you see a left cranial torsion and C6 rotation increase during this task?
Brittany’s response:
During the squat task, her back was kept upright and neck and head aligned with thorax. A left cranial torsion and a C6 rotation that increases during the task can be a sign of a visceral system impairment.
Diane’s comment:
My mind immediately went to fascial!
Driver for Functional Unit #2
The cervical spine is the primary driver (priority segment is C6).
Clinical reasoning: Correcting the cranium had no impact on any of the findings. Correcting C6 corrected C2. Correcting C6 also corrected the cranium and the shoulder girdle and made the experience of the squat task feel much easier to Ms. C.
Priority between unit drivers
Finding drivers in a screening task guides the further assessment and treatment of the appropriate areas of the body, regardless of the location and phenotype of pain. A primary driver is an area of the body that, when corrected, or changed, fully corrects all other sites of impairment. A secondary driver is an area of the body that when corrected/changed, has no impact on the primary driver, but is partially corrected (improved) when the primary driver is corrected.
Ms. C’s primary driver is the cervical spine (C6 segment) and her secondary driver is the pelvis.
Clinical reasoning: Correcting the cervical spine (C6), partially corrected the pelvis (the left SIJ lost control later in the squat task), and correcting the pelvis had no impact on her cervical spine.
Further Analysis of Drivers
Further assessment of the individual driver includes tests for active mobility, passive mobility, active control and passive control, if appropriate. The outcome of this assessment helps to determine the underlying system impairments, and guides the treatment plan. During all mobility tests, analysis of vectors which impede, or influence, motion are analysed for location, direction of pull, length of pull, depth of pull. A vector can arise from any system (articular, neural, myofascial or visceral) and each system has a felt quality that helps to differentiate the vector and thus facilitate the treatment chosen for release.
System vectors can impact alignment, biomechanics and control of the body.
Active and passive listening during active and passive mobility tests are used to understand more about restrictive system vectors.
- Active Listening: listen and feel for the vector as the body encounters the first point of resistance while the patient actively moves their body through a task or range of motion
- Passive Listening #1: listen and feel for the first vector when passively moving a segment
- Passive Listening #2: release the correction and listen to where the vector is taking you, how strong is it, how long is it, does it stay outside in the musculoskeletal system or does it go into the visceral cavities of the body
Further Assessment of the Cervical Spine (C6)
Active Mobility: During dressage, Ms. C needs to be able to rotate her head in both directions as she moves throughout the course. For this reason, rotation of the neck was assessed. She had full mobility in a left cervical rotation, but had decreased right cervical rotation by ~25% range of motion.
Diane’s comment:
For clarity, Brittany is NOT finding a driver for a different screening task here. She has determined that the cervical spine (C6) is the driver for the squat task and is using head and neck rotation to determine if C6 has full active mobility (likely not if it’s a driver), passive mobility (maybe) and what vectors are impeding its function.
Diane’s question:
Did Active Listening direct you to a particular part of the cervical spine?
Brittany’s response:
Active listening took me to the lower part of the right cervical spine, as there was resistance when she got to the last 75% of the cervical range of motion.
Diane’s comment:
This finding is consistent with C6 being responsible for limiting right rotation (she is triangulating her findings to provide further support to her hypothesis).
Passive Mobility: With Ms. C in supine, the passive mobility of her cervical spine was tested, specifically the 6th cervical segment. See Video #2 in the skills acquisition section below for how this technique is done. It was a little bit harder to correct, but it was able to move.
Diane’s comment & question:
So here it is, I would suggest that C6 is compensating for something else in the unit. If this was an articular system impairment it wouldn’t be easy to correct in sitting and difficult in lying. It would be difficult in both. I’m curious as to why you chose to assess her passive mobility in supine when she rides a horse upright? Your findings may have changed in the supine position since strategies are task specific?
Brittany’s response:
On reflection, I don’t know why I did this in supine, I definitely should have done this in sitting.
An easy correction would typically be impacted by the neural system and a very stiff segment that is tough to correct could be impacted by the articular system. For Ms. C, a correction was possible, but took a little bit more effort than a simple correction impacted by the nervous system. This correction felt affected by the myofascial system.
Diane’s comment:
This is also how a fascial impairment feels. C6 was easy to correct in sitting – this finding negates an articular system impairment even if it was hard to correct in supine. Something is pulling more on C6 in supine than it does in sitting – this is a really interesting finding. What is different that attaches to C6 in sitting than in lying
Brittany’s response:
The supra pleural ligament attaches from the lower cervical segments to the pleura. She did have collapsed lungs, so this could all make sense that there’s a visceral restriction I didn’t realize.
Passive Listening #1: Correcting the 6th cervical segment was possible but felt difficult to do secondary to the right sided pull anterior to the vertebrae.
Passive Listening #2: Upon release of the correction, there was a medium length pull into the front of the right chest, outside the thorax.
Diane’s comment:
The location of pull, combined with your knowledge of anatomy, is so critical for hypothesis generation as to what is causing the vector and thus what to treat. While this could have been the supra pleural membrane, the finding of the pull being outside the thorax rules this hypothesis out and suggests the pull was from the fascial system.
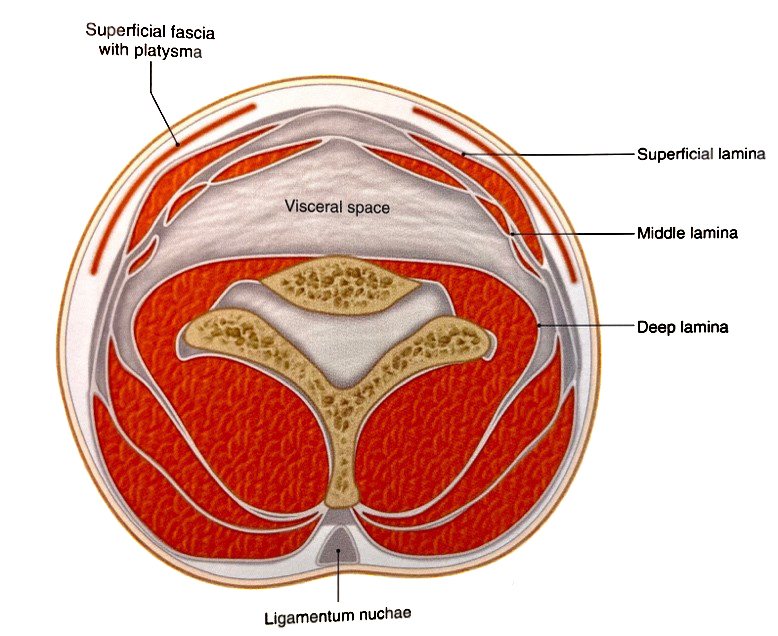
There are three lamina of the deep cervical fascia:
- Superficial lamina
- Middle lamina
- Deep lamina
Diane’s comment:
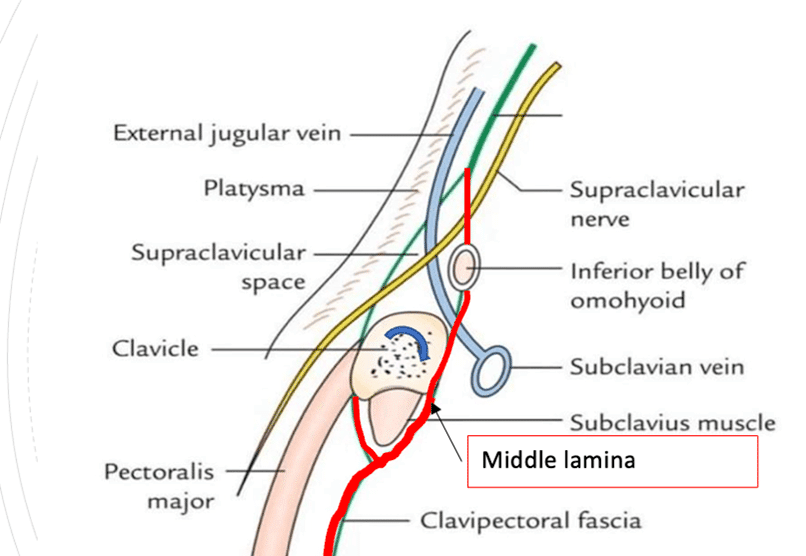
Which of the depicted structures below are in each lamina. Below you state that you felt the vector coming from the middle lamina but I see the middle lamina indicated in this illustration below. What muscles are contained in the middle lamina?
Brittany’s response:
The middle lamina contains the hyoid muscles, and goes posteriorly to encompass splenius and levator scapulae. It also contains the rhomboids and serratus posterior.
Upon releasing the correction of the 6th cervical segment for the passive listening technique #2, there was a medium length listening coming from the right side of the anterior portion of the neck. It was hypothesized that this was from the middle lamina of the deep cervical fascia.
Diane’s question:
Above you state that on release of the C6 correction there was a “medium length pull into the front of the right chest”. I’ve asked you to list the muscles that are contained in this lamina of the deep cervical fascia above. Now then, when the middle lamina reaches the clavicles does it go anterior or posterior to them and where does it go below the clavicles in the thorax region? This is highly relevant to her story and trauma.
Brittany’s response:
The middle lamina of the deep cervical fascia attaches posteriorly to the clavicle. It wraps around to the front of the clavicle to encompass the subclavius muscle. It then blends with the clavipectoral fascia inferiorly and remains outside the thorax, underneath the pectoralis major muscle.
Diane’s question:
Where does the middle lamina of the deep cervical fascia attach to the cranium (anterior and posterior)? Can you hypothesize here how the LICT/Lsphenoid may be responding to this vector – think about the pull through both the mandible and its impact on the temporal bones as well as the attachment to the temporals and occiput directly in your answer.
Brittany’s response:
The middle lamina of the deep cervical fascia goes superiorly and anteriorly to the hyoid muscle, and then attaches to the mandible. Posteriorly it envelops the splenius and levator scapulae muscles. It is through the attachment to the splenius capitus that it reaches the cranium via the lateral superior nuchal line of the occipital bone and the mastoid process of the temporal bone.
When the horse stepped onto Ms. C’s ribcage, there was trauma both on the left and right side of the upper thorax. In a left ICT, the left temporal bone is posteriorly rotated and the right temporal bone is anteriorly rotated. The sphenoid is also left rotated. The occiput will follow the left posterior rotation of the temporal bone. After the trauma to the thorax, the cervical fascia created a pull via the middle lamina posteriorly to the splenius muscle, which attaches to the mastoid process of the temporal bone. The right splenius capitus exerts pull which can create an anterior rotation of the right temporal bone, and consequently a posterior rotation of the left temporal bone, resulting in the left ICT.
Diane’s comment:
Nicely hypothesized!
Active Control: Active control was not tested during the first session as the vectors influencing the mobility of the cervical segment had yet to be released. When tested in a following session, Ms. C could maintain control with both a simple arm elevation task and when resistance was applied to both elevated arms.
Passive Control: Passive control was also not tested during the first session secondary to the presence of the vectors that had yet to be released and reassessed. When tested in a subsequent session, there was no loss of control in either the anterior or posterior translation tests.
Further Assessment of the Pelvis (SIJ)
Active Mobility: Decreased posterior rotation of the left innominate relative to the left side of the sacrum compared to the right
Diane’s question:
In the standing start screen, her pelvis was in a right TPR/IPT. This active mobility test is done in standing. Therefore, what was the relative starting position of the left innominate relative to the left side of the sacrum and where was the relative starting position of the left innominate relative to the right innominate? If the starting position is different, this could be an explanation for the asymmetry noted on this active test.
Brittany’s response:
In the original standing screen, her pelvis was in a right transverse plane rotation (TPR) and a right intra pelvic torsion (IPT). In a right IPT, the left innominate rotates anteriorly relative to the right innominate, the sacrum rotates to the right and the right innominate rotates posteriorly relative to the left innominate. Therefore, the left innominate was posteriorly rotated relative to the left side of the sacrum and the left innominate was anterior relative to the right innominate in the transverse plane.
Passive Mobility: Her pelvis was placed into a neutral TPR/IPT in supine to ensure both sides were symmetrical. If the passive mobility of the pelvis is assessed when there is an IPT present, the findings may not be accurate as you can get different amplitudes of movement between the right and left sides. The upper pole of the left SIJ was restricted, whereas the middle and lower poles of the SIJ had full mobility.
- Passive Listening: This technique was done with the patient lying supine and an anteroposterior load was applied in the plane of the joint. After releasing the anteroposterior load, a pull was felt to the left superficial fibres of multifidus (sMF). Those fibres were released with the use of dry needling and the mobility test repeated.
Diane’s question:
So what system impairment is this?
Brittany’s response:
This is a neural system impairment.
Diane’s question:
What does the evidence tell us about muscle recruitment response of the back extensors to acute trauma? What muscle would you want to assess given the over-activation of both the sMF and longissimus on the left side? Did you trace the fascicle of the longissimus to see which thoracic ring it was in relationship to? I would be curious to know if it was TR4 – why?
Brittany’s response:
During acute trauma or episode of back pain, the deep fibres of multifidus become inhibited and the erector spinae are then used to help stabilize and are often, but not always, over recruited. Given the overactivation of both the superficial fibres of multifidus and longissimus on the left side, I would want to assess the deep fibres of multifidus to see if they are able to turn on and recruit, or if this person is solely using their superficial muscles.
Longissimus was traced up to the thorax and the fascicle did attach up into TR4. This is important because a tight fascicle of longissimus up to TR4 can contribute to a forward flexion movement of the 4th lumbar vertebrae, and thus have an impact on the findings I was seeing in her lumbar spine.
Diane’s comment:
The TR4 is right translated/left rotated so if this vector is causing the ring to rotate it would be on the left side. TR4 is incongruently rotated to her pelvis in both standing and the squat so when she sits on her horse, she is sitting rotated between her TR4 and pelvis. Not a great posture for your low back when riding a horse!
Diane’s question:
In the start screen, it was noted that L5 was right rotated, did you note where L4 was perchance?
Brittany’s response:
L4 was in left rotation which means that L5 and the pelvis were both in a right transverse plane rotation, whereas L4 was left rotated. I should have assessed this further, because as you said sitting rotated between her TR4 and pelvis could certainly contribute to her story and the pain she was experiencing.
Diane’s comment:
Indeed this could have been a key contributor to her nociception since incongruent rotation between the lumbar segments is poorly tolerated by the lumbar region. However, the cause of this may be the strategy she is using to stabilize her left SIJ (superficial multifidus and left longissimus) and since you are treating this, the alignment of L4 and L5 may have automatically become congruent.
Active Control: In a squat task, her left innominate rotates anteriorly in relation to the left side of the sacrum early in the task, this is an unlocking sacroiliac joint. The right side of the sacrum remained nutated in relation to the innominate. This active control test was done in a subsequent session once the vectors were released.
Diane’s question:
According to Snijders and Vleeming (1993) there are two mechanisms that work together to provide control of motion for the SIJ – the form and force closure mechanisms. The force closure mechanism is influenced by motor control strategies. Can you provide a definition of these two mechanisms (form and force closure) and then describe which position of the SIJ enhances form closure and why, and which muscles provide force closure.
Brittany’s response:
The sacroiliac joint (SIJ) has both form and force closure mechanisms. The form closure mechanism relies on the shape of the bones and joints as well as the ligaments of the pelvis to provide closure. The articular surfaces of the SIJ interlock together after skeletal maturity, providing some control of shear. The study by Snijders and Vleeming (1993) shows that articular surfaces with depressions and ridges, provide a higher coefficient of friction, thus protecting the joint from shearing. The pelvis is also anatomically designed in a wedge shape, further supporting control of the joint.
Nutation and counternutation both occur at the SIJ. It is hypothesized that during nutation, the sacral promontory moves anterior in the pelvis (in a nodding motion) and the joint surface of the sacrum glides inferoposteriorly relative to the innominate. During counternutation, the sacral promontory moves posterior and the joint surface of the sacrum glides anterosuperiorly relative to the innominate (Lee, D., 2011).
Diane’s comments:
These biomechanics have only been validated in the open chain position for nutation of the sacrum (Hungerford et al 2003 PhD thesis).
Brittany continued:
Nutation enhances the form closure mechanism of the sacroiliac joint and the resistance to sacral shearing is provided by the coefficient of friction mentioned, as well as the wedge shape of the sacrum between the two innominates and the interlocking surfaces of the joint. The ligaments of the pelvis (interosseous, sacrospinous and sacrotuberous ligaments) tighten in nutation thus adding further compression and form closure.
Force closure pertains to the forces produced by structures around the joint that create a perpendicular force, compression, or “closure” and include the muscles and thoracolumbar fascia. The muscles that contribute to the force closure mechanism include the hamstring muscle group, specifically the long head of biceps femoris as it attaches to the sacrotuberous ligament, the pelvic floor, deep sacral multifidus, the lower fibres of tranvsersus abdominis, the low anterior part of the internal oblique, longissimus, the glutes and piriformis.
Passive Control: Similar to active control, the passive control was also tested in a subsequent session after releasing the appropriate vectors. The SIJ was placed in a closed pack position and there was no loss of control observed upon testing.
Diane’s question:
The close-packed position is a Nordic orthopaedic manual therapy term defined as….:
Brittany’s response:
The term closed-pack position refers to when the joint surfaces are compressed, the ligaments and joint capsule have maximum tension and the surfaces of the joint cannot be separated by external forces (Magee 2014).
Diane’s question:
What is the closed pack position for the SIJ? (i.e. where is the innominate relative to the sacrum and the sacrum relative to the innominate)
Brittany’s response:
The closed pack position of the SIJ is when the sacrum is nutated and the innominate is posteriorly rotated in relation to the sacrum.
Diane’s question:
OK so now we understand what ‘placing the pelvis in the close pack position means’. What did you then do to determine “there was no loss of control observed upon testing”.
Brittany’s response:
When testing the passive control of the pelvis, the client is placed in supine and one hand of the therapist nutates the sacrum, while the other hand posteriorly rotates the innominate in order to the place the pelvis in the closed pack position. In this position, the therapist then performs an anterior-posterior glide, in which there should be no movement, which was the case for Ms. C. If movement is present, it indicates a loss of integrity of the major ligaments that stabilize the pelvis (sacrotuberous, sacrospinous and interosseous ligaments).
Diane’s comment:
This test can be falsely positive IF there is inhibition or atrophy of the sacral fibres of deep multifidus. Sometimes we have to train to wake up and build capacity in this muscle before this test is determined to be truly positive.
Ms. C was very interested in learning more about her pelvic floor and the bladder, so we incorporated the use of real time ultrasound in order to educate Ms. C about the pelvic floor muscles, even though the pelvic floor muscles did not require further assessment secondary to the clinical findings.
Diane’s question:
Is this assessment then to address her cognitive belief or yours?
Brittany’s response:
I used the real time ultrasound to help with Ms. C’s cognitive belief, as one of her concerns was her bladder. I also find that the ultrasound is a great educational tool to teach the client about their pelvic floor.
There were no tight pelvic floor muscles on either side of the pelvis, a finding which correlates with the SIJ passive mobility finding, and Ms. C had good ability to recruit her muscles when given the proper cues.
However, because the left SIJ control was only partially restored with correction of the primary driver (cervical – C6) further assessment of the force closure mechanism and motor control for the pelvis was indicated. The pelvic floor assessment suggests that the impairment is in another muscle group. This assessment follows this section below.
Nerve testing of the lower extremity was normal and did not show any signs of potential nerve damage to the pelvic floor muscles.
Motor Control Analysis of the Pelvis and Impact of Primary Driver Correction (C6)
In an active bent leg raise test, the left leg was heavier to lift than the right. When asked to lift the left leg with a pelvic floor cue, her low fibres of transversus abdominis had a symmetrical activation; however, there was no activation of the deep fibres of multifidus on the left side. When cued to activate her deep fibres of multifidus, the left leg felt lighter and the patient had the best experience with this. Her pelvic floor muscles and low fibres of TA did not activate with the dMF cue, and she required a combined dMF, pelvic floor and tranvsersus abdominis cue.
When correcting C6, her deep fibres of multifidus were able to turn on easier; however, there was still poor control (unlocking) of the left sacroiliac joint, although this occurred later in the squat task. This suggests that we will need to train the left sacral fibres of multifidus.
Diane’s question:
So there is a relationship between the alignment of C6 and the motor control strategy for left SIJ control in that the loss of control of the left SIJ occurred later in the squat task. Can you explain what you mean by ‘we have to train the deep fibres of multifidus’. Do you need to restore motor control, build strength/endurance, build bulk – all of this is training – can you be more specific.
Brittany’s response:
In order to train the deep fibres of the left multifidus, we need to start with motor control training to wake up the muscle, as correcting the primary driver (C6) improved the loss of control of the left SIJ; however, it didn’t fully correct it as the loss of control appeared later in the squat. We can then build capacity through strength and endurance training.
Hypothesis
Ms. C was likely experiencing pain in her left sacroiliac joint after the cervical fascia was affected from the trauma of the horse stepping on her neck and thorax. Although many layers of cervicothoracic fascia were likely impacted due to the severe nature of the trauma, the middle lamina of the deep fascial layer of the neck appeared to be impairing the alignment and mobility of the 6th cervical segment, which was found to be in relationship to the control of the left SIJ.
The middle lamina includes the following muscles: hyoid muscles, splenii, levator scapulae, rhomboids and serratus posterior and connects laterally to the posterior aspect of the clavicle (Stecco, 2015). The attachment to the posterior aspect of the clavicle and the tension that was observed within the middle lamina of the cervical fascia, resulted in a medial compression of the right clavicle.
The middle lamina of the deep cervical fascia continues to become the clavipectoral fascia laterally. The clavipectoral fascia extends from the clavicle and continues inferiorly with the fascia of the internal oblique muscle. The right side of the internal oblique fascia meets with that of the left side to help form the rectus sheath, containing the rectus abdominus muscle, therefore affecting both the left and right sides of the body. The fascia of the internal oblique also inserts posteriorly to the anterior aspect of the thoracolumbar fascia (Stecco, 2015).
When further assessing Ms. C’s pelvis, the left upper pole of the sacroiliac joint was restricted and the passive listening led to the left superficial multifidus and longissimus. The longissimus is part of the erector spinae group which shares an attachment to the thoracolumbar fascia.
After falling off the horse and getting stepped on, it is hypothesized that the injuries to the cervical fascia caused an extension of restriction down to the lower abdomen through the internal oblique fascia and to the thoracolumbar fascia. This ‘twist’ in the fascia of the trunk may, in part, be in relationship to the loss of left SIJ control, although restoring C6 alignment (see treatment below) did not completely restore left SIJ control. There were factors directly related to her secondary driver (the pelvis) that needed addressing and these included:
- Atrophy of the left deep sacral fibres of multifidus
- Over-activation of the left superficial fibres of multifidus (compressing the superior pole of the left SIJ)
- Over-activation of longissiumus (extending to L4 and by extension perhaps to the sacrum)
Ms. C also experienced a loss of sensation of a need to void after the fall from the horse. We began Ms. C on a scheduled voiding routine after reviewing her bladder diary that she filled out.
Diane’s question:
What were the findings of the bladder diary that required change?
Brittany’s response:
Her bladder diary showed that she was drinking large quantities of water throughout the day, which we changed to sipping on the water in order to help the tissues absorb the fluid more. She was also holding her bladder for sometimes over four hours at a time, and we made sure she was going to the bathroom at least every four hours, even if there was no signal to go at that time.
Although we did not work specifically on the pelvic floor muscles, her bladder slowly began to improve and she was beginning to regain the sensation of feeling when the bladder is filling towards the end of the treatment sessions. It is hypothesized that working on the fascia of the cervical region and subsequently into her back, may have indirectly improved the mobility of the pelvic fascia surrounding the bladder.
Treatment
Treatment sessions incorporate all dimensions of a biopsychosocial approach, the amount of each dimension varies between clients depending on the assessment findings. For some this treatment may begin with education or working into an emotional or sensorial experience before even touching the body. For Ms. C, we began with education about the relevant body areas and their function and then followed up with the RACM acronym, which stands for release, align, connect and move.
Release
- Cervical region (C6): release with awareness for the right middle lamina of the deep cervical fascia; home exercise program (HEP) was to continue the release with awareness at home for 30 seconds, 3x/daily
Diane’s question:
Many clinicians believe fascia to be a ‘passive’ tissue. Release with awareness works within the neural system for the first part of the technique. How does release with awareness change tension/tone of the middle lamina of the cervical fascia? Are you working on the connective tissue or something else? Given her severe trauma I’m sure things were ‘tight’ but here you have first chosen a technique that is not totally appropriate for ‘tight’ structures but rather ‘toned structures’.
Brittany’s response:
Release with awareness works within the neural system and is done as follows:
- Position the tissue to provide the most amount of shortening of the hypertonic tissue
- Wait for the reduction in tone to the tissue
- Further release the tone in the muscle by cueing the patient to “soften” or “let go” of the area
- Once the tissue has decreased in tonicity, its taken into its maximum passive length
This is often done with muscular tissues, as fascia is believed to be a passive tissue. However, according to Schleip et al. (2005), there is some evidence to show that fascia may be able to actively contract in a similar manner to muscular tissue, thereby influencing the dynamics of the musculoskeletal system. This was studied after contractile cells were first found in fascia. Although this may require further studies, the release with awareness technique was found to be clinically effective for releasing the middle lamina of the deep cervical fascia with this client.
Diane’s comment:
And since 2005, we have way more evidence to suggest that fascia is hugely neural and important for proprioception.
- Pelvis: release left longissimus vector using release with awareness technique; release left superficial lumbar multifidus with dry needling; Home exercise practice (HEP) was to release left longissimus with a massage ball
Align
- Cervical region (C6): imagine a fish hook gently creating space in the between the 6th and 7th cervical vertebrae
Connect
- Tape the posterior pelvis using leukotape (transversely across the posterior pelvis to provide force closure for control as left side of pelvis was still losing control after releasing relevant muscles
- Reviewed left sacral multifidus activation. Best cue was to “imagine a guy wire from one back dimple (PSIS) to the other. Slowly try and shorten that wire.” HEP: sacral multifidus 30 reps x 3 sets (hold 3 seconds) daily. See Video #3 in the skills acquisition section for a demonstration of how this is taught.
Move
- Practice integrating the align cue for the cervical spine when sitting on the horse or when sitting on a chair at home
- It was too early in Ms. C’s treatment to teach the connect cue of the pelvis with a move cue, but see section below on follow up treatment sessions for more detail.
Follow Up Treatment Sessions
Follow up sessions were initially scheduled at once per week. Focus was on continued release work of the cervical fascia and muscles around the lower cervical spine and pelvis, along with the integration of the align cues into her day-to-day routines, and ultimately while sitting on the horse.
Diane’s question:
Below there is no focus on C6, which initially was her primary driver. Had the pelvis now become the primary driver after release of the cervicothoracic fascia?
Brittany's response:
After releasing the cervicothoracic fascia in the earlier sessions, the cervical region was no longer the primary driver, and the treatment focused on the pelvis as it was now the primary driver.
Her continued sessions then began to focus on motor control of her pelvis and progressing her through the following stages:
Stage 1. We worked on activating multifidus without over activation of the superficial erector spinae muscles. This was initiated in a 4-pt (hands and knees) position, and slowly added into other static positions such as sitting and standing.
Stage 2. This stage required that we maintain the static control of the pelvis but add load and coordination of distal segments. For Ms. C, we added the bilateral arm elevation in standing and sitting and progressed to holding weights in her hands.
Stage 3. This stage has three different levels working on greater complexity of movement. We began to integrate the multifidus connect cue while moving the pelvis into different planes. Ms. C started in her squat position and had to shift her weight from one leg to the other, while maintaining control of her pelvis. We then progressed by adding arm elevation to the weight shift task, adding weights to her hands and integrating a single leg task within the weight shift movement where Ms. C had to lift the alternate foot off the ground while keeping her arm elevated and weight on one leg.
Summary
Ms. C was able to get to the point that she was pain free after her horseback riding sessions, and was able to integrate the control cues into her daily riding practices. She began to increase her daily activity levels and is now comfortable managing on her own. She was very appreciative of taking the time to learn what was actually causing her pain, and was so motivated with learning about the body that she now integrates some of these postural cues when coaching her equestrian students.
References
Butler, D. S. (2000). The sensitive nervous system. Noigroup Publications.
Hasegawa, J., Tateda, M., Hidaka, H., Sagai, S., Nakanome, A., Katagiri, K., … & Kobayashi, T. (2007). Retropharyngeal abscess complicated with torticollis: case report and review of the literature. The Tohoku journal of experimental medicine, 213(1), 99-104. from: https://www.researchgate.net/figure/Schematic-diagram-of-deep-neck-fascia-The-cross-section-of-the-neck-at-the-thyroid-The_fig6_6054479
Lee, D. (2011). The pelvic girdle. Churchill Livingstone.
Magee, D. J. (2014). Orthopedic physical assessment. Saunders Elsevier.
Schleip, R., Klingler, W., & Lehmann-Horn, F. (2005). Active fascial contractility: fascia may be able to contract in a smooth muscle-like manner and thereby influence musculoskeletal dynamics. Medical hypotheses, 65(2), 273-277.
Stecco, C. (2015). Functional atlas of the Human Fascial System. Churchill Livingstone.
St. George, L., Thetford, C., Clayton, H. M., & Hobbs, S. J. (2022). An exploration of
stakeholder perceptions to inform the development of an evidence-based classification system in para dressage. Journal of Sports Sciences, 40(4), 459-469.
Taylor, B. K., & Corder, G. (2014). Endogenous analgesia, dependence, and latent pain sensitization. Behavioral Neurobiology of Chronic Pain, 283-325.
Skills Demonstration
Clinical Mentorship in the Integrated Systems Model
Join Diane, and her team of highly skilled assistants, on this mentorship journey and immerse yourself in a series of education opportunities that will improve your clinical efficacy for treating the whole person using the updated Integrated Systems Model.
We will come together for 3 sessions of 4 (4.5) days over a period of 6-8 months with lots of practical/clinical time to focus on acquiring the skills and clinical reasoning to put the ISM model into practice. Hours of online lecture and reading material and 12 hours of in-person lecture are...
More Info

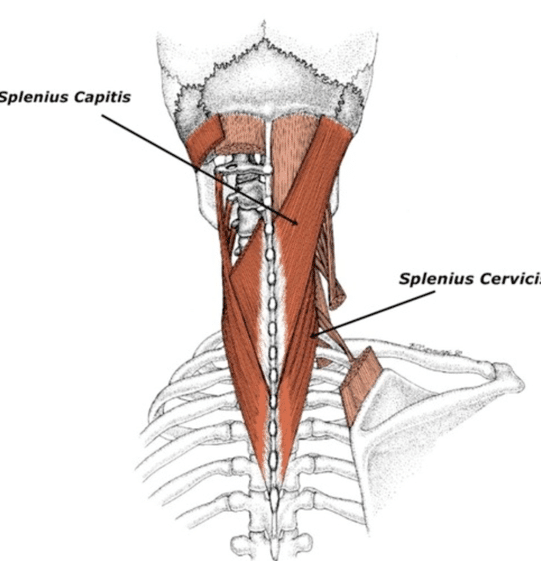 The middle lamina of the deep cervical fascia goes superiorly and anteriorly to the hyoid muscle, and then attaches to the mandible. Posteriorly it envelops the splenius and levator scapulae muscles. It is through the attachment to the splenius capitus that it reaches the cranium via the lateral superior nuchal line of the occipital bone and the mastoid process of the temporal bone.
The middle lamina of the deep cervical fascia goes superiorly and anteriorly to the hyoid muscle, and then attaches to the mandible. Posteriorly it envelops the splenius and levator scapulae muscles. It is through the attachment to the splenius capitus that it reaches the cranium via the lateral superior nuchal line of the occipital bone and the mastoid process of the temporal bone.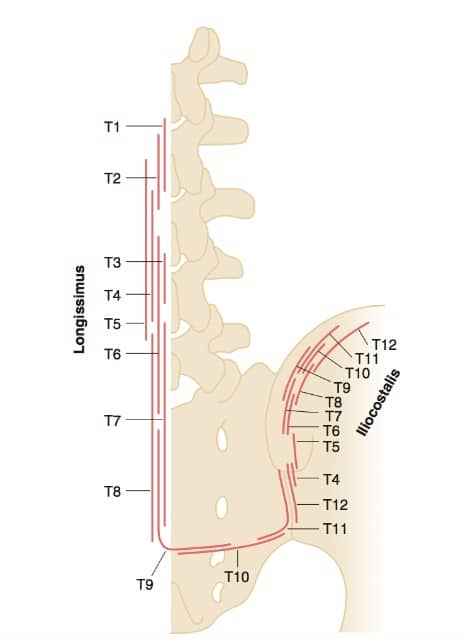 During acute trauma or episode of back pain, the deep fibres of multifidus become inhibited and the erector spinae are then used to help stabilize and are often, but not always, over recruited. Given the overactivation of both the superficial fibres of multifidus and longissimus on the left side, I would want to assess the deep fibres of multifidus to see if they are able to turn on and recruit, or if this person is solely using their superficial muscles.
During acute trauma or episode of back pain, the deep fibres of multifidus become inhibited and the erector spinae are then used to help stabilize and are often, but not always, over recruited. Given the overactivation of both the superficial fibres of multifidus and longissimus on the left side, I would want to assess the deep fibres of multifidus to see if they are able to turn on and recruit, or if this person is solely using their superficial muscles.

